Tuesday Poster Session
Category: Stomach and Spleen
P6398 - Oozing Hemorrhagic Gastritis: A Presentation of AA Amyloidosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Michael Tran, MD (he/him/his)
Ochsner LSU Health
Shreveport, LA
Presenting Author(s)
Michael Tran, MD1, Sarav Daid, MD2, Qiang Cai, MD, PhD, MACG3
1Ochsner LSU Health, Shreveport, LA; 2LSU Health Shreveport, Shreveport, LA; 3LSU Health Sciences Center - SHREVEPORT, LA, Shreveport, LA
Introduction: AA (Amyloid A) amyloidosis is due to other illnesses like chronic inflammatory disease or chronic infection. Incidence rate is 2 cases per million people per year and is rare in the United States compared to AL (amyloid light chain) amyloidosis. AA amyloidosis can cause nonspecific subtle symptoms like weight loss, diarrhea, and fatigue. It can also cause anemia of chronic disease due to amyloid deposition within certain organs. We present a case of anemia due to hemorrhagic gastritis incidentally found to be due to AA amyloidosis.
Case Description/
Methods: 43-year-old male with past medical history of end stage renal disease, congestive heart failure who presented to the hospital for encephalopathy. Hemoglobin at admission was 5.8. CTA (computed tomography angiography) was completed without signs of bleeding. Transfusion completed. He eventually developed sepsis, seizures, and pulmonary embolism. Anticoagulation was initiated. He later pulled out his NG (nasogastric tube) with blood clots seen. EGD (esophagogastroduodenoscopy) was completed for upper gastrointestinal bleeding. Blood was seen in the proximal stomach. Slight touch of mucosa caused oozing. No obvious source of bleeding seen, but 2 clips were placed at the area of bleeding with no improvement. It was determined to be hemorrhagic gastritis and to start pantoprazole twice a day. Due to need for anticoagulation, another EGD was completed 1 week later. Same findings seen and recommendation of risk vs benefit for anticoagulation and to continue pantoprazole. Patient eventually self improved and had repeat EGD outpatient. Hemorrhagic gastritis had mildly improved and gastric biopsies were taken at this time. Pathology consistent with AA amyloidosis. He was referred to hematology oncology (H/O) who did a bone marrow biopsy showing amyloid deposition. Workup was negative for myeloma. He currently has been referred to rheumatology for further assessment.
Discussion: AA amyloidosis is controlled by treating the underlying condition. A patient without any chronic inflammatory disease or infection this condition would not be expected. Hemorrhagic gastritis from AA amyloidosis is due to amyloid deposition weakening the mucosa and blood vessels. This case emphasizes the importance of gastric biopsies in patients with hemorrhagic gastritis to rule out amyloidosis, despite the concern of worsening bleeding, and to think of amyloidosis as a differential for hemorrhagic gastritis. Once confirmed further workup with H/O and rheumatology is necessary.
