Monday Poster Session
Category: Biliary/Pancreas
P2293 - Diabetic Ketoacidosis, Hypertriglyceridemia, and Acute Pancreatitis: A Rare but Potentially Fatal Triad Complicated by Pancreatic Pseudocyst
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Shu-Yen Emily Chan, MD (she/her/hers)
Weiss Memorial Hospital
Nashville, TN
Presenting Author(s)
Emily Shu-Yen Chan, MD1, Ayat Alhakeem, MD1, Natchaya Polpichai, MD2, Allen Cho, MD1, Yusuf Hussein. Kebato, MD1
1Weiss Memorial Hospital, Chicago, IL; 2Division of gastroenterology/hepatology, Medical College of Georgia at Augusta University, Chicago, IL
Introduction: High triglyceride induced acute pancreatitis (HTGP) is a well-known cause of acute pancreatitis (AP), with severity correlating to hypertriglyceridemia. Concurrent HTGP and DKA in a patient without prior diabetes is rare. We present a case of high TG levels exceeding 5,000 mg/dL, new-onset concurrent DKA complicated by AP and a pancreatic pseudocyst.
Case Description/
Methods: A 33‑year‑old obese (BMI 33) man with no medical history presented with three‑day of worsening, intermittent 10/10 epigastric pain, with multiple episodes of non‑bloody, non‑bilious emesis. He also reported polydipsia and nocturia ( > 20 voids/night). On examination, he was tachycardia (HR 122), afebrile, and in moderate distress. Abdominal exam revealed epigastric tenderness without rebound or guarding. Initial laboratory studies: WBC: 27.4K, bicarbonate:< 4, anion gap: 20, glucose: 399, Ca:8.5, Creatine: 1.71, lipase 193, TG >5680, cholesterol: 569, unable to detect LDH, β‑hydroxybutyrate: 6.93, HbA1c: 11%, osmolarity:315. ABG pH: 7.06, CO2:12, O2:112, bicarbonate: 3.3, lactate 2.8.Contrast‑enhanced CT showed acute pancreatitis with peripancreatic inflammation, diffuse hepatic steatosis, and a 10.8 × 9.7 cm low‑attenuation lesion in the pancreatic tail consistent with a pseudocyst.
The patient was diagnosed with HTGP and DKA and admitted to the ICU. He received aggressive IV hydration, an insulin infusion per DKA protocol, and serial monitoring of CMP (q4 hr) and TG (q12 hr). Empiric antibiotics and opioid analgesia were initiated. Plasmapheresis was considered but deferred as TG values decreased to 2,840, then 1,354 on day 2, and 451 mg/dL on day 3, with closure of the anion gap and bicarbonate rising to18. Surgical and IR teams recommended outpatient pseudocyst follow‑up. A post‑DKA C‑peptide of 1.1 ng/mL suggested underlying T2DM. On hospital day 6, repeat CT: a markedly reduced pseudocyst (1.1 ×1.0 cm), despite worsening peripancreatic inflammation with increased free fluid. Lipase decreased to 126 U/L. Upon clinical improvement, the patient was discharged on a basal‑bolus insulin, fenofibrate, atorvastatin, and a strict low‑fat diet.
Discussion: Pancreatic pseudocysts usually develop more than four weeks after acute pancreatitis. Per AGA guidelines, most resolve spontaneously with conservative management. In our case, a pseudocyst formed during the acute phase but regressed as inflammation subsided without intervention. Broad-spectrum antibiotics were administered because walled‑off necrosis could not be excluded.
