Monday Poster Session
Category: Biliary/Pancreas
P2170 - Predictors of High-Cost Unplanned Readmissions After Curative Surgery for Localized Pancreatic Cancer: A Nationwide Analysis of Surgical Approach, Complications, and Outcomes
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Iqra Arshad, MD, MPH (she/her/hers)
SSM Health Saint Louis University Hospital
Saint Louis, MO
Presenting Author(s)
Nehemias Guevara Rodriguez, MD1, Iqra Arshad, MD, MPH1, Ronald Blanco Montecino, MD2, Noemy Coreas, MD3, Mahmoud Y. Madi, MD4, Wissam Kiwan, MD1
1SSM Health Saint Louis University Hospital, Saint Louis, MO; 2St. Barnabas Hospital, New York, NY; 3National University of El Salvador, El Salvador, San Salvador, El Salvador; 4University of Texas at Austin Dell Medical School, Austin, TX
Introduction: High-cost unplanned readmissions in localized pancreatic cancer patients following curative surgical treatment represent a significant burden to the healthcare system. The drivers of these high-cost readmissions remain poorly characterized. The current study aims to assess predictors of high-cost readmissions among patients who underwent curative surgery for localized pancreatic cancer during index hospitalization from a Nationwide perspective.
Methods: We conducted a retrospective cohort analysis using the Nationwide Readmissions Database (NRD) from 2016 to 2019, focusing on adult patients with localized pancreatic cancer who underwent surgical resection with curative intent. We identified 30-day unplanned readmissions following index surgical hospitalization using NRD-defined linkage variables and admission timing. Based on cost distribution analysis, readmissions were categorized as high-cost if the total hospital cost exceeded the 75th percentile ($18,132.92). Data on patients demographics, comorbidity burden (Charlson Comorbidity Index), surgical approach (open, laparoscopic, robotic), and complications (e.g., pancreatic leak) were extracted. We performed bivariate comparisons using chi-square tests for categorical variables and t-tests for continuous variables and a multivariable linear regression model to assess independent predictors of log-transformed readmission costs. Statistical significance was defined as p < 0.05.
Results: 46.3% of readmissions among the cohort were classified as high-cost. Among the high-cost group, patients underwent open surgery (71.4%), while other approaches (laparoscopic and robotic) accounted for only 41.2%. High-cost readmissions were significantly associated with longer length of stay (5.39 vs. 4.80 days; p = 0.005) but not with demographic factors, or Charlson Comorbidity Index. Although not statistically significant, high-cost readmissions were more common in patients with postoperative pancreatic leaks (57.1% vs. 42.9%, p = 0.411) and those undergoing laparoscopic surgery. Disease progression (ICD-10 C25*) was the leading cause of readmission (81.7%), followed by biliary obstruction (4.7%) and sepsis (1.7%).
Discussion: Study highlights that nearly half of readmissions result in high-cost hospitalization, and importantly, disease progression was the predominant cause of readmissions, thus, highlighting the need for improved perioperative risk stratification and early outpatient monitoring to mitigate the burden of high-cost readmissions.
