Tuesday Poster Session
Category: Stomach and Spleen
P6367 - Iron Gastropathy: When the Cure Becomes the Culprit
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- KA
Khaled Alsabbagh Alchirazi, MD
Aurora Health Care
Brookfield, WI
Presenting Author(s)
Khaled Alsabbagh Alchirazi, MD1, Nishkarsh Kumar, 2, Suzanna Logan, MD3, Tarun Sharma, MD4
1Aurora Health Care, Brookfield, WI; 2St. Luke's Hospital, Milwaukee, WI; 3Aurora Healthcare, Miluakee, WI; 4Aurora Health Care, Milwaukee, WI
Introduction: Iron pill gastropathy is an underrecognized cause of gastric mucosal injury, typically seen in patients on chronic oral iron supplementation. It can present with nonspecific gastrointestinal symptoms or, less commonly, overt upper gastrointestinal bleeding. Characteristic endoscopic and histopathologic features support the diagnosis. We present a rare case of iron pill gastropathy manifesting as symptomatic anemia in an elderly patient.
Case Description/
Methods: A 78-year-old female with a history of hypertension, hypertrophic obstructive cardiomyopathy, hyperlipidemia, type 2 diabetes, stage 4 chronic kidney disease, GERD and Iron Deficiency on oral iron presented with nausea, vomiting, and melena. She was afebrile, blood pressure was 178/82 mmHg, heart rate 98 bpm, and oxygen saturation was 100% on room air. Labs revealed hemoglobin of 6.7 g/dL (baseline 8–8.5), hematocrit 20.2% (baseline 26–28%), iron level 29 µg/dL, and TIBC 118 µg/dL. The patient received a red blood cell transfusion for symptomatic anemia. Esophagogastroduodenoscopy showed a normal esophagus and duodenum. However, multiple small nodular lesions with overlying acid hematin and scant oozing were visualized in the stomach body and fundus. Argon plasma coagulation was applied with good hemostasis. Gastric biopsies revealed oxyntic mucosa with intracytoplasmic iron deposits (confirmed by Prussian blue stain), lamina propria chronic inflammation, and surface epithelial erosion—consistent with iron pill gastropathy.