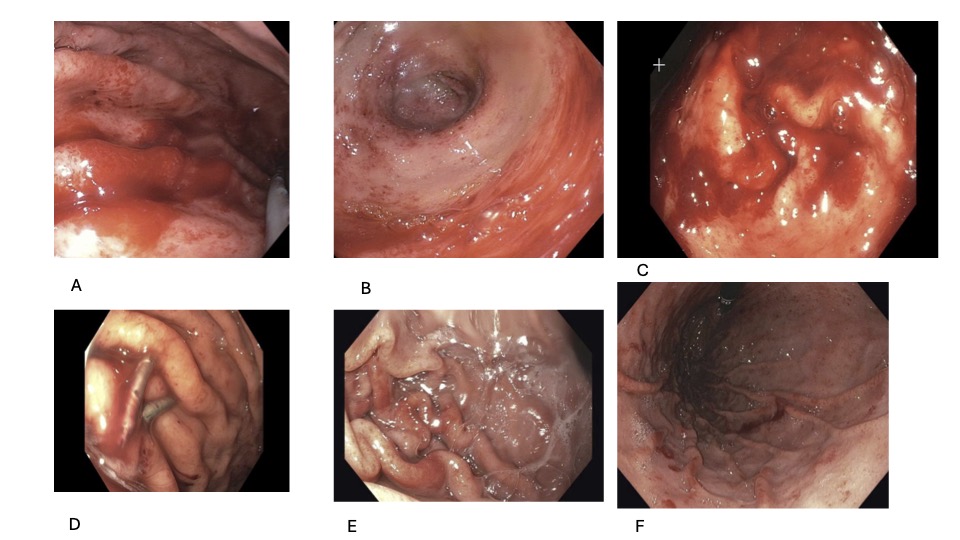
Figure: A. Initial EGD body of stomach
B. Initial EGD antrum
C. Hemorrhagic gastritis
D. Clips placed for hemostasis
E. Repeat EGD outpatient with improvement
F. Repeat EGD outpatient retroflexion
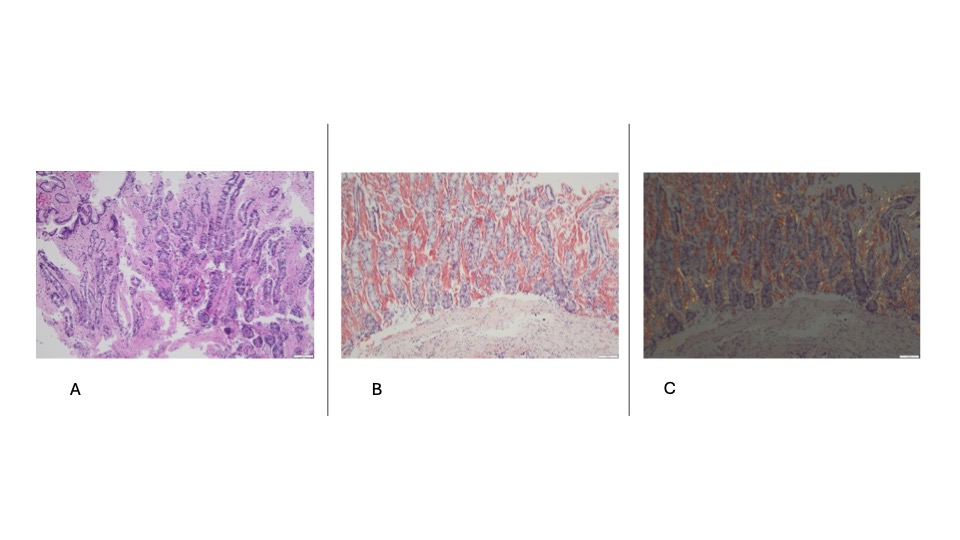
Figure: A. Congo Red 10x H&E AA amyloidosis
B. Congo Red 10x AA amyloidosis
C. Congo Red 10x polarized AA amyloidosis
Disclosures:
Michael Tran indicated no relevant financial relationships.
Sarav Daid indicated no relevant financial relationships.
Qiang Cai indicated no relevant financial relationships.
Michael Tran, MD1, Sarav Daid, MD2, Qiang Cai, MD, PhD, MACG3. P6398 - Oozing Hemorrhagic Gastritis: A Presentation of AA Amyloidosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ochsner LSU Health, Shreveport, LA; 2LSU Health Shreveport, Shreveport, LA; 3LSU Health Sciences Center - SHREVEPORT, LA, Shreveport, LA
Introduction: AA (Amyloid A) amyloidosis is due to other illnesses like chronic inflammatory disease or chronic infection. Incidence rate is 2 cases per million people per year and is rare in the United States compared to AL (amyloid light chain) amyloidosis. AA amyloidosis can cause nonspecific subtle symptoms like weight loss, diarrhea, and fatigue. It can also cause anemia of chronic disease due to amyloid deposition within certain organs. We present a case of anemia due to hemorrhagic gastritis incidentally found to be due to AA amyloidosis.
Case Description/
Methods: 43-year-old male with past medical history of end stage renal disease, congestive heart failure who presented to the hospital for encephalopathy. Hemoglobin at admission was 5.8. CTA (computed tomography angiography) was completed without signs of bleeding. Transfusion completed. He eventually developed sepsis, seizures, and pulmonary embolism. Anticoagulation was initiated. He later pulled out his NG (nasogastric tube) with blood clots seen. EGD (esophagogastroduodenoscopy) was completed for upper gastrointestinal bleeding. Blood was seen in the proximal stomach. Slight touch of mucosa caused oozing. No obvious source of bleeding seen, but 2 clips were placed at the area of bleeding with no improvement. It was determined to be hemorrhagic gastritis and to start pantoprazole twice a day. Due to need for anticoagulation, another EGD was completed 1 week later. Same findings seen and recommendation of risk vs benefit for anticoagulation and to continue pantoprazole. Patient eventually self improved and had repeat EGD outpatient. Hemorrhagic gastritis had mildly improved and gastric biopsies were taken at this time. Pathology consistent with AA amyloidosis. He was referred to hematology oncology (H/O) who did a bone marrow biopsy showing amyloid deposition. Workup was negative for myeloma. He currently has been referred to rheumatology for further assessment.
