Tuesday Poster Session
Category: Stomach and Spleen
P6354 - MALT Lymphoma and Chronic Inflammatory Demyelinating Polyneuropathy: A Case Suggesting Paraneoplastic Association
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RA
Rawia Aburumman, MD
Louisiana State University
Spring, TX
Presenting Author(s)
Rawia Aburumman, MD1, Naba Saeed, MD2, Michael Tran, MD3, Kshitij Arora, MD2
1Louisiana State University, Spring, TX; 2LSU Health, Shreveport, LA; 3LSU Health Shreveport, Shreveport, LA
Introduction: Mucosa-associated lymphoid tissue (MALT) lymphoma is a low-grade extra nodal B-cell lymphoma often linked to chronic Helicobacter pylori infection. Chronic inflammatory demyelinating polyneuropathy (CIDP) is an autoimmune peripheral neuropathy. CIDP can be associated with chronic inflammatory disease states that trigger B and T-cell mediated immune responses. It has been reported with several types of lymphomas suggesting a potential paraneoplastic disease manifestation. We present a case of coexisting CIDP and MALT lymphoma, raising the possibility of a shared immunopathogenesis.
Case Description/
Methods: 53-year-old male with diabetes and hypertension presented with progressive lower extremity weakness and sensory loss, and was diagnosed with CIDP. He was started on intravenous immunoglobulin (IVIG), resulting in significant improvement in his symptoms but continued to have residual weakness. Two years later, he underwent esophagogastroduodenoscopy (EGD) and colonoscopy for evaluation of iron deficiency anemia. EGD revealed moderate atrophic, erythematous mucosa involving the cardia, fundus, body, greater and lesser curvatures of the stomach, along with linear erosions in the antrum, findings consistent with gastritis. Biopsies confirmed MALT lymphoma with concurrent Helicobacter pylori infection. The patient completed bismuth quadruple therapy with eradication confirmed via breath testing. Follow-up EGD six months later showed patchy atrophic areas and several small nodules with central erythema in the antrum and body (greater curvature). Narrow Band Imaging (NBI) demonstrated darker-appearing mucosa in these regions, and repeat biopsies confirmed persistent MALT lymphoma with negative H.pylori testing this time.
Discussion: This case highlights a possible paraneoplastic relationship between MALT lymphoma and CIDP. Literature review reveals similar CIDP associations with other lymphomas, including diffuse large B-cell, T-cell, mantle cell, follicular and hodgkins lymphoma. In our patient, incomplete lymphoma regression after H. pylori eradication and the partial response of CIDP to IVIG suggest an immune-mediated connection. Clinicians should consider occult lymphoma in patients with atypical or treatment-refractory CIDP especially when accompanied with IDA. Further studies would help in understanding presenting CIDP symptoms that should hasten further investigation for malignancy, and to assess whether treatment of lymphoma also treats the CIDP.
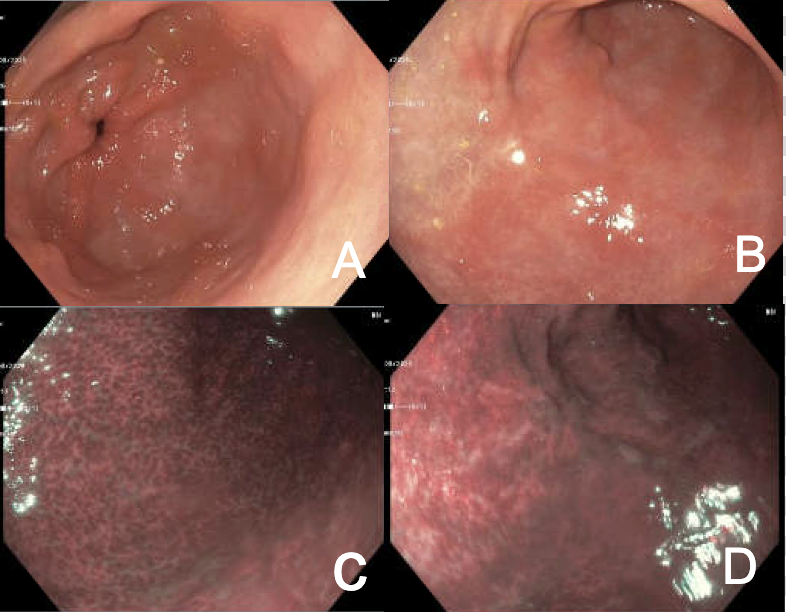
Figure: A and B: Endoscopic appearance of gastric mucosa during second EGD after completion of Quadruple therapy. C and D: Endoscopic appearance of gastric mucosa under NBI light highlighting underlying blood vessels “tree-like appearance”.