Discussion: Iron pill gastropathy results from mucosal injury due to direct oxidative damage by iron salts, especially ferrous sulfate. This entity is more frequently identified in elderly patients or those with chronic comorbidities such as CKD and diabetes, who are often on iron supplementation with a delayed gastric transit leading to increased local concentration. Endoscopically, it may mimic other causes of gastritis or neoplasia with findings such as erythema, erosions, or dark pigmented nodules. Histologic confirmation with Prussian blue staining is diagnostic. In this case, the patient likely developed gastric injury from chronic iron use, complicated by bleeding and anemia. Management includes cessation or modification of iron therapy to parenteral formulations and supportive care. Clinicians should maintain a high index of suspicion in at-risk populations presenting with unexplained upper GI symptoms or bleeding.
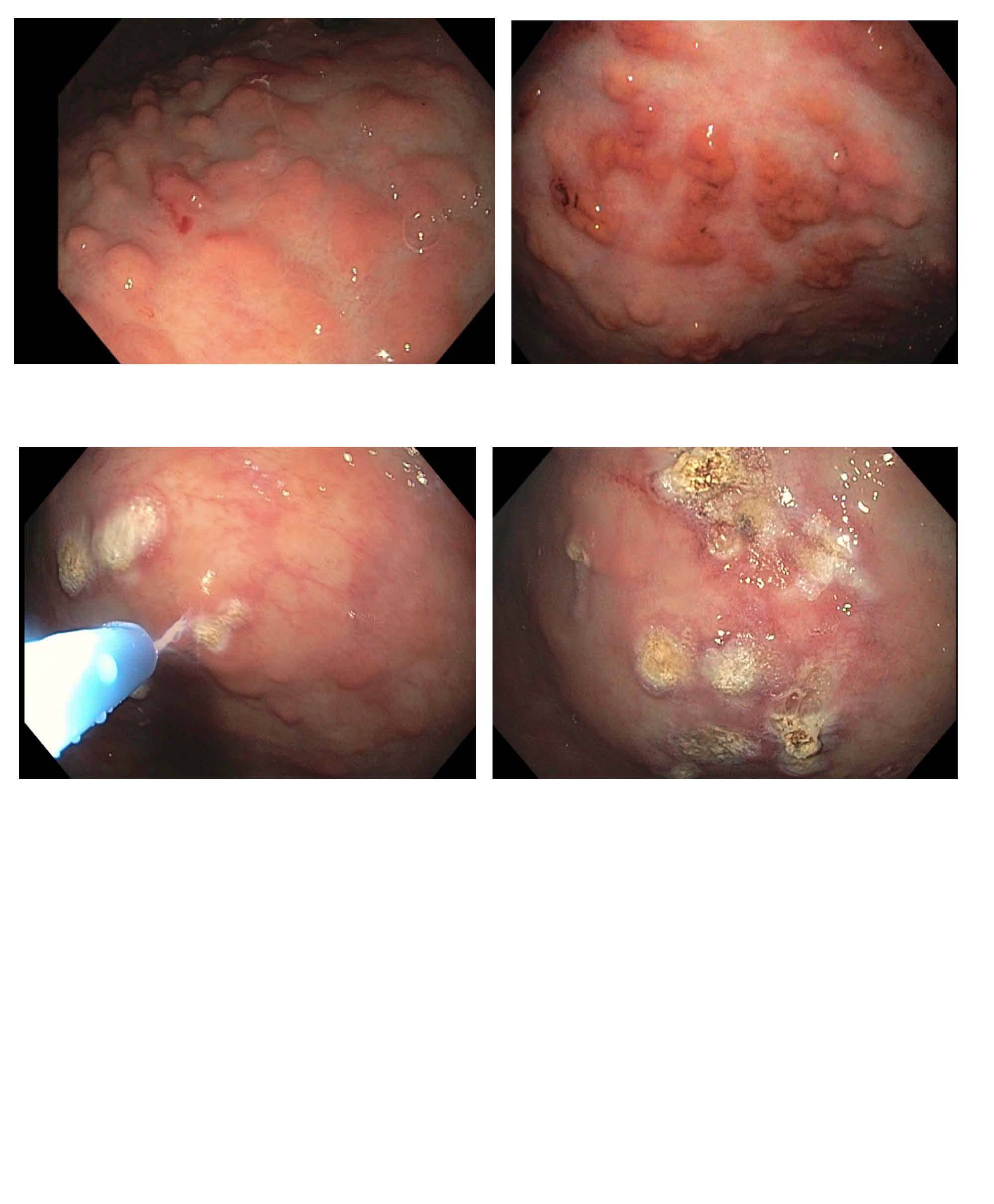
Figure: Image 1: Multiple small nodular lesions with overlying acid hematin and scant oozing subsequently treated with Argon plasma coagulation treatment.
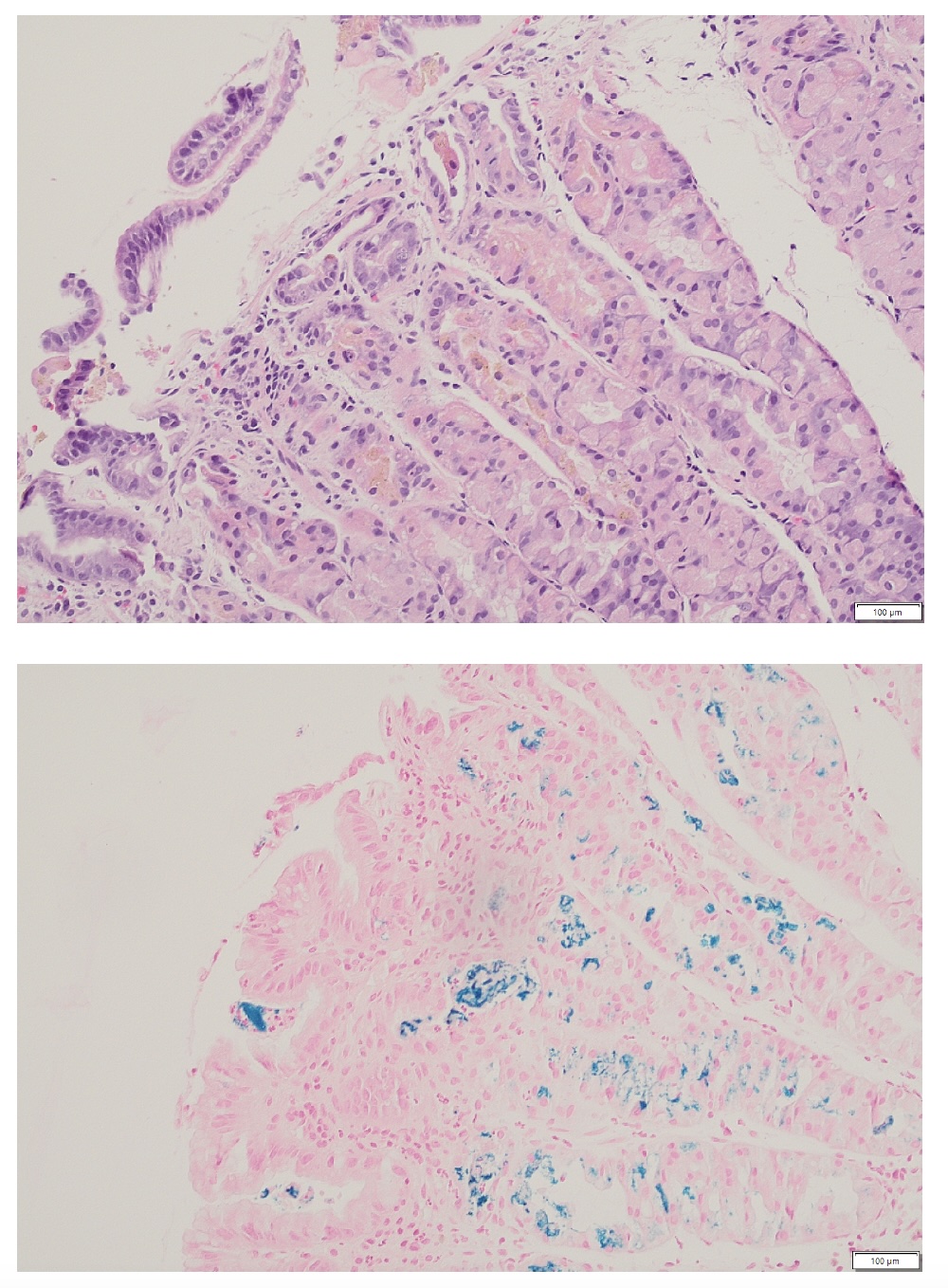
Figure: Image 2: Iron deposition in gastric glands highlighted by Prussian blue stain.
Disclosures:
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Nishkarsh Kumar indicated no relevant financial relationships.
Suzanna Logan indicated no relevant financial relationships.
Tarun Sharma indicated no relevant financial relationships.
