Tuesday Poster Session
Category: Stomach and Spleen
Incidentally Detected <i>H. pylori</i>-Negative, t(11;18)-Negative Gastric MALT Lymphoma With Complete Response to Radiation
P6394 - Incidentally Detected H. pylori-Negative, t(11;18)-Negative Gastric MALT Lymphoma With Complete Response to Radiation
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anveet Janwadkar, MD
Tulane School of Medicine
New Orleans, LA
Presenting Author(s)
Anveet Janwadkar, MD1, Aishwarya Gatiganti, MD1, Naseeruddin Naseem, MD1, Yucel Aydin, MD2, Leela Nayak, MD3
1Tulane School of Medicine, New Orleans, LA; 2Tulane University, New Orleans, LA; 3VA Southeast Louisiana Healthcare, New Orleans, LA
Introduction: Gastric mucosa-associated lymphoid tissue (MALT) lymphoma is typically associated with Helicobacter pylori infection and frequently regresses with eradication therapy. However, H. pylori-negative and t(11;18)-negative MALT lymphomas are uncommon, raising questions regarding optimal management and prognosis in this molecularly distinct subset.
Case Description/
Methods: A 74-year-old man with a history of Barrett’s esophagus on proton pump inhibitor therapy underwent surveillance esophagogastroduodenoscopy (EGD). He denied dyspepsia, weight loss, or constitutional symptoms. Endoscopy revealed patchy mucosal abnormalities in the gastric body. Biopsies demonstrated extranodal marginal zone B-cell lymphoma of MALT type. Immunohistochemistry was negative for H. pylori and fluorescence in situ hybridization (FISH) testing showed no evidence of the t(11;18)(q21;q21)/BIRC3-MALT1 translocation. Staging CT imaging revealed no nodal or systemic involvement (stage IE). The patient was referred to hematology and treated with involved-site radiation therapy (ISRT), receiving 30 Gy in 20 fractions. He remained asymptomatic post-treatment. Follow-up EGDs at 6 and 24 months demonstrated endoscopic and histologic remission, with no clonal IgH rearrangement detected on molecular testing of surveillance biopsies.
Discussion: This case illustrates a rare presentation of gastric MALT lymphoma in an H. pylori-negative, t(11;18)-negative patient—highlighting the importance of biopsy in endoscopic abnormalities, even in asymptomatic individuals. In the absence of H. pylori or translocation-driven lymphomagenesis, localized disease can still respond favorably to ISRT. Though the prognosis of H. pylori-negative MALT lymphoma is less well defined, radiation therapy remains a highly effective modality in early-stage disease. As noted in the HELYX II trial, there were excellent outcomes showing complete eradication of MALT lymphoma in H. pylori-negative patients with 24–30 Gy radiotherapy. While surveillance intervals aren’t standardized in current literature, most guidelines are recommending endoscopic monitoring every 3–6 months for two years, then every 6–12 months, with long-term follow-up due to late relapse risk. This case reinforces the role of personalized management based on molecular and staging data.
References
ClinicalTrialsgps. Helicobacter – Lymphoma – Radiation Part I: Eradication, Part II: Radiation. https://www.clinicaltrialsgps.com/search-clinical-trials/trial-1100/. Published 2011. Accessed June 1, 2025.
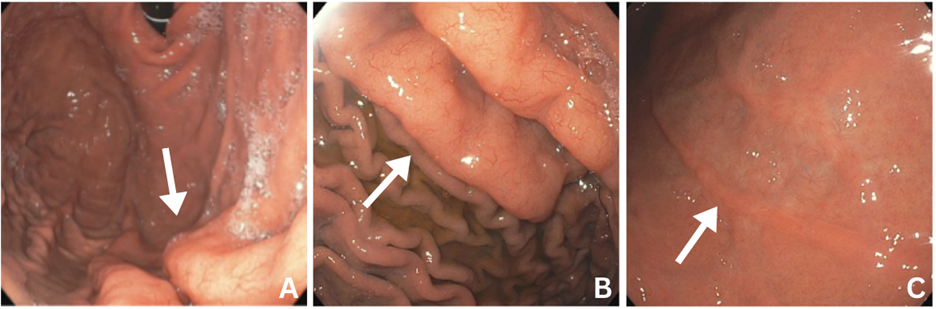
Figure: A: Initial findings showing abnormal folds (white arrow) in the gastric fundus and proximal body of the greater curvature where biopsy findings showed MALT lymphoma
B: 1-month follow-up showing persistence of abnormal folds (white arrow) in the area with biopsy-proven MALT lymphoma
C: 8-month follow-up after completion of radiation therapy showing the resolution and scarring of the previous folds (white arrow)
Disclosures:
Anveet Janwadkar indicated no relevant financial relationships.
Aishwarya Gatiganti indicated no relevant financial relationships.
Naseeruddin Naseem indicated no relevant financial relationships.
Yucel Aydin indicated no relevant financial relationships.
Leela Nayak indicated no relevant financial relationships.