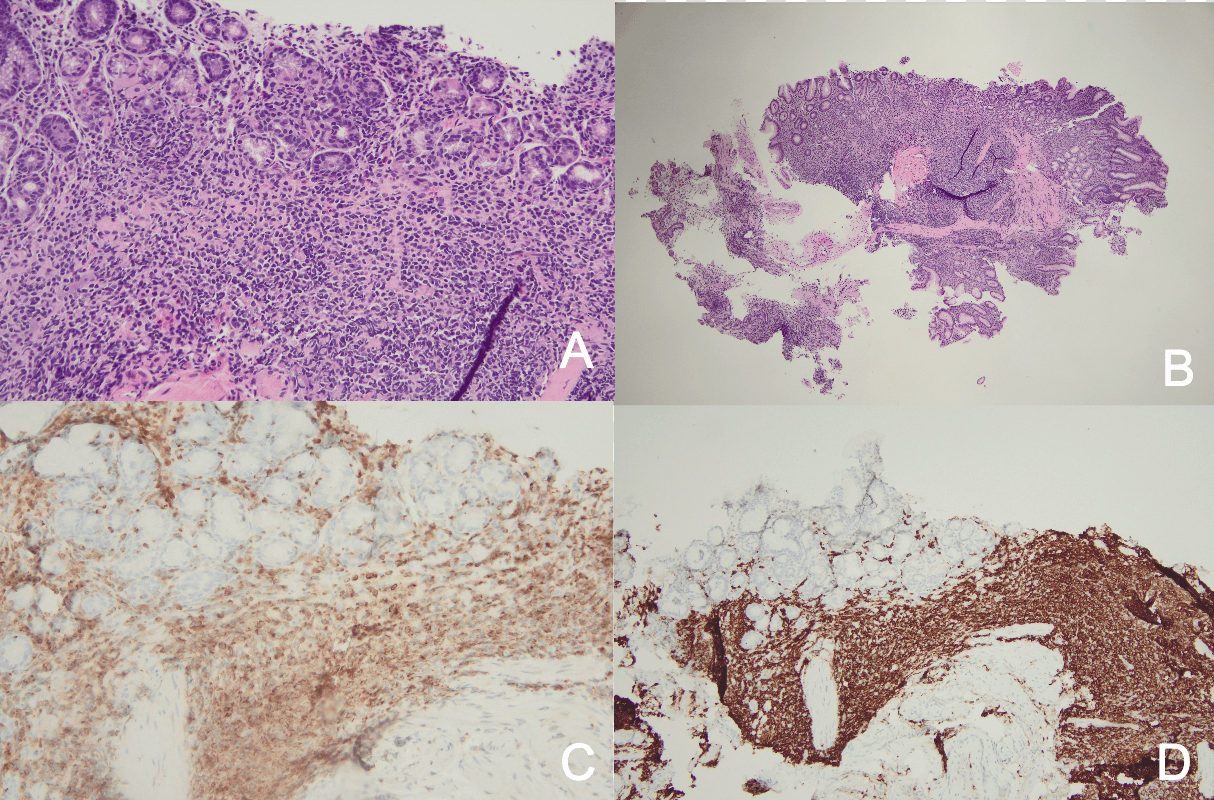
Figure: A and B: This is a hematoxylin and eosin (H&E) stained histology slide showing dense lymphoid infiltration of the gastrointestinal mucosa, most consistent with a low-grade lymphoma. C and D: This is an immunohistochemical (IHC) stained tissue section, showing expansion of lamina propria with atypical monocytoid B cells (CD20 and BCL 2 positive) and lymphoepithelial lesions.
Disclosures:
Rawia Aburumman indicated no relevant financial relationships.
Naba Saeed indicated no relevant financial relationships.
Michael Tran indicated no relevant financial relationships.
Kshitij Arora indicated no relevant financial relationships.