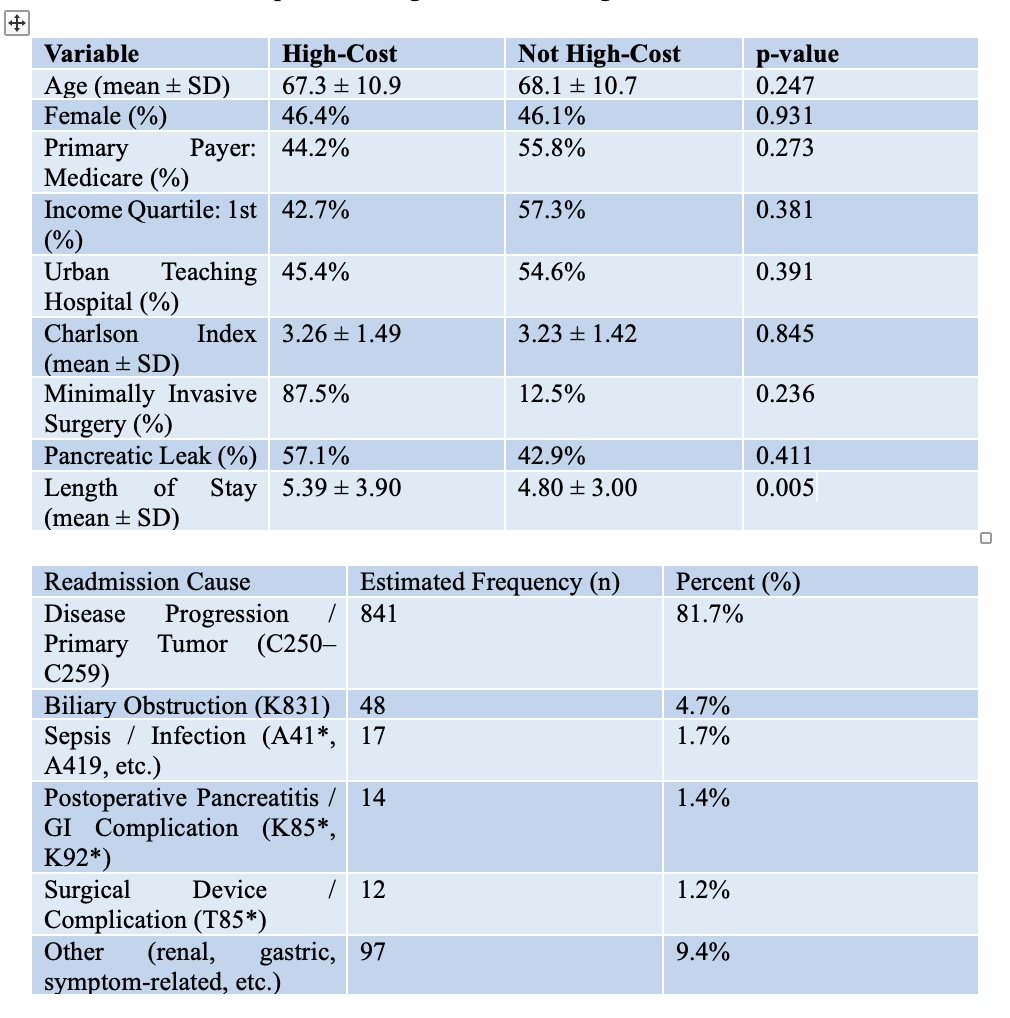
Figure: Table 1. Baseline Characteristics of Overall Study Cohort
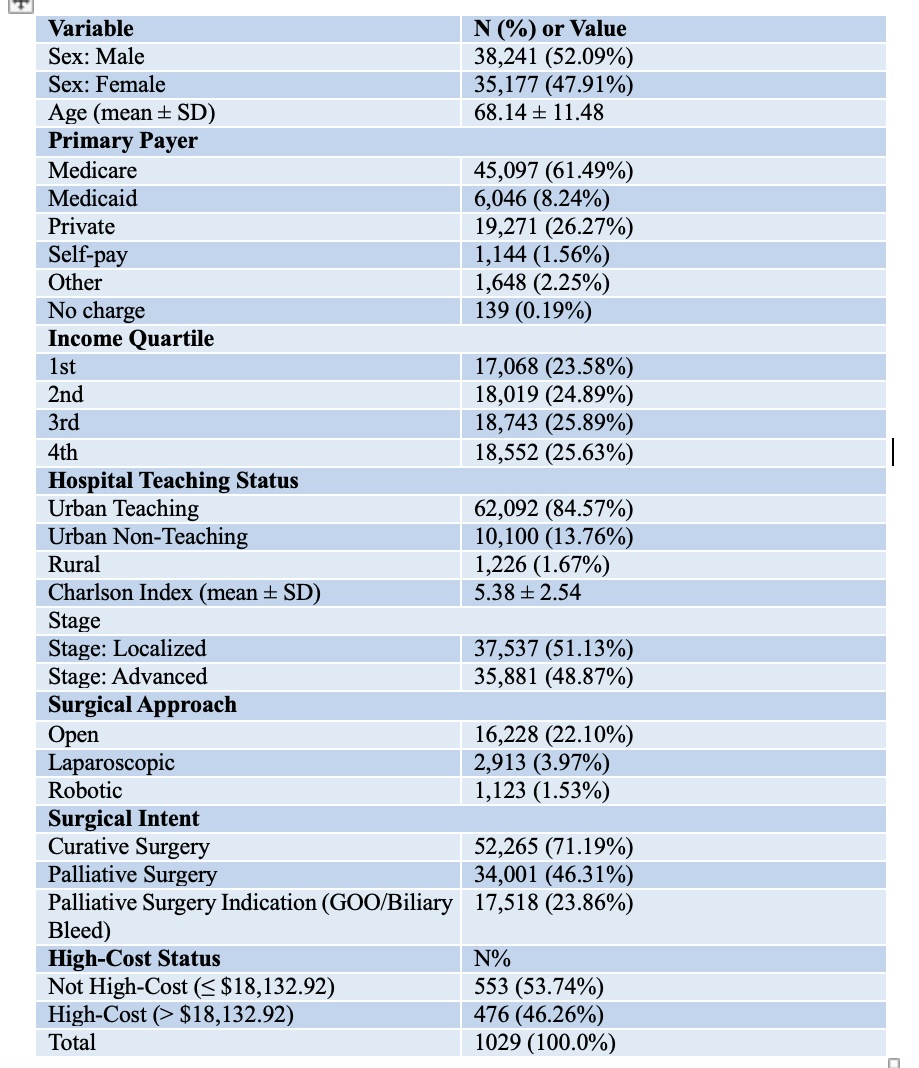
Figure: Table 2. Bivariate Comparison of High Cost Versus Non-High Cost Groups. Table 3. Primary Reasons for 30-day Unplanned Readmissions.
Disclosures:
Nehemias Guevara Rodriguez indicated no relevant financial relationships.
Iqra Arshad indicated no relevant financial relationships.
Ronald Blanco Montecino indicated no relevant financial relationships.
Noemy Coreas indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Wissam Kiwan indicated no relevant financial relationships.
Nehemias Guevara Rodriguez, MD1, Iqra Arshad, MD, MPH1, Ronald Blanco Montecino, MD2, Noemy Coreas, MD3, Mahmoud Y. Madi, MD4, Wissam Kiwan, MD1. P2170 - Predictors of High-Cost Unplanned Readmissions After Curative Surgery for Localized Pancreatic Cancer: A Nationwide Analysis of Surgical Approach, Complications, and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SSM Health Saint Louis University Hospital, Saint Louis, MO; 2St. Barnabas Hospital, New York, NY; 3National University of El Salvador, El Salvador, San Salvador, El Salvador; 4University of Texas at Austin Dell Medical School, Austin, TX
Introduction: High-cost unplanned readmissions in localized pancreatic cancer patients following curative surgical treatment represent a significant burden to the healthcare system. The drivers of these high-cost readmissions remain poorly characterized. The current study aims to assess predictors of high-cost readmissions among patients who underwent curative surgery for localized pancreatic cancer during index hospitalization from a Nationwide perspective.
Methods: We conducted a retrospective cohort analysis using the Nationwide Readmissions Database (NRD) from 2016 to 2019, focusing on adult patients with localized pancreatic cancer who underwent surgical resection with curative intent. We identified 30-day unplanned readmissions following index surgical hospitalization using NRD-defined linkage variables and admission timing. Based on cost distribution analysis, readmissions were categorized as high-cost if the total hospital cost exceeded the 75th percentile ($18,132.92). Data on patients demographics, comorbidity burden (Charlson Comorbidity Index), surgical approach (open, laparoscopic, robotic), and complications (e.g., pancreatic leak) were extracted. We performed bivariate comparisons using chi-square tests for categorical variables and t-tests for continuous variables and a multivariable linear regression model to assess independent predictors of log-transformed readmission costs. Statistical significance was defined as p < 0.05.
