Tuesday Poster Session
Category: Stomach and Spleen
P6343 - The Diagnosis of Gastric Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma Needs Heightened Alert
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anna Lauren G. Winter, MD
University of Mississippi Medical Center
Jackson, MS
Presenting Author(s)
Anna Lauren G. Winter, MD, Namrata Paladugu, MD, Anna H.. Owings, DO, Shou-jiang Tang, MD
University of Mississippi Medical Center, Jackson, MS
Introduction: Gastric mucosa-associated lymphoid tissue (MALT) lymphoma is an extranodal marginal zone B-cell lymphoma that often arises in the stomach and is most commonly due to Helicobacter pylori infection. Diagnosis of gastric MALT lymphoma is established by obtaining multiple endoscopic biopsies from normal and abnormal appearing gastric mucosa. Here, we present a case of newly diagnosed gastric MALT lymphoma that was nearly missed on endoscopy and pathology.
Case Description/
Methods: A 79-year-old man with hypertension presented with fatigue, melena, and bright red blood per rectum. He endorsed 20 pounds of unintentional weight loss over the past 6 months. Vital signs were within normal limits. On physical exam, there was tenderness to palpation in the left lower quadrant of the abdomen. Hemoglobin was 6.3 g/dL on admission, decreased from 9.2 g/dL prior. He was started on a proton pump inhibitor and underwent endoscopy. Esophagogastroduodenoscopy (EGD) showed two non-bleeding large ulcers in the gastric body 40 mm x 30 mm and 30 mm x 3 mm in size. The ulcer edges were biopsied. Colonoscopy revealed 15 mm and 13 mm semi-pedunculated polyps, both of which were removed. Pathology of the gastric ulcer biopsy showed evidence of ulceration, reactive gastropathy, increased eosinophils, and intestinal metaplasia, as well as prominent lymphoid aggregates of B-lineage lymphocytes, which was attributed to chronic inflammation. He was discharged and returned in 2 months for a routinely scheduled EGD to ensure ulcer healing. He was asymptomatic since the index EGD and with proton pump inhibitor treatment. The endoscopists reviewed prior endoscopic images and noted all gastric ulcerations had completely healed. However, the mucosa surrounding the scar tissue appeared indurated. Since the previous ulcerations were in atypical location for peptic ulcer and there was mucosal induration on current EGD, endoscopists obtained biopsy of the scar tissue and surrounding mucosa. Flow cytometry detected monotypic B cell lymphoma in both lesions, and no transformation with large cell lymphoma was seen.
Discussion: Diagnosis of MALT lymphoma requires histological examination of gastric biopsies. To improve accuracy, samples should be taken from both abnormal and normal-appearing mucosa due to the disease’s patchy and subtle nature. Indurated areas near healed ulcers or atypical ulcer locations, such as the antrum, should be biopsied and evaluated with surgical pathology and flow cytometry during the initial EGD.
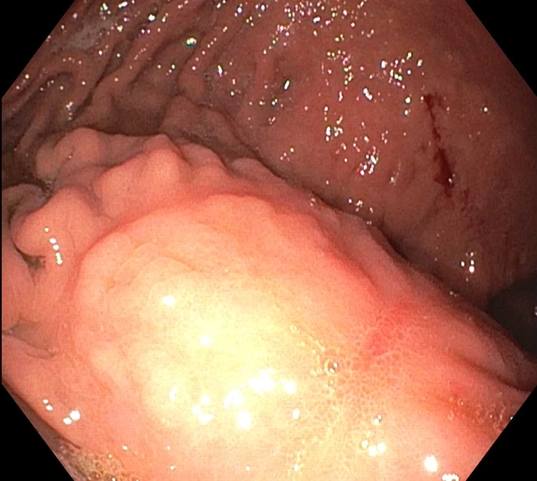
Figure: Non-bleeding cratered ulcer in the lesser curvature of the stomach.
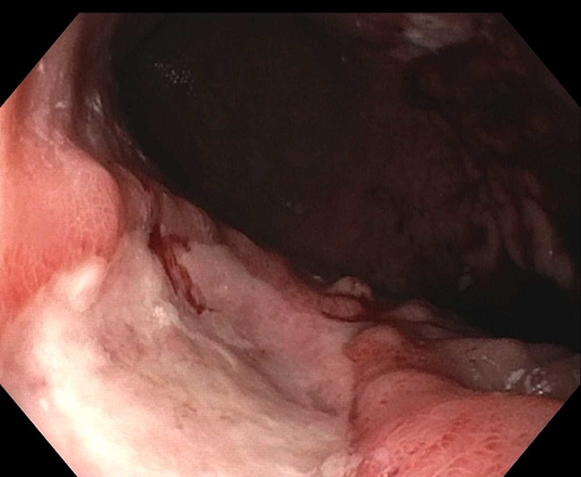
Figure: Small healed ulcer with scar tissue found in the gastric body.
Disclosures:
Anna Lauren Winter indicated no relevant financial relationships.
Namrata Paladugu indicated no relevant financial relationships.
Anna Owings indicated no relevant financial relationships.
Shou-jiang Tang indicated no relevant financial relationships.