Rawia Aburumman, MD1, Naba Saeed, MD2, Michael Tran, MD3, Kshitij Arora, MD2. P6354 - MALT Lymphoma and Chronic Inflammatory Demyelinating Polyneuropathy: A Case Suggesting Paraneoplastic Association, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Louisiana State University, Spring, TX; 2LSU Health, Shreveport, LA; 3LSU Health Shreveport, Shreveport, LA
Introduction: Mucosa-associated lymphoid tissue (MALT) lymphoma is a low-grade extra nodal B-cell lymphoma often linked to chronic Helicobacter pylori infection. Chronic inflammatory demyelinating polyneuropathy (CIDP) is an autoimmune peripheral neuropathy. CIDP can be associated with chronic inflammatory disease states that trigger B and T-cell mediated immune responses. It has been reported with several types of lymphomas suggesting a potential paraneoplastic disease manifestation. We present a case of coexisting CIDP and MALT lymphoma, raising the possibility of a shared immunopathogenesis.
Case Description/
Methods: 53-year-old male with diabetes and hypertension presented with progressive lower extremity weakness and sensory loss, and was diagnosed with CIDP. He was started on intravenous immunoglobulin (IVIG), resulting in significant improvement in his symptoms but continued to have residual weakness. Two years later, he underwent esophagogastroduodenoscopy (EGD) and colonoscopy for evaluation of iron deficiency anemia. EGD revealed moderate atrophic, erythematous mucosa involving the cardia, fundus, body, greater and lesser curvatures of the stomach, along with linear erosions in the antrum, findings consistent with gastritis. Biopsies confirmed MALT lymphoma with concurrent Helicobacter pylori infection. The patient completed bismuth quadruple therapy with eradication confirmed via breath testing. Follow-up EGD six months later showed patchy atrophic areas and several small nodules with central erythema in the antrum and body (greater curvature). Narrow Band Imaging (NBI) demonstrated darker-appearing mucosa in these regions, and repeat biopsies confirmed persistent MALT lymphoma with negative H.pylori testing this time.
Discussion: This case highlights a possible paraneoplastic relationship between MALT lymphoma and CIDP. Literature review reveals similar CIDP associations with other lymphomas, including diffuse large B-cell, T-cell, mantle cell, follicular and hodgkins lymphoma. In our patient, incomplete lymphoma regression after H. pylori eradication and the partial response of CIDP to IVIG suggest an immune-mediated connection. Clinicians should consider occult lymphoma in patients with atypical or treatment-refractory CIDP especially when accompanied with IDA. Further studies would help in understanding presenting CIDP symptoms that should hasten further investigation for malignancy, and to assess whether treatment of lymphoma also treats the CIDP.
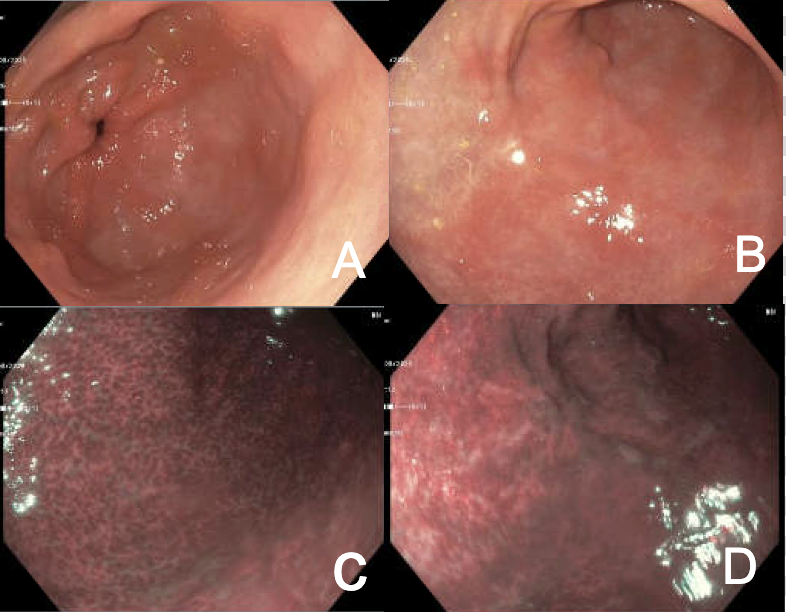
Figure: A and B: Endoscopic appearance of gastric mucosa during second EGD after completion of Quadruple therapy. C and D: Endoscopic appearance of gastric mucosa under NBI light highlighting underlying blood vessels “tree-like appearance”.