Results: 46.3% of readmissions among the cohort were classified as high-cost. Among the high-cost group, patients underwent open surgery (71.4%), while other approaches (laparoscopic and robotic) accounted for only 41.2%. High-cost readmissions were significantly associated with longer length of stay (5.39 vs. 4.80 days; p = 0.005) but not with demographic factors, or Charlson Comorbidity Index. Although not statistically significant, high-cost readmissions were more common in patients with postoperative pancreatic leaks (57.1% vs. 42.9%, p = 0.411) and those undergoing laparoscopic surgery. Disease progression (ICD-10 C25*) was the leading cause of readmission (81.7%), followed by biliary obstruction (4.7%) and sepsis (1.7%).
Discussion: Study highlights that nearly half of readmissions result in high-cost hospitalization, and importantly, disease progression was the predominant cause of readmissions, thus, highlighting the need for improved perioperative risk stratification and early outpatient monitoring to mitigate the burden of high-cost readmissions.
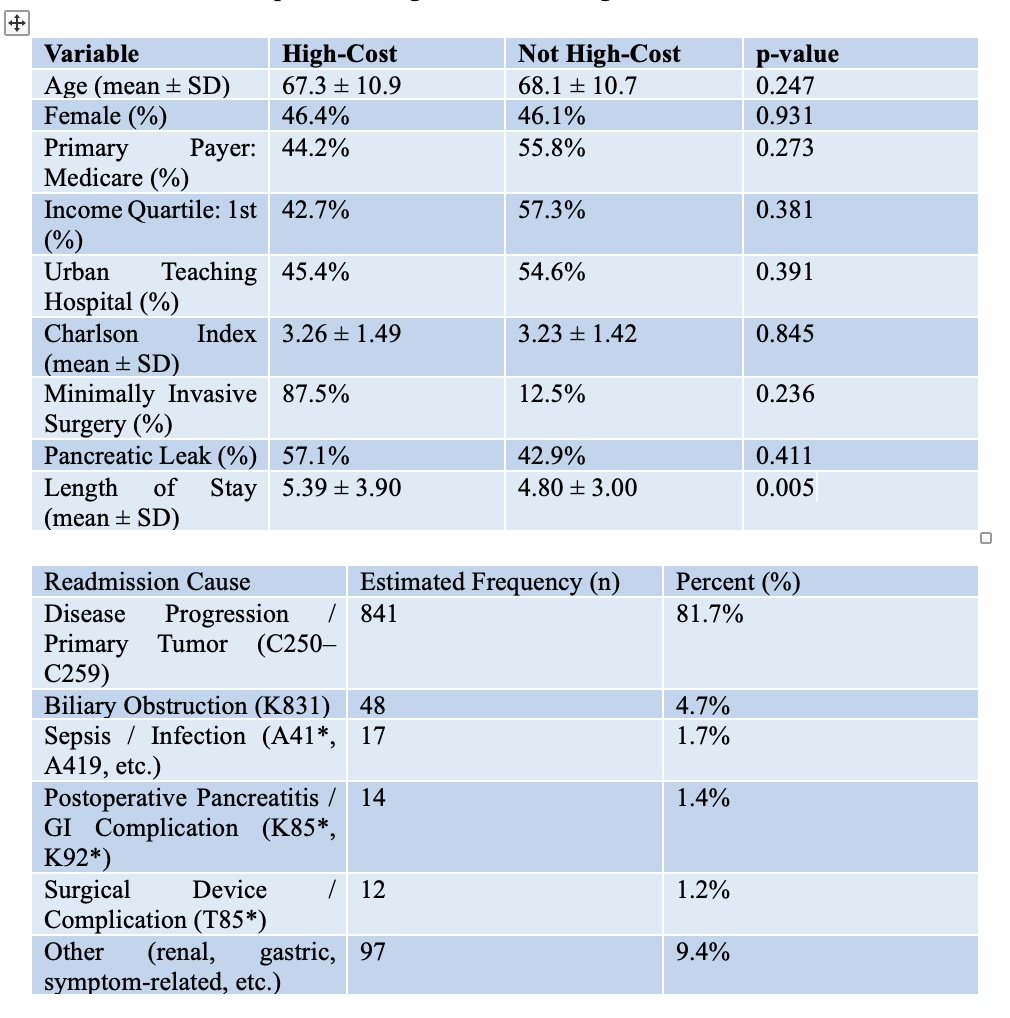
Figure: Table 1. Baseline Characteristics of Overall Study Cohort
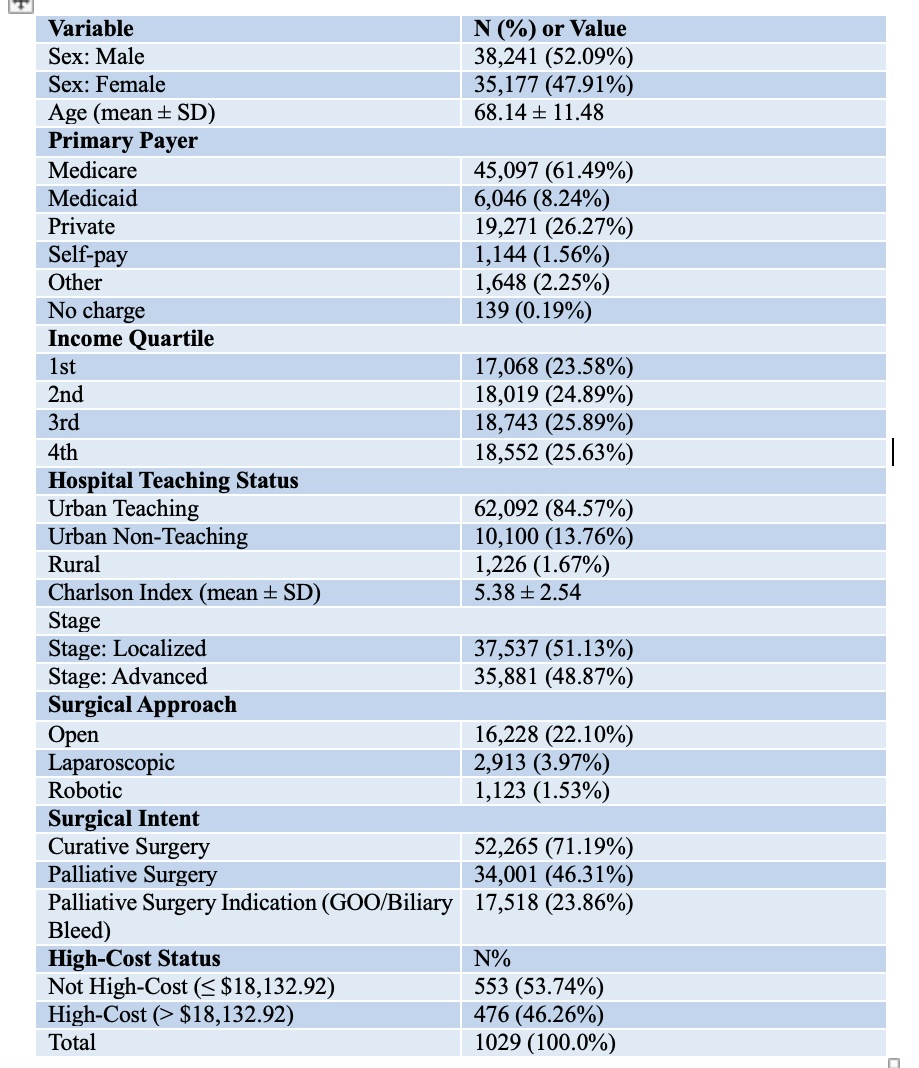
Figure: Table 2. Bivariate Comparison of High Cost Versus Non-High Cost Groups. Table 3. Primary Reasons for 30-day Unplanned Readmissions.
Disclosures:
Nehemias Guevara Rodriguez indicated no relevant financial relationships.
Iqra Arshad indicated no relevant financial relationships.
Ronald Blanco Montecino indicated no relevant financial relationships.
Noemy Coreas indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Wissam Kiwan indicated no relevant financial relationships.
Nehemias Guevara Rodriguez, MD1, Iqra Arshad, MD, MPH1, Ronald Blanco Montecino, MD2, Noemy Coreas, MD3, Mahmoud Y. Madi, MD4, Wissam Kiwan, MD1. P2170 - Predictors of High-Cost Unplanned Readmissions After Curative Surgery for Localized Pancreatic Cancer: A Nationwide Analysis of Surgical Approach, Complications, and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