Anna Lauren G. Winter, MD, Namrata Paladugu, MD, Anna H.. Owings, DO, Shou-jiang Tang, MD. P6343 - The Diagnosis of Gastric Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma Needs Heightened Alert, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Mississippi Medical Center, Jackson, MS
Introduction: Gastric mucosa-associated lymphoid tissue (MALT) lymphoma is an extranodal marginal zone B-cell lymphoma that often arises in the stomach and is most commonly due to Helicobacter pylori infection. Diagnosis of gastric MALT lymphoma is established by obtaining multiple endoscopic biopsies from normal and abnormal appearing gastric mucosa. Here, we present a case of newly diagnosed gastric MALT lymphoma that was nearly missed on endoscopy and pathology.
Case Description/
Methods: A 79-year-old man with hypertension presented with fatigue, melena, and bright red blood per rectum. He endorsed 20 pounds of unintentional weight loss over the past 6 months. Vital signs were within normal limits. On physical exam, there was tenderness to palpation in the left lower quadrant of the abdomen. Hemoglobin was 6.3 g/dL on admission, decreased from 9.2 g/dL prior. He was started on a proton pump inhibitor and underwent endoscopy. Esophagogastroduodenoscopy (EGD) showed two non-bleeding large ulcers in the gastric body 40 mm x 30 mm and 30 mm x 3 mm in size. The ulcer edges were biopsied. Colonoscopy revealed 15 mm and 13 mm semi-pedunculated polyps, both of which were removed. Pathology of the gastric ulcer biopsy showed evidence of ulceration, reactive gastropathy, increased eosinophils, and intestinal metaplasia, as well as prominent lymphoid aggregates of B-lineage lymphocytes, which was attributed to chronic inflammation. He was discharged and returned in 2 months for a routinely scheduled EGD to ensure ulcer healing. He was asymptomatic since the index EGD and with proton pump inhibitor treatment. The endoscopists reviewed prior endoscopic images and noted all gastric ulcerations had completely healed. However, the mucosa surrounding the scar tissue appeared indurated. Since the previous ulcerations were in atypical location for peptic ulcer and there was mucosal induration on current EGD, endoscopists obtained biopsy of the scar tissue and surrounding mucosa. Flow cytometry detected monotypic B cell lymphoma in both lesions, and no transformation with large cell lymphoma was seen.
Discussion: Diagnosis of MALT lymphoma requires histological examination of gastric biopsies. To improve accuracy, samples should be taken from both abnormal and normal-appearing mucosa due to the disease’s patchy and subtle nature. Indurated areas near healed ulcers or atypical ulcer locations, such as the antrum, should be biopsied and evaluated with surgical pathology and flow cytometry during the initial EGD.
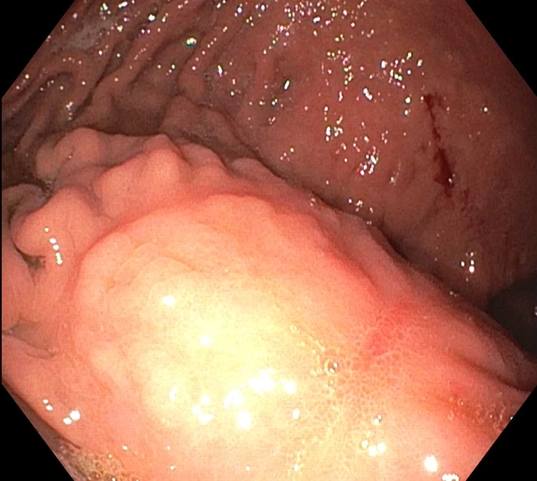
Figure: Non-bleeding cratered ulcer in the lesser curvature of the stomach.
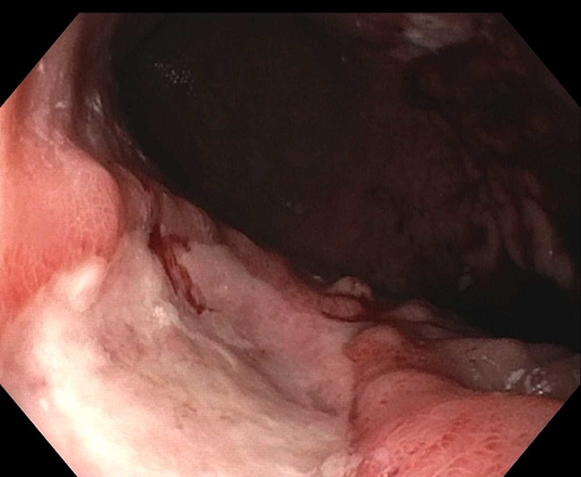
Figure: Small healed ulcer with scar tissue found in the gastric body.
Disclosures:
Anna Lauren Winter indicated no relevant financial relationships.
Namrata Paladugu indicated no relevant financial relationships.
Anna Owings indicated no relevant financial relationships.
Shou-jiang Tang indicated no relevant financial relationships.
Anna Lauren G. Winter, MD, Namrata Paladugu, MD, Anna H.. Owings, DO, Shou-jiang Tang, MD. P6343 - The Diagnosis of Gastric Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma Needs Heightened Alert, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