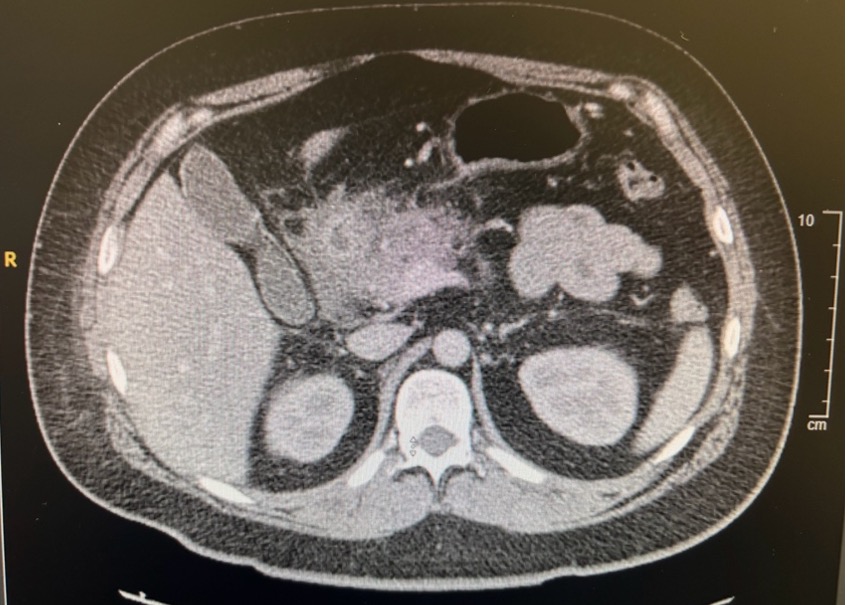
Figure: Figure 1. Day 1 CT abdomen+pelvic with IV contrast
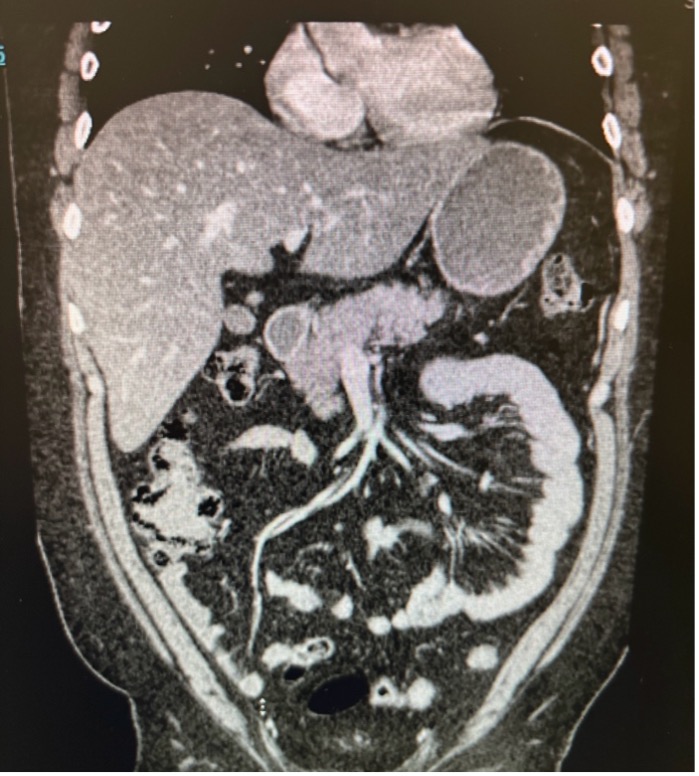
Figure: Figure 2. Day 6 repeat CT abdomen+pelvic with IV contrast
Disclosures:
Emily Shu-Yen Chan indicated no relevant financial relationships.
Ayat Alhakeem indicated no relevant financial relationships.
Natchaya Polpichai indicated no relevant financial relationships.
Allen Cho indicated no relevant financial relationships.
Yusuf Kebato indicated no relevant financial relationships.
Emily Shu-Yen Chan, MD1, Ayat Alhakeem, MD1, Natchaya Polpichai, MD2, Allen Cho, MD1, Yusuf Hussein. Kebato, MD1. P2293 - Diabetic Ketoacidosis, Hypertriglyceridemia, and Acute Pancreatitis: A Rare but Potentially Fatal Triad Complicated by Pancreatic Pseudocyst, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Weiss Memorial Hospital, Chicago, IL; 2Division of gastroenterology/hepatology, Medical College of Georgia at Augusta University, Chicago, IL
Introduction: High triglyceride induced acute pancreatitis (HTGP) is a well-known cause of acute pancreatitis (AP), with severity correlating to hypertriglyceridemia. Concurrent HTGP and DKA in a patient without prior diabetes is rare. We present a case of high TG levels exceeding 5,000 mg/dL, new-onset concurrent DKA complicated by AP and a pancreatic pseudocyst.
Case Description/
Methods: A 33‑year‑old obese (BMI 33) man with no medical history presented with three‑day of worsening, intermittent 10/10 epigastric pain, with multiple episodes of non‑bloody, non‑bilious emesis. He also reported polydipsia and nocturia ( > 20 voids/night). On examination, he was tachycardia (HR 122), afebrile, and in moderate distress. Abdominal exam revealed epigastric tenderness without rebound or guarding. Initial laboratory studies: WBC: 27.4K, bicarbonate:< 4, anion gap: 20, glucose: 399, Ca:8.5, Creatine: 1.71, lipase 193, TG >5680, cholesterol: 569, unable to detect LDH, β‑hydroxybutyrate: 6.93, HbA1c: 11%, osmolarity:315. ABG pH: 7.06, CO2:12, O2:112, bicarbonate: 3.3, lactate 2.8.Contrast‑enhanced CT showed acute pancreatitis with peripancreatic inflammation, diffuse hepatic steatosis, and a 10.8 × 9.7 cm low‑attenuation lesion in the pancreatic tail consistent with a pseudocyst.
The patient was diagnosed with HTGP and DKA and admitted to the ICU. He received aggressive IV hydration, an insulin infusion per DKA protocol, and serial monitoring of CMP (q4 hr) and TG (q12 hr). Empiric antibiotics and opioid analgesia were initiated. Plasmapheresis was considered but deferred as TG values decreased to 2,840, then 1,354 on day 2, and 451 mg/dL on day 3, with closure of the anion gap and bicarbonate rising to18. Surgical and IR teams recommended outpatient pseudocyst follow‑up. A post‑DKA C‑peptide of 1.1 ng/mL suggested underlying T2DM. On hospital day 6, repeat CT: a markedly reduced pseudocyst (1.1 ×1.0 cm), despite worsening peripancreatic inflammation with increased free fluid. Lipase decreased to 126 U/L. Upon clinical improvement, the patient was discharged on a basal‑bolus insulin, fenofibrate, atorvastatin, and a strict low‑fat diet.
