Monday Poster Session
Category: Colon
P2402 - Colonic Transit, Breath Test Patterns, and Colectomy Outcomes in Patients With Chronic Constipation Leading to Colectomy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Jane Lim, MD (she/her/hers)
Cedars-Sinai Medical Center
Los Angeles, CA
Presenting Author(s)
Lim Jane, MD1, Jonathan Busam, MD2, Barbara Hollander, MD2, Amrit K. Kamboj, MD1, Nicha Wongjarupong, MD1, Yin Chan, MD2, Bianca Chang, MD2, Ali Rezaie, MD, MSc1, Mark Pimentel, MD, FACG1
1Cedars-Sinai Medical Center, Los Angeles, CA; 2Cedars-Sinai Medical Center, Beverly Hills, CA
Introduction: Colonic inertia, a severe form of slow transit constipation, is medication refractory and often managed with total abdominal colectomy. Factors distinguishing surgical from non-surgical cases of chronic constipation are unclear. While constipation is associated with higher rates of intestinal methanogen overgrowth (IMO), data on rates of IMO in colonic inertia is lacking. The primary aim was to compare colonic transit and rates of IMO in patients with chronic constipation who underwent colectomy vs those managed non-surgically. The secondary aim was to compare outcomes after total vs partial colectomy.
Methods: This retrospective cohort study included adults with chronic constipation who underwent colon transit testing at a tertiary center (Jan 2011-Dec 2023). Data was collected from transit tests, breath tests, anorectal manometry, and MR defecography. Post-colectomy outcomes were based on symptoms and use of constipation drugs ³ 3 months after surgery. IMO was defined as methane ³ 10 ppm. Categorical and continuous variables were analyzed using Chi-square and t-tests, respectively.
Results: We identified 40 subjects with chronic constipation who underwent colectomy (mean age 53.4 ± 17.8 yrs, 95% female) and 299 subjects who underwent colon transit testing but no colectomy (mean age 47.6 ± 16.6 years, 82% female). Groups differed significantly (Table 1). The colectomy group was predominantly female (p=0.004) and white (p=0.015), had more retained sitz markers (16.7 ± 7.7 vs 6.2 ± 8.6, p< 0.001) and higher rates of absent tracer movement on scintigraphy (50% vs 19.2%, p=0.04). The colectomy group had lower rates of IMO (7.7% vs 40.9%, p=0.018). Rates of dyssynergic defecation (33% vs 30%, p=0.71) and structural evacuation disorders (88.2% vs 73.8%, p=0.20) did not differ between groups. Among the colectomy group, 20% had a partial colectomy and all required post-operative constipation agents compared to 26.7% in the total colectomy group (p< 0.001) (Table 2).
Discussion: Patients with chronic constipation who underwent colectomy have distinct features compared to those managed non-surgically. The colectomy group was predominantly white women and had more severe colonic dysmotility based on significantly higher number of retained sitz markers and more frequent absent tracer movement on scintigraphy. Constipation in this group was less often associated with IMO. Total colectomy appears to yield better outcomes than partial colectomy, however larger studies are needed.
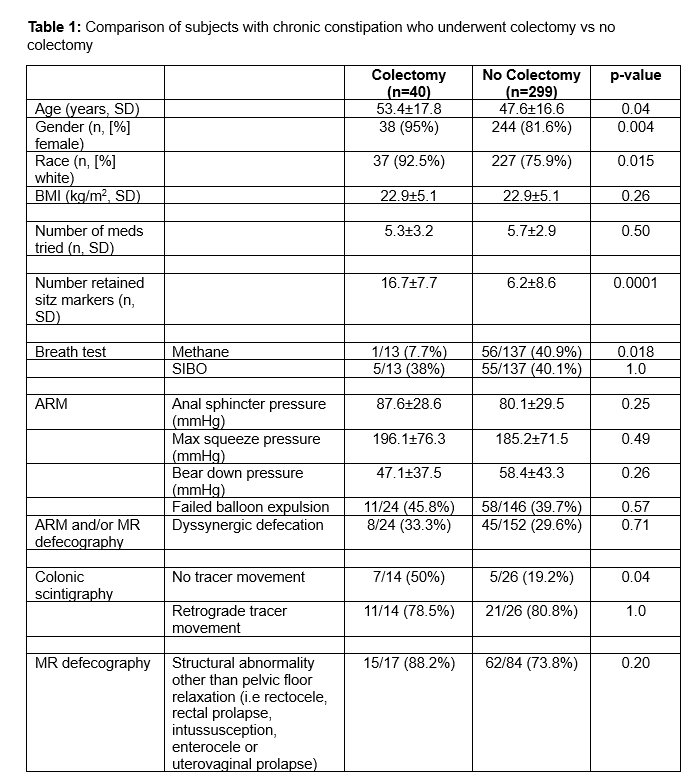
Figure: Table 1: Comparison of subjects with chronic constipation who underwent colectomy vs no colectomy
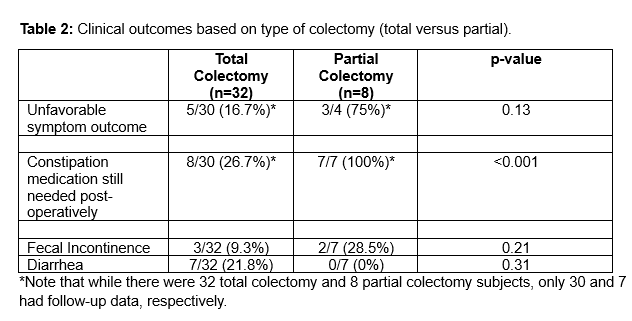
Figure: Table 2: Clinical outcomes based on type of colectomy (total versus partial).