Khaled Alsabbagh Alchirazi, MD1, Nishkarsh Kumar, 2, Suzanna Logan, MD3, Tarun Sharma, MD4. P6367 - Iron Gastropathy: When the Cure Becomes the Culprit, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Aurora Health Care, Brookfield, WI; 2St. Luke's Hospital, Milwaukee, WI; 3Aurora Healthcare, Miluakee, WI; 4Aurora Health Care, Milwaukee, WI
Introduction: Iron pill gastropathy is an underrecognized cause of gastric mucosal injury, typically seen in patients on chronic oral iron supplementation. It can present with nonspecific gastrointestinal symptoms or, less commonly, overt upper gastrointestinal bleeding. Characteristic endoscopic and histopathologic features support the diagnosis. We present a rare case of iron pill gastropathy manifesting as symptomatic anemia in an elderly patient.
Case Description/
Methods: A 78-year-old female with a history of hypertension, hypertrophic obstructive cardiomyopathy, hyperlipidemia, type 2 diabetes, stage 4 chronic kidney disease, GERD and Iron Deficiency on oral iron presented with nausea, vomiting, and melena. She was afebrile, blood pressure was 178/82 mmHg, heart rate 98 bpm, and oxygen saturation was 100% on room air. Labs revealed hemoglobin of 6.7 g/dL (baseline 8–8.5), hematocrit 20.2% (baseline 26–28%), iron level 29 µg/dL, and TIBC 118 µg/dL. The patient received a red blood cell transfusion for symptomatic anemia. Esophagogastroduodenoscopy showed a normal esophagus and duodenum. However, multiple small nodular lesions with overlying acid hematin and scant oozing were visualized in the stomach body and fundus. Argon plasma coagulation was applied with good hemostasis. Gastric biopsies revealed oxyntic mucosa with intracytoplasmic iron deposits (confirmed by Prussian blue stain), lamina propria chronic inflammation, and surface epithelial erosion—consistent with iron pill gastropathy.
