Monday Poster Session
Category: Biliary/Pancreas
P2190 - High-Volume Centers and Necrotizing Pancreatitis: Balancing Complexity and Outcomes
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hima Varsha Voruganti, MD
North Alabama Medical Center
Florence, AL
Presenting Author(s)
Hima Varsha Voruganti, MD1, Rohit Sekandlapuram, MD2, Rahul Karna, MD3, Mohammad Bilal, MD, FACG4, Shifa Umar, MD5, Rineetha Tandra, MD, MBBS6
1North Alabama Medical Center, Florence, AL; 2The Brooklyn Hospital Center, Brooklyn, NY; 3University of Minnesota Medical Center, Minneapolis, MN; 4University of Colorado Anschutz Medical Campus, Denver, CO; 5Baylor College of Medicine, Houston, TX; 6Baton Rouge General Medical Center, Baton Rogue, LA
Introduction:Necrotizing pancreatitis (NP) comprising 5-10% of acute pancreatitis is associated with high morbidity and mortality. Hospital volume may affect outcomes, but data on this association are limited. This study uses national inpatient sample database to compare patient demographics and outcomes across hospital volume tertiles, aiming to inform referral decisions and enhance care delivery.
1North Alabama Medical Center, Florence, AL; 2The Brooklyn Hospital Center, Brooklyn, NY; 3University of Minnesota Medical Center, Minneapolis, MN; 4University of Colorado Anschutz Medical Campus, Denver, CO; 5Baylor College of Medicine, Houston, TX; 6Baton Rouge General Medical Center, Baton Rogue, LA
Introduction:
Necrotizing pancreatitis (NP) comprising 5-10% of acute pancreatitis is associated with high morbidity and mortality. Hospital volume may affect outcomes, but data on this association are limited. This study uses national inpatient sample database to compare patient demographics and outcomes across hospital volume tertiles, aiming to inform referral decisions and enhance care delivery.
Methods: We retrospectively analyzed adult hospitalizations for NP using the National Inpatient Sample (2018–2020). Hospitals were stratified by case volume tertiles based on percentiles: low-volume (≤25th percentile, ≤2 cases), medium-volume ( >25th to ≤75th percentile, 3–8 cases), and high-volume ( >75th percentile, >8 cases). Survey-weighted analyses compared demographics, hospital traits, and outcomes—including age, sex, race, income, Charlson Comorbidity Index, region, teaching status, bed size, mortality, length of stay, and total charges—ensuring national representativeness. Variance estimation was adjusted using Stata’s singleunit(centered) option to address strata with a single PSU, in accordance with HCUP survey analysis guidelines.
Results: Among 90,495 weighted hospitalizations for NP, 11,040 occurred in low-volume, 39,275 in medium-volume, and 40,180 in high-volume centers (Table 1). High-volume centers had a significantly greater proportion of admissions in large, urban teaching hospitals (p< 0.001). Mean in-hospital mortality increased significantly with volume: 3.8% (low), 4.8% (medium), and 5.9% (high) (p< 0.001). Length of stay was significantly longer in high-volume hospitals (13.1 days) compared to medium (11.6 days) and low-volume centers (9.2 days) (p< 0.001). Similarly, mean total charges were highest in high-volume centers ($169,785), followed by medium ($143,620) and low-volume centers ($107,273) (p< 0.001) (Table 2). High-volume centers also had a significantly higher proportion of patients with severe Charlson Comorbidity Index scores (p=0.0008) and greater resource utilization.
Discussion: Our analysis demonstrates that high-volume centers manage a disproportionate share of necrotizing pancreatitis hospitalizations and are more often large, urban teaching hospitals. Despite greater resource utilization, these centers showed higher mortality and longer lengths of stay, likely reflecting more complex patient populations with severe comorbidities.