Disclosures:
Lim Jane indicated no relevant financial relationships.
Jonathan Busam indicated no relevant financial relationships.
Barbara Hollander indicated no relevant financial relationships.
Amrit Kamboj: Sanofi – Speakers Bureau.
Nicha Wongjarupong indicated no relevant financial relationships.
Yin Chan indicated no relevant financial relationships.
Bianca Chang indicated no relevant financial relationships.
Ali Rezaie: Ardelyx, Blueprint Medicine and Salix Pharmaceuticals – Consultant. Gemelli Biotech, and Good LFE – Equity stake.
Mark Pimentel: Ardelyx – Consultant. Gemelli Biotech – Advisory Committee/Board Member, Royalties, Stock-privately held company. GoodLFE – Stock-privately held company. Salvo Health, Cylinder Health – Stock Options.
Lim Jane, MD1, Jonathan Busam, MD2, Barbara Hollander, MD2, Amrit K. Kamboj, MD1, Nicha Wongjarupong, MD1, Yin Chan, MD2, Bianca Chang, MD2, Ali Rezaie, MD, MSc1, Mark Pimentel, MD, FACG1. P2402 - Colonic Transit, Breath Test Patterns, and Colectomy Outcomes in Patients With Chronic Constipation Leading to Colectomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cedars-Sinai Medical Center, Los Angeles, CA; 2Cedars-Sinai Medical Center, Beverly Hills, CA
Introduction: Colonic inertia, a severe form of slow transit constipation, is medication refractory and often managed with total abdominal colectomy. Factors distinguishing surgical from non-surgical cases of chronic constipation are unclear. While constipation is associated with higher rates of intestinal methanogen overgrowth (IMO), data on rates of IMO in colonic inertia is lacking. The primary aim was to compare colonic transit and rates of IMO in patients with chronic constipation who underwent colectomy vs those managed non-surgically. The secondary aim was to compare outcomes after total vs partial colectomy.
Methods: This retrospective cohort study included adults with chronic constipation who underwent colon transit testing at a tertiary center (Jan 2011-Dec 2023). Data was collected from transit tests, breath tests, anorectal manometry, and MR defecography. Post-colectomy outcomes were based on symptoms and use of constipation drugs ³ 3 months after surgery. IMO was defined as methane ³ 10 ppm. Categorical and continuous variables were analyzed using Chi-square and t-tests, respectively.
Results: We identified 40 subjects with chronic constipation who underwent colectomy (mean age 53.4 ± 17.8 yrs, 95% female) and 299 subjects who underwent colon transit testing but no colectomy (mean age 47.6 ± 16.6 years, 82% female). Groups differed significantly (Table 1). The colectomy group was predominantly female (p=0.004) and white (p=0.015), had more retained sitz markers (16.7 ± 7.7 vs 6.2 ± 8.6, p< 0.001) and higher rates of absent tracer movement on scintigraphy (50% vs 19.2%, p=0.04). The colectomy group had lower rates of IMO (7.7% vs 40.9%, p=0.018). Rates of dyssynergic defecation (33% vs 30%, p=0.71) and structural evacuation disorders (88.2% vs 73.8%, p=0.20) did not differ between groups. Among the colectomy group, 20% had a partial colectomy and all required post-operative constipation agents compared to 26.7% in the total colectomy group (p< 0.001) (Table 2).