Discussion: AA amyloidosis is controlled by treating the underlying condition. A patient without any chronic inflammatory disease or infection this condition would not be expected. Hemorrhagic gastritis from AA amyloidosis is due to amyloid deposition weakening the mucosa and blood vessels. This case emphasizes the importance of gastric biopsies in patients with hemorrhagic gastritis to rule out amyloidosis, despite the concern of worsening bleeding, and to think of amyloidosis as a differential for hemorrhagic gastritis. Once confirmed further workup with H/O and rheumatology is necessary.
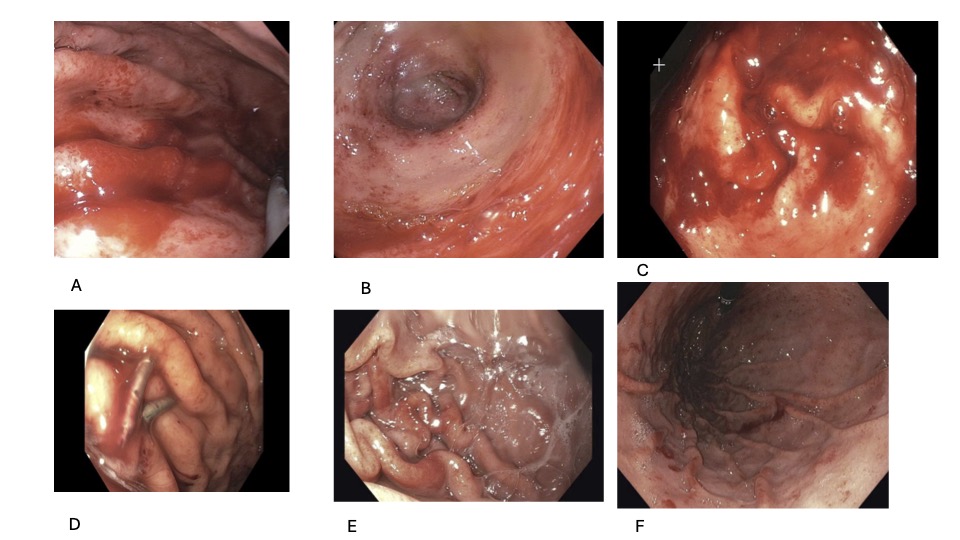
Figure: A. Initial EGD body of stomach
B. Initial EGD antrum
C. Hemorrhagic gastritis
D. Clips placed for hemostasis
E. Repeat EGD outpatient with improvement
F. Repeat EGD outpatient retroflexion
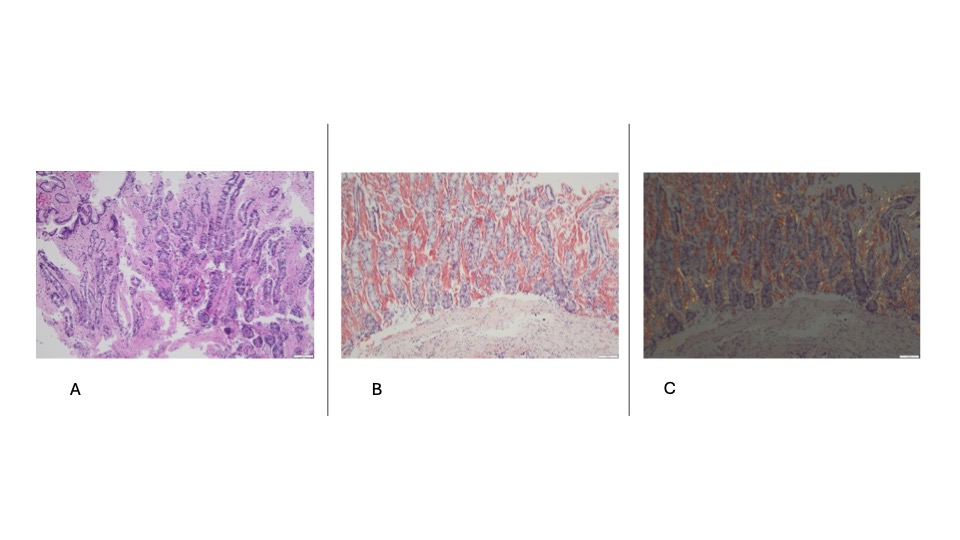
Figure: A. Congo Red 10x H&E AA amyloidosis
B. Congo Red 10x AA amyloidosis
C. Congo Red 10x polarized AA amyloidosis
Disclosures:
Michael Tran indicated no relevant financial relationships.
Sarav Daid indicated no relevant financial relationships.
Qiang Cai indicated no relevant financial relationships.
Michael Tran, MD1, Sarav Daid, MD2, Qiang Cai, MD, PhD, MACG3. P6398 - Oozing Hemorrhagic Gastritis: A Presentation of AA Amyloidosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
