Monday Poster Session
Category: Colon
P2404 - Cold vs Hot Endoscopic Mucosal Resection of Large Colorectal Polyps: Findings After Second Surveillance Colonoscopy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- PS
Pranit Sunkara, MD (he/him/his)
Wayne State University School of Medicine / Detroit Medical Center
Detroit, MI
Presenting Author(s)
Pranit Sunkara, MD1, Anshu Wadehra, MD1, Kirthi Lilley, MD2, Samara Rifkin, MD2, Ziad Kanaan, MD, PhD2, Usman Rahim, MD1, Fadi Antaki, MD3
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Wayne State University School of Medicine /John D. Dingell VA Medical Center, Detroit, MI; 3John D. Dingell VA Medical Center & Wayne State University School of Medicine, Detroit, MI
Introduction: Endoscopic mucosal resection (EMR) is an efficient and effective method to remove large colon polyps. EMR can be performed via cautery-assisted (hot) or cold techniques. Prior studies have concluded that hot EMR leads to lower adenoma recurrence rates at first surveillance colonoscopy (SC1) while cold EMR leads to lower adverse event rates. After EMR, close follow-up with surveillance colonoscopy is crucial to monitor for recurrence. Our objective was to assess outcomes of cold versus hot EMR after second surveillance colonoscopy (SC2) at a single academic medical center.
Methods: A retrospective review of all patients who underwent colonoscopy and EMR of large polyps ≥ 1 cm from 2016 to 2023 was conducted. This analysis is limited to the patients who completed follow up with both SC1 and SC2. Data regarding polyp size, histology, removal techniques, adverse events, as well as outcomes after SC2 were obtained. Characteristics of patients with and without a history of recurrent polyp at SC2 were compared using Fisher’s exact test for categorical variables and Kruskal-Wallis test for continuous variables. Predictors of recurrent polyp were derived from unconditional logistic regression model. The final multivariable logistic model was adjusted for age, removal technique, size of index polyp, and histopathology.
Results: Of the 242 polyps included in this analysis, 117 polyps were included in the hot EMR group and 125 polyps were included in the cold EMR group. Time to SC1 was comparable (4.4 months vs. 5.8 months, p=0.6). Overall recurrence rate at SC1 was lower for hot EMR group vs. cold EMR group (19% vs. 34%, p</span>< 0.01). Recurrence at SC1 was endoscopically resected in all cases, using snare (55% in hot, 68% in cold), EMR (9%, 5%), biopsy avulsion (14%, 3%) or combination of snare, biopsy and ablation by cautery (23%, 24%). Time to SC2 was similar between hot and cold EMR groups (18 vs 18 months, p</span> = 0.11). Recurrence rates at SC2 were similar in hot versus cold EMR groups (8.6% vs 11%, p = 0.7). All recurrences were amenable to endoscopic treatment. Increasing patient age and index polyp size correlated with increased recurrence rate at SC2.
Discussion: Our results suggest that despite a higher recurrence rate at SC1 after cold EMR, the recurrence rate for polyps resected by cold EMR is similar to hot EMR at the second surveillance colonoscopy. This provides reassurance that cold EMR is a safe and effective technique for long-term endoscopic management of colonic polyps.