Discussion: Patients with chronic constipation who underwent colectomy have distinct features compared to those managed non-surgically. The colectomy group was predominantly white women and had more severe colonic dysmotility based on significantly higher number of retained sitz markers and more frequent absent tracer movement on scintigraphy. Constipation in this group was less often associated with IMO. Total colectomy appears to yield better outcomes than partial colectomy, however larger studies are needed.
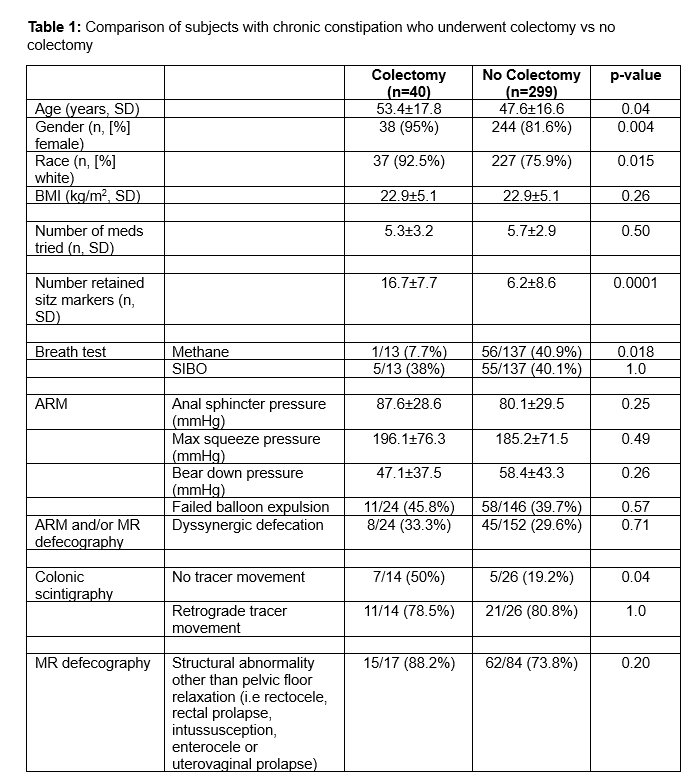
Figure: Table 1: Comparison of subjects with chronic constipation who underwent colectomy vs no colectomy
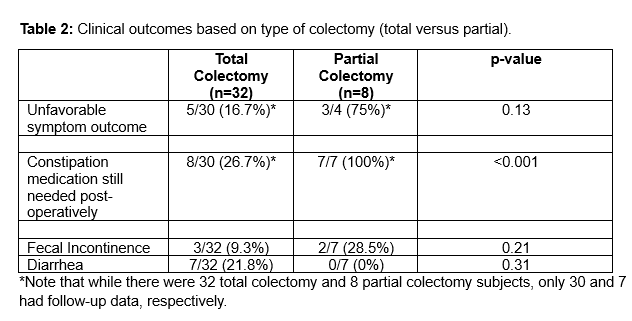
Figure: Table 2: Clinical outcomes based on type of colectomy (total versus partial).
Disclosures:
Lim Jane indicated no relevant financial relationships.
Jonathan Busam indicated no relevant financial relationships.
Barbara Hollander indicated no relevant financial relationships.
Amrit Kamboj: Sanofi – Speakers Bureau.
Nicha Wongjarupong indicated no relevant financial relationships.
Yin Chan indicated no relevant financial relationships.
Bianca Chang indicated no relevant financial relationships.
Ali Rezaie: Ardelyx, Blueprint Medicine and Salix Pharmaceuticals – Consultant. Gemelli Biotech, and Good LFE – Equity stake.
Mark Pimentel: Ardelyx – Consultant. Gemelli Biotech – Advisory Committee/Board Member, Royalties, Stock-privately held company. GoodLFE – Stock-privately held company. Salvo Health, Cylinder Health – Stock Options.
Lim Jane, MD1, Jonathan Busam, MD2, Barbara Hollander, MD2, Amrit K. Kamboj, MD1, Nicha Wongjarupong, MD1, Yin Chan, MD2, Bianca Chang, MD2, Ali Rezaie, MD, MSc1, Mark Pimentel, MD, FACG1. P2402 - Colonic Transit, Breath Test Patterns, and Colectomy Outcomes in Patients With Chronic Constipation Leading to Colectomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