Discussion: Iron pill gastropathy results from mucosal injury due to direct oxidative damage by iron salts, especially ferrous sulfate. This entity is more frequently identified in elderly patients or those with chronic comorbidities such as CKD and diabetes, who are often on iron supplementation with a delayed gastric transit leading to increased local concentration. Endoscopically, it may mimic other causes of gastritis or neoplasia with findings such as erythema, erosions, or dark pigmented nodules. Histologic confirmation with Prussian blue staining is diagnostic. In this case, the patient likely developed gastric injury from chronic iron use, complicated by bleeding and anemia. Management includes cessation or modification of iron therapy to parenteral formulations and supportive care. Clinicians should maintain a high index of suspicion in at-risk populations presenting with unexplained upper GI symptoms or bleeding.
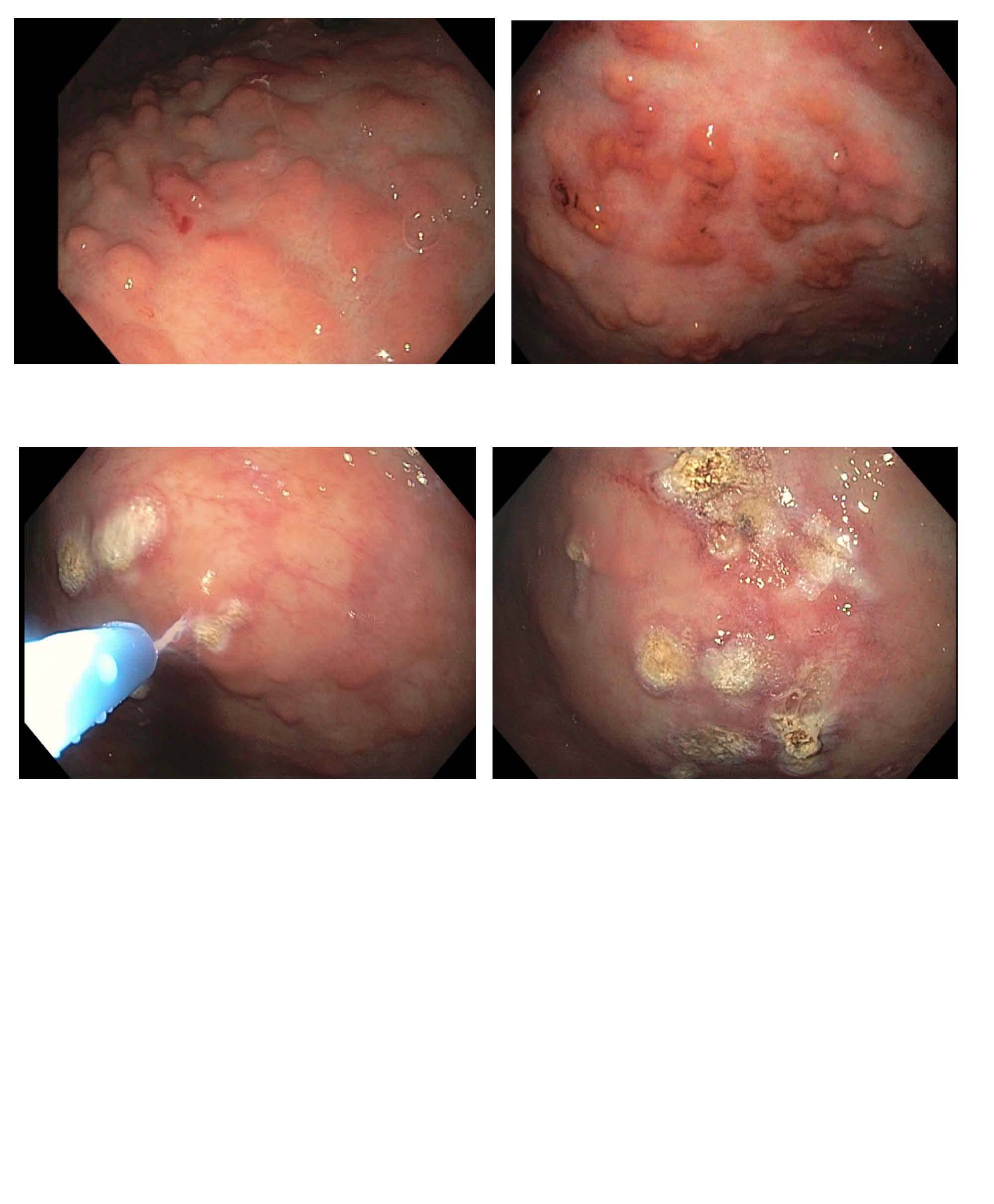
Figure: Image 1: Multiple small nodular lesions with overlying acid hematin and scant oozing subsequently treated with Argon plasma coagulation treatment.