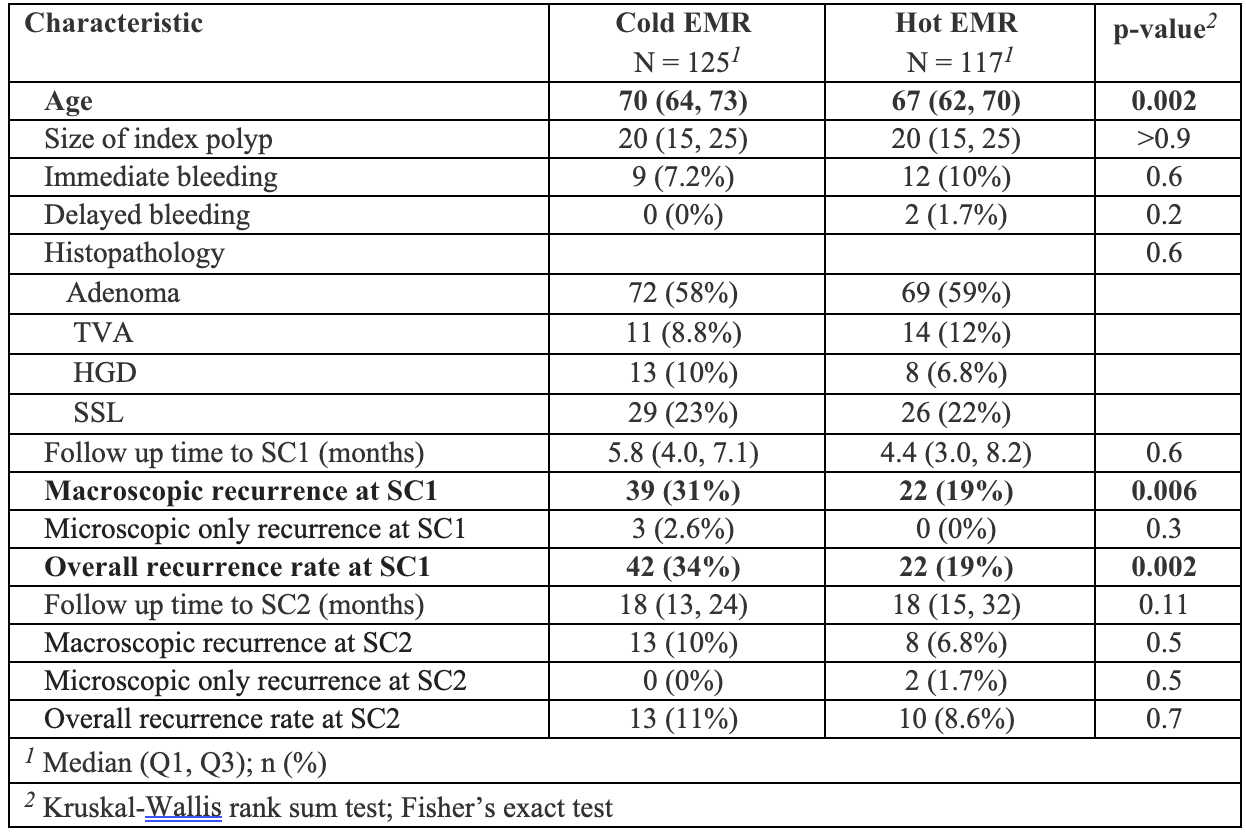
Figure: Table 1. Baseline Characteristics and Outcomes of Hot versus Cold EMR at SC1 and SC2
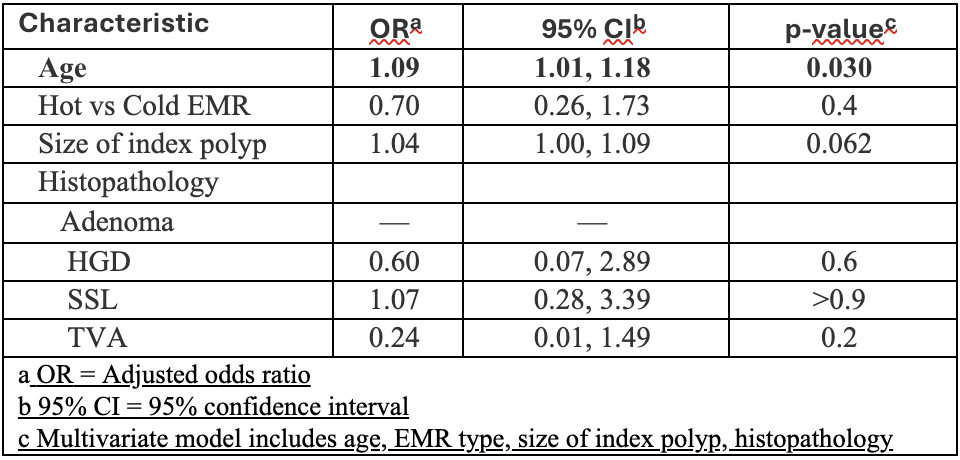
Figure: Table 2. Adjusted Odds Ratios (aORs) for Polyp Recurrence at Second Surveillance
Disclosures:
Pranit Sunkara indicated no relevant financial relationships.
Anshu Wadehra indicated no relevant financial relationships.
Kirthi Lilley indicated no relevant financial relationships.
Samara Rifkin indicated no relevant financial relationships.
Ziad Kanaan indicated no relevant financial relationships.
Usman Rahim indicated no relevant financial relationships.
Fadi Antaki indicated no relevant financial relationships.