Discussion: Pancreatic pseudocysts usually develop more than four weeks after acute pancreatitis. Per AGA guidelines, most resolve spontaneously with conservative management. In our case, a pseudocyst formed during the acute phase but regressed as inflammation subsided without intervention. Broad-spectrum antibiotics were administered because walled‑off necrosis could not be excluded.
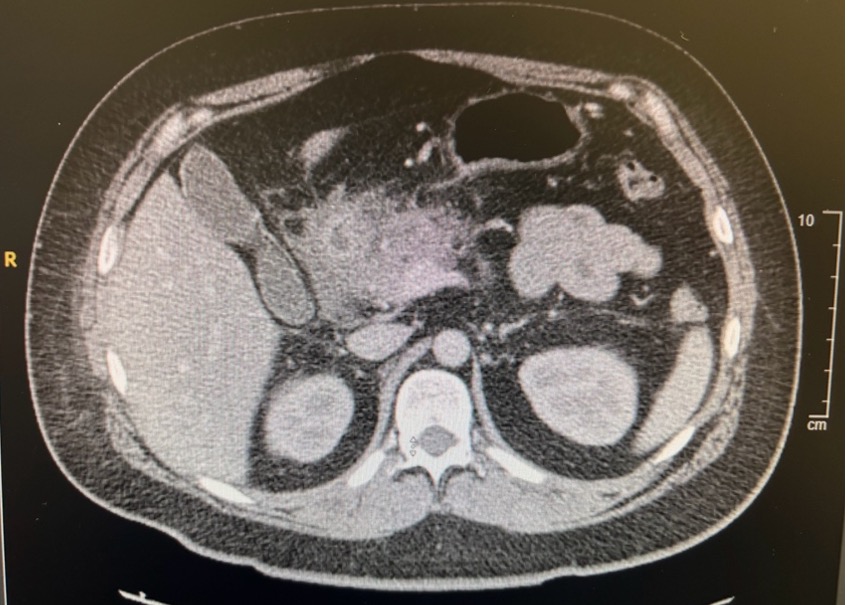
Figure: Figure 1. Day 1 CT abdomen+pelvic with IV contrast
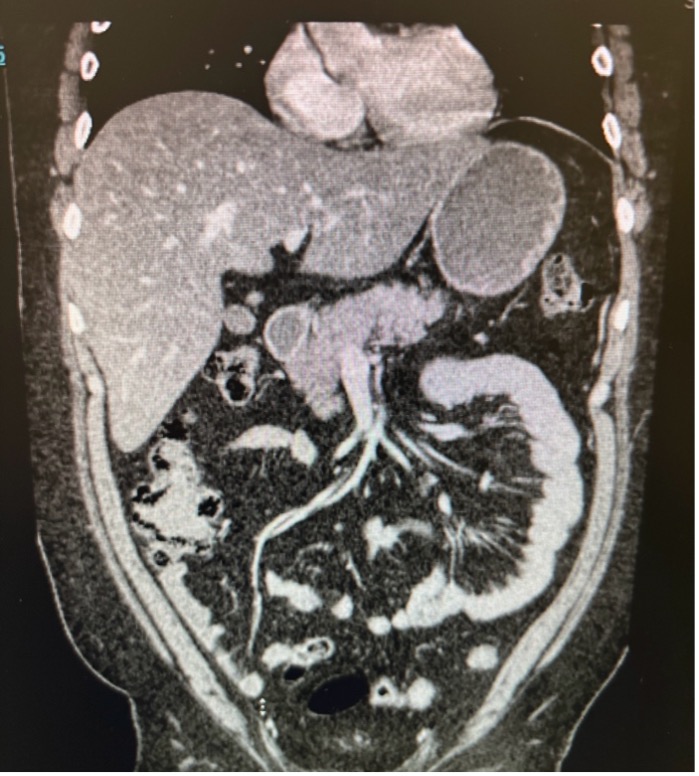
Figure: Figure 2. Day 6 repeat CT abdomen+pelvic with IV contrast
Disclosures:
Emily Shu-Yen Chan indicated no relevant financial relationships.
Ayat Alhakeem indicated no relevant financial relationships.
Natchaya Polpichai indicated no relevant financial relationships.
Allen Cho indicated no relevant financial relationships.
Yusuf Kebato indicated no relevant financial relationships.
Emily Shu-Yen Chan, MD1, Ayat Alhakeem, MD1, Natchaya Polpichai, MD2, Allen Cho, MD1, Yusuf Hussein. Kebato, MD1. P2293 - Diabetic Ketoacidosis, Hypertriglyceridemia, and Acute Pancreatitis: A Rare but Potentially Fatal Triad Complicated by Pancreatic Pseudocyst, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