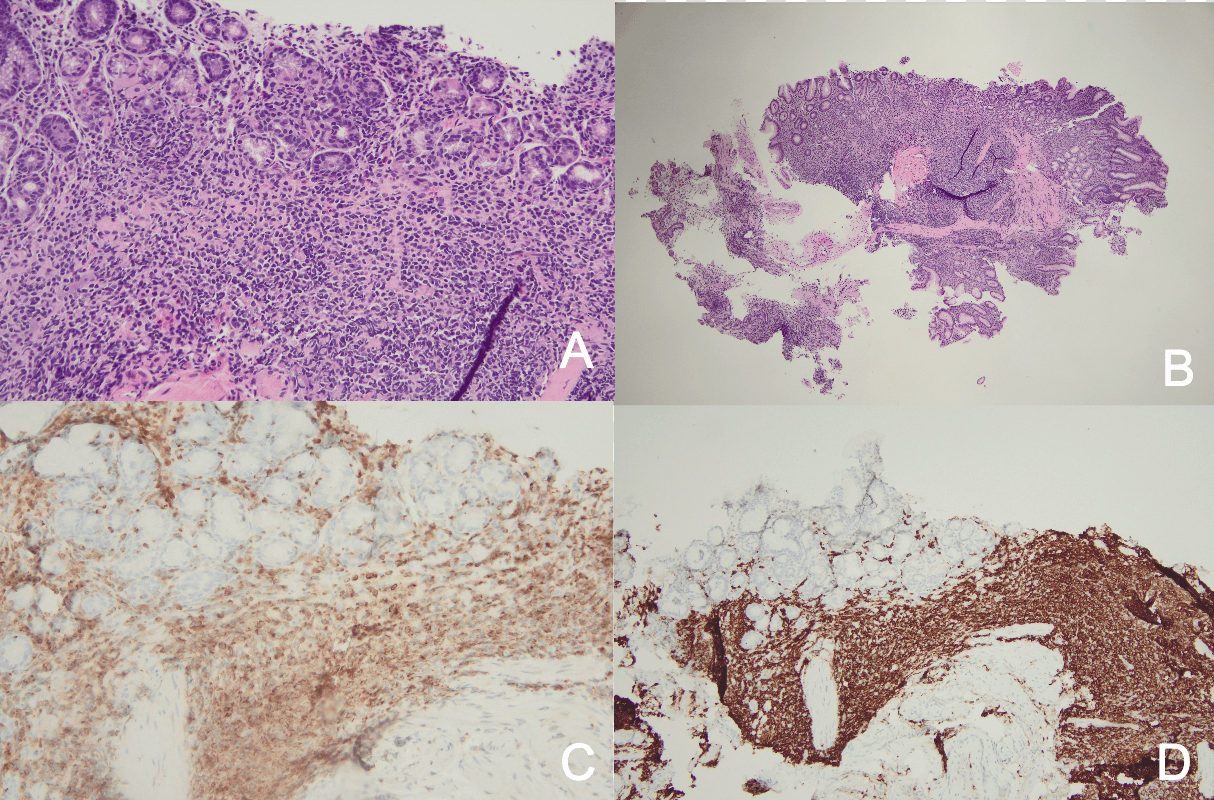
Figure: A and B: This is a hematoxylin and eosin (H&E) stained histology slide showing dense lymphoid infiltration of the gastrointestinal mucosa, most consistent with a low-grade lymphoma. C and D: This is an immunohistochemical (IHC) stained tissue section, showing expansion of lamina propria with atypical monocytoid B cells (CD20 and BCL 2 positive) and lymphoepithelial lesions.
Disclosures:
Rawia Aburumman indicated no relevant financial relationships.
Naba Saeed indicated no relevant financial relationships.
Michael Tran indicated no relevant financial relationships.
Kshitij Arora indicated no relevant financial relationships.
Rawia Aburumman, MD1, Naba Saeed, MD2, Michael Tran, MD3, Kshitij Arora, MD2. P6354 - MALT Lymphoma and Chronic Inflammatory Demyelinating Polyneuropathy: A Case Suggesting Paraneoplastic Association, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