Pranit Sunkara, MD1, Anshu Wadehra, MD1, Kirthi Lilley, MD2, Samara Rifkin, MD2, Ziad Kanaan, MD, PhD2, Usman Rahim, MD1, Fadi Antaki, MD3. P2404 - Cold vs Hot Endoscopic Mucosal Resection of Large Colorectal Polyps: Findings After Second Surveillance Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Wayne State University School of Medicine /John D. Dingell VA Medical Center, Detroit, MI; 3John D. Dingell VA Medical Center & Wayne State University School of Medicine, Detroit, MI
Introduction: Endoscopic mucosal resection (EMR) is an efficient and effective method to remove large colon polyps. EMR can be performed via cautery-assisted (hot) or cold techniques. Prior studies have concluded that hot EMR leads to lower adenoma recurrence rates at first surveillance colonoscopy (SC1) while cold EMR leads to lower adverse event rates. After EMR, close follow-up with surveillance colonoscopy is crucial to monitor for recurrence. Our objective was to assess outcomes of cold versus hot EMR after second surveillance colonoscopy (SC2) at a single academic medical center.
Methods: A retrospective review of all patients who underwent colonoscopy and EMR of large polyps ≥ 1 cm from 2016 to 2023 was conducted. This analysis is limited to the patients who completed follow up with both SC1 and SC2. Data regarding polyp size, histology, removal techniques, adverse events, as well as outcomes after SC2 were obtained. Characteristics of patients with and without a history of recurrent polyp at SC2 were compared using Fisher’s exact test for categorical variables and Kruskal-Wallis test for continuous variables. Predictors of recurrent polyp were derived from unconditional logistic regression model. The final multivariable logistic model was adjusted for age, removal technique, size of index polyp, and histopathology.