Anveet Janwadkar, MD1, Aishwarya Gatiganti, MD1, Naseeruddin Naseem, MD1, Yucel Aydin, MD2, Leela Nayak, MD3. P6394 - Incidentally Detected <i>H. pylori</i>-Negative, t(11;18)-Negative Gastric MALT Lymphoma With Complete Response to Radiation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Tulane School of Medicine, New Orleans, LA; 2Tulane University, New Orleans, LA; 3VA Southeast Louisiana Healthcare, New Orleans, LA
Introduction: Gastric mucosa-associated lymphoid tissue (MALT) lymphoma is typically associated with Helicobacter pylori infection and frequently regresses with eradication therapy. However, H. pylori-negative and t(11;18)-negative MALT lymphomas are uncommon, raising questions regarding optimal management and prognosis in this molecularly distinct subset.
Case Description/
Methods: A 74-year-old man with a history of Barrett’s esophagus on proton pump inhibitor therapy underwent surveillance esophagogastroduodenoscopy (EGD). He denied dyspepsia, weight loss, or constitutional symptoms. Endoscopy revealed patchy mucosal abnormalities in the gastric body. Biopsies demonstrated extranodal marginal zone B-cell lymphoma of MALT type. Immunohistochemistry was negative for H. pylori and fluorescence in situ hybridization (FISH) testing showed no evidence of the t(11;18)(q21;q21)/BIRC3-MALT1 translocation. Staging CT imaging revealed no nodal or systemic involvement (stage IE). The patient was referred to hematology and treated with involved-site radiation therapy (ISRT), receiving 30 Gy in 20 fractions. He remained asymptomatic post-treatment. Follow-up EGDs at 6 and 24 months demonstrated endoscopic and histologic remission, with no clonal IgH rearrangement detected on molecular testing of surveillance biopsies.
Discussion: This case illustrates a rare presentation of gastric MALT lymphoma in an H. pylori-negative, t(11;18)-negative patient—highlighting the importance of biopsy in endoscopic abnormalities, even in asymptomatic individuals. In the absence of H. pylori or translocation-driven lymphomagenesis, localized disease can still respond favorably to ISRT. Though the prognosis of H. pylori-negative MALT lymphoma is less well defined, radiation therapy remains a highly effective modality in early-stage disease. As noted in the HELYX II trial, there were excellent outcomes showing complete eradication of MALT lymphoma in H. pylori-negative patients with 24–30 Gy radiotherapy. While surveillance intervals aren’t standardized in current literature, most guidelines are recommending endoscopic monitoring every 3–6 months for two years, then every 6–12 months, with long-term follow-up due to late relapse risk. This case reinforces the role of personalized management based on molecular and staging data.
References
ClinicalTrialsgps. Helicobacter – Lymphoma – Radiation Part I: Eradication, Part II: Radiation. https://www.clinicaltrialsgps.com/search-clinical-trials/trial-1100/. Published 2011. Accessed June 1, 2025.
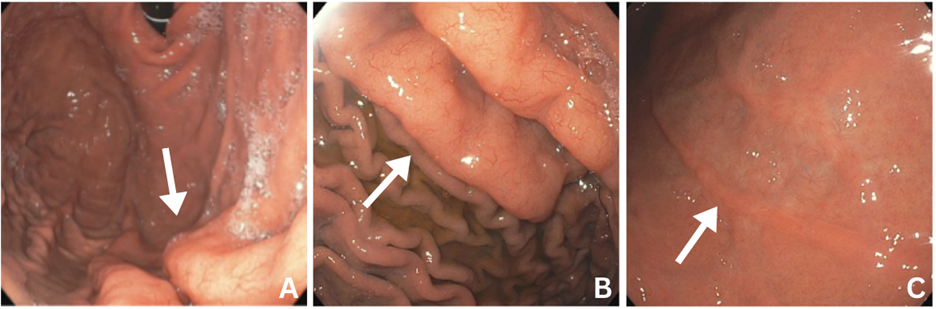
Figure: A: Initial findings showing abnormal folds (white arrow) in the gastric fundus and proximal body of the greater curvature where biopsy findings showed MALT lymphoma
B: 1-month follow-up showing persistence of abnormal folds (white arrow) in the area with biopsy-proven MALT lymphoma
C: 8-month follow-up after completion of radiation therapy showing the resolution and scarring of the previous folds (white arrow)
Disclosures:
Anveet Janwadkar indicated no relevant financial relationships.
Aishwarya Gatiganti indicated no relevant financial relationships.
Naseeruddin Naseem indicated no relevant financial relationships.
Yucel Aydin indicated no relevant financial relationships.
Leela Nayak indicated no relevant financial relationships.
Anveet Janwadkar, MD1, Aishwarya Gatiganti, MD1, Naseeruddin Naseem, MD1, Yucel Aydin, MD2, Leela Nayak, MD3. P6394 - Incidentally Detected <i>H. pylori</i>-Negative, t(11;18)-Negative Gastric MALT Lymphoma With Complete Response to Radiation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