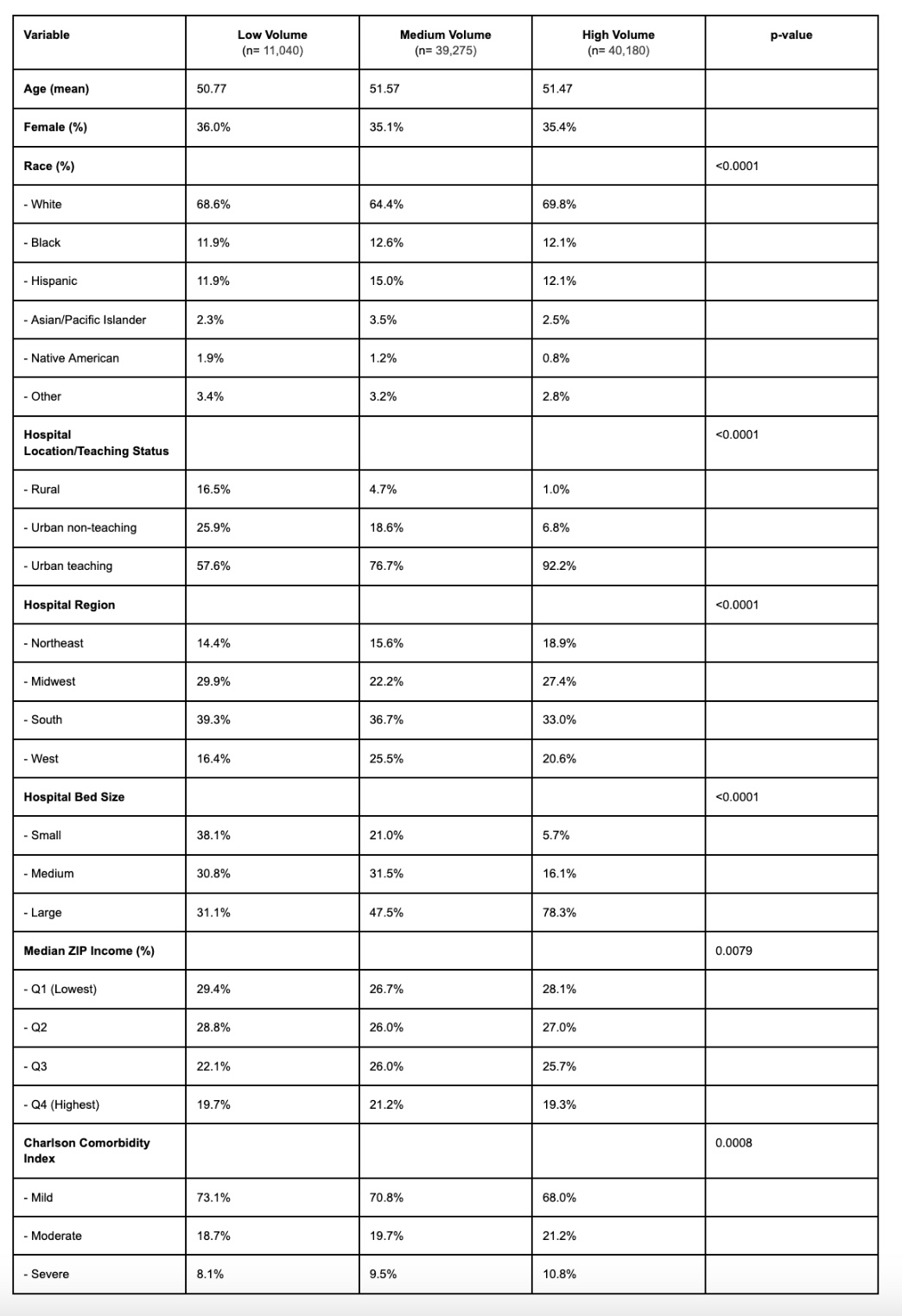
Figure: Table 1: Distribution of Patient and Hospital Characteristics by Hospital Volume Category.

Figure: Table 2: Unadjusted Survey-Weighted Means by Hospital Volume Category
Disclosures:
Hima Varsha Voruganti indicated no relevant financial relationships.
Rohit Sekandlapuram indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Shifa Umar indicated no relevant financial relationships.
Rineetha Tandra indicated no relevant financial relationships.
Hima Varsha Voruganti, MD1, Rohit Sekandlapuram, MD2, Rahul Karna, MD3, Mohammad Bilal, MD, FACG4, Shifa Umar, MD5, Rineetha Tandra, MD, MBBS6. P2190 - High-Volume Centers and Necrotizing Pancreatitis: Balancing Complexity and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Discussion: Our analysis demonstrates that high-volume centers manage a disproportionate share of necrotizing pancreatitis hospitalizations and are more often large, urban teaching hospitals. Despite greater resource utilization, these centers showed higher mortality and longer lengths of stay, likely reflecting more complex patient populations with severe comorbidities.