Results: Of the 242 polyps included in this analysis, 117 polyps were included in the hot EMR group and 125 polyps were included in the cold EMR group. Time to SC1 was comparable (4.4 months vs. 5.8 months, p=0.6). Overall recurrence rate at SC1 was lower for hot EMR group vs. cold EMR group (19% vs. 34%, p</span>< 0.01). Recurrence at SC1 was endoscopically resected in all cases, using snare (55% in hot, 68% in cold), EMR (9%, 5%), biopsy avulsion (14%, 3%) or combination of snare, biopsy and ablation by cautery (23%, 24%). Time to SC2 was similar between hot and cold EMR groups (18 vs 18 months, p</span> = 0.11). Recurrence rates at SC2 were similar in hot versus cold EMR groups (8.6% vs 11%, p = 0.7). All recurrences were amenable to endoscopic treatment. Increasing patient age and index polyp size correlated with increased recurrence rate at SC2.
Discussion: Our results suggest that despite a higher recurrence rate at SC1 after cold EMR, the recurrence rate for polyps resected by cold EMR is similar to hot EMR at the second surveillance colonoscopy. This provides reassurance that cold EMR is a safe and effective technique for long-term endoscopic management of colonic polyps.
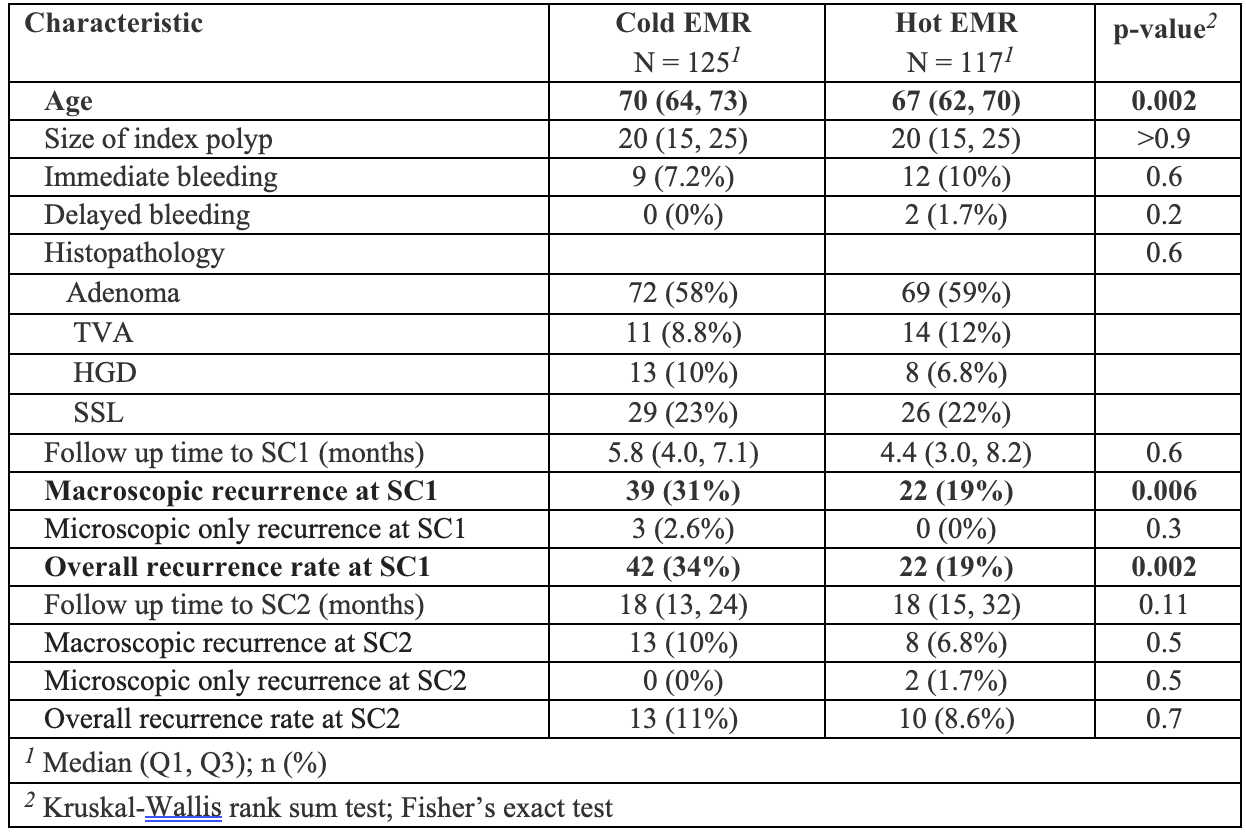
Figure: Table 1. Baseline Characteristics and Outcomes of Hot versus Cold EMR at SC1 and SC2
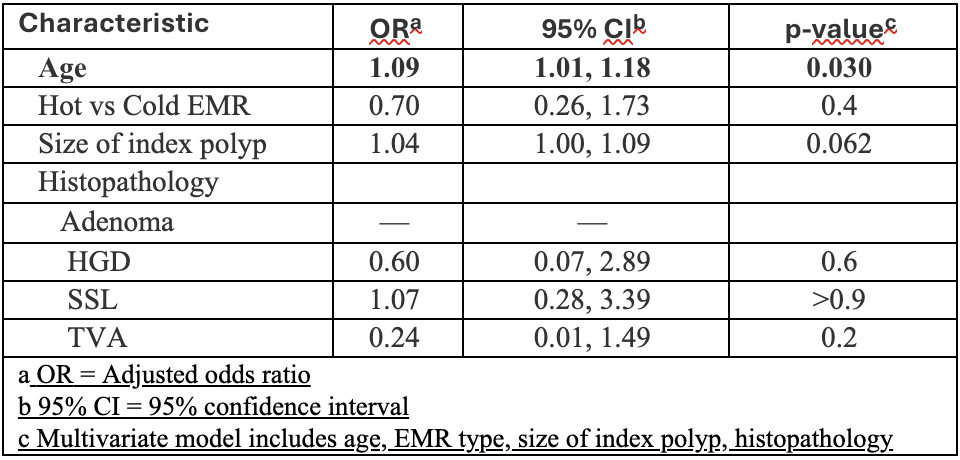
Figure: Table 2. Adjusted Odds Ratios (aORs) for Polyp Recurrence at Second Surveillance
Disclosures:
Pranit Sunkara indicated no relevant financial relationships.
Anshu Wadehra indicated no relevant financial relationships.
Kirthi Lilley indicated no relevant financial relationships.
Samara Rifkin indicated no relevant financial relationships.
Ziad Kanaan indicated no relevant financial relationships.
Usman Rahim indicated no relevant financial relationships.
Fadi Antaki indicated no relevant financial relationships.
Pranit Sunkara, MD1, Anshu Wadehra, MD1, Kirthi Lilley, MD2, Samara Rifkin, MD2, Ziad Kanaan, MD, PhD2, Usman Rahim, MD1, Fadi Antaki, MD3. P2404 - Cold vs Hot Endoscopic Mucosal Resection of Large Colorectal Polyps: Findings After Second Surveillance Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