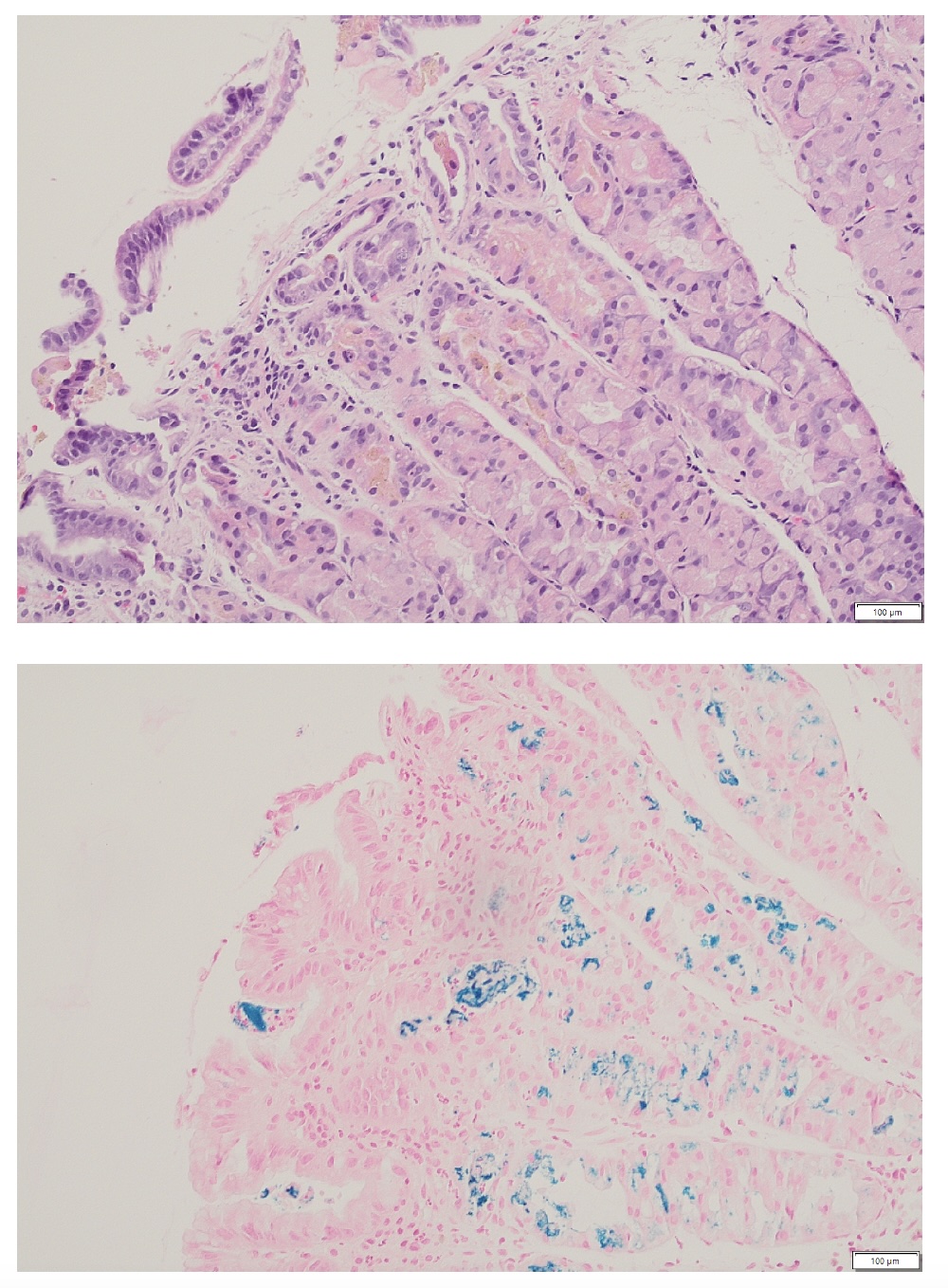
Figure: Image 2: Iron deposition in gastric glands highlighted by Prussian blue stain.
Disclosures:
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Nishkarsh Kumar indicated no relevant financial relationships.
Suzanna Logan indicated no relevant financial relationships.
Tarun Sharma indicated no relevant financial relationships.
Khaled Alsabbagh Alchirazi, MD1, Nishkarsh Kumar, 2, Suzanna Logan, MD3, Tarun Sharma, MD4. P6367 - Iron Gastropathy: When the Cure Becomes the Culprit, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