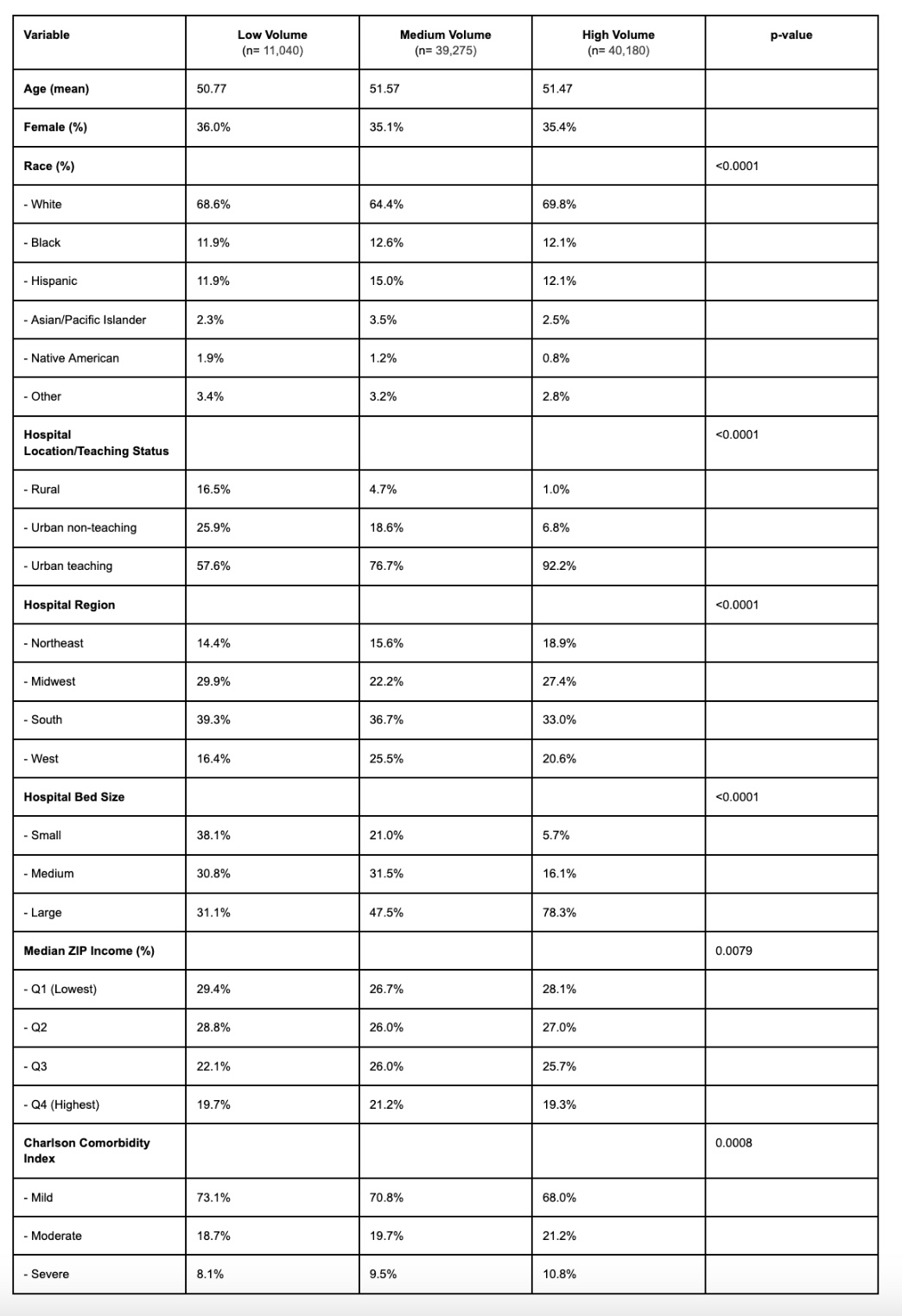
Figure: Table 1: Distribution of Patient and Hospital Characteristics by Hospital Volume Category.

Figure: Table 2: Unadjusted Survey-Weighted Means by Hospital Volume Category
Disclosures:
Hima Varsha Voruganti indicated no relevant financial relationships.
Rohit Sekandlapuram indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Shifa Umar indicated no relevant financial relationships.
Rineetha Tandra indicated no relevant financial relationships.
Hima Varsha Voruganti, MD1, Rohit Sekandlapuram, MD2, Rahul Karna, MD3, Mohammad Bilal, MD, FACG4, Shifa Umar, MD5, Rineetha Tandra, MD, MBBS6. P2190 - High-Volume Centers and Necrotizing Pancreatitis: Balancing Complexity and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

