Monday Poster Session
Category: Colon
P2400 - When Gut Meets Heart: Endocarditis Significantly Worsens Outcomes in Diverticulitis Admissions
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Abdullah Hafeez, MD (he/him/his)
Landmark Medical Center
Woonsocket, RI
Presenting Author(s)
Abdullah Hafeez, MD1, Omar Alkasabrah, MD1, Ritu Tated, MD2, Dhruvi Joshi, MBBS3, Siddharth Agrawal, MD1, Mangesh Kritya, MBBS4, Jatin Thukral, MD1, Hamza Ansari, MD5
1Landmark Medical Center, Woonsocket, RI; 2New York Medical College, New York, NY; 3Narendra Modi Medical College, Ahmedabad, Gujarat, India; 4Houston Methodist Research Institute, Houston, TX; 5NYMC St. Mary's and St. Clare, Denville, NJ
Introduction: Diverticulitis is a prevalent gastrointestinal condition that frequently necessitates hospitalization, particularly among older adults. While the disease typically remains localized, systemic complications can arise, especially in the presence of comorbid conditions. This study aimed to evaluate the impact of concurrent endocarditis on clinical outcomes and healthcare resource utilization in patients hospitalized with diverticulitis.
Methods: We conducted a retrospective cohort analysis using the National Inpatient Sample (NIS) database from 2016 to 2022. Adult patients hospitalized with a primary diagnosis of diverticulitis were identified and stratified based on the presence or absence of a secondary diagnosis of endocarditis. Baseline demographics, comorbidities, hospital characteristics, and outcomes were compared between the two groups. Multivariate logistic regression analyses were performed to assess the independent association of endocarditis with in-hospital mortality, sepsis, septic shock, length of stay (LOS), and total hospital charges, adjusting for potential confounders including age, sex, comorbidity burden, and hospital teaching status.
Results: Among 3,423,274 hospitalizations for diverticulitis, 6,435 (0.19%) had a concurrent diagnosis of endocarditis. Patients with endocarditis were more likely to be male (62.5% vs. 25.2%, p < 0.0001) and had higher rates of comorbid conditions such as chronic kidney disease and coronary artery disease. After adjustment, endocarditis was independently associated with increased odds of in-hospital mortality (OR 2.93; 95% CI, 2.30–3.72; p < 0.0001), sepsis (OR 5.87; 95% CI, 5.22–6.60; p < 0.0001), and septic shock (OR 4.12; 95% CI, 3.39–5.00; p < 0.0001). Additionally, patients with endocarditis had a significantly longer LOS (mean 12.92 vs. 5.33 days; p < 0.0001) and higher total hospital charges (mean $173,925 vs. $66,811; p < 0.0001).
Discussion: In conclusion, the presence of endocarditis in patients hospitalized with diverticulitis is associated with markedly worse clinical outcomes and substantially increased healthcare resource utilization. These findings underscore the importance of early recognition and aggressive management of endocarditis in this patient population. Further research is warranted to develop targeted strategies aimed at improving outcomes and optimizing resource use in patients with coexisting diverticulitis and endocarditis.
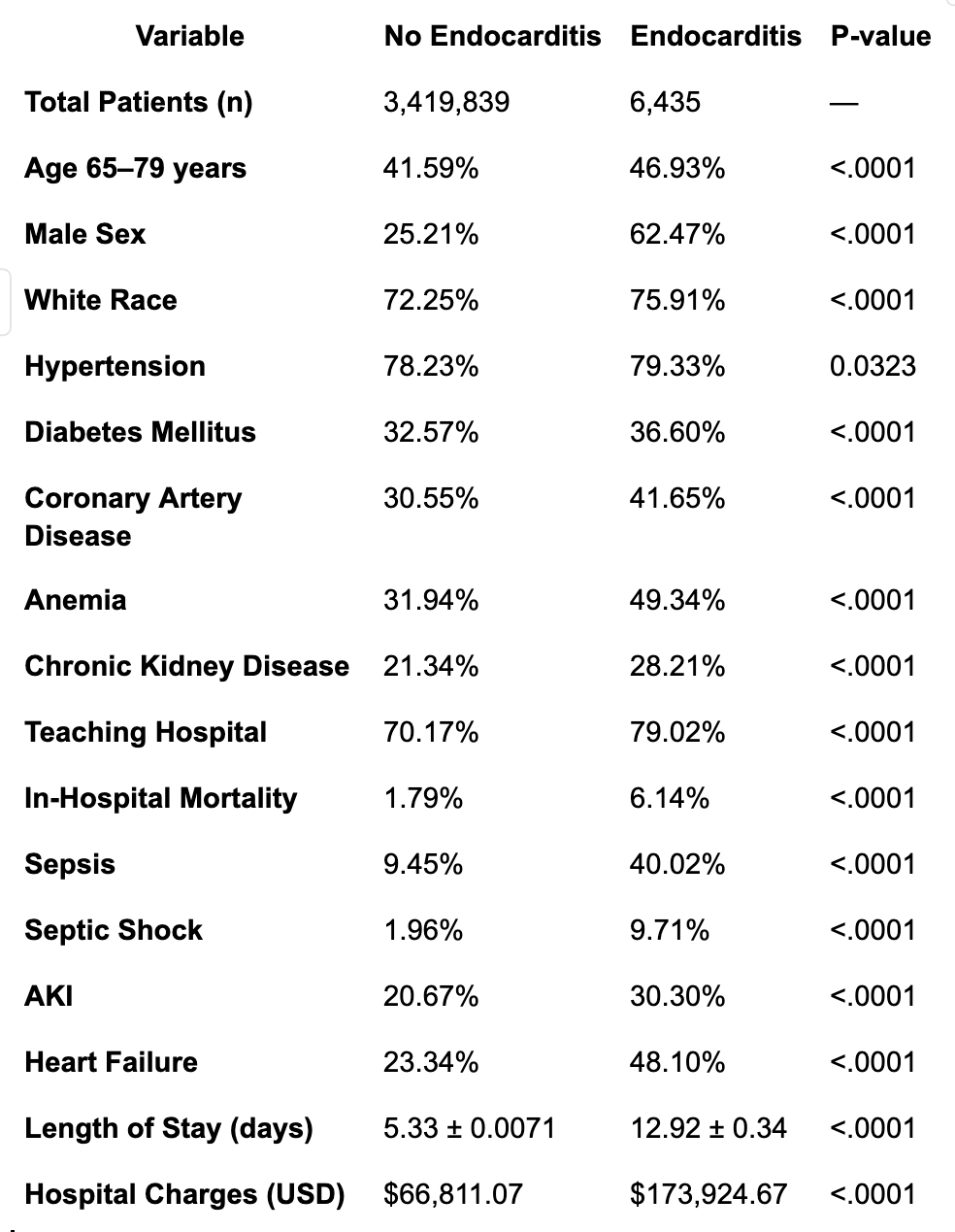
Figure: Table: Baseline Characteristics and Outcomes in Patients with Diverticulitis, Stratified by Endocarditis Status

Figure: Table: Adjusted Odds Ratios for Clinical Outcomes in Diverticulitis Patients with and without Endocarditis (2016–2022)
Disclosures:
Abdullah Hafeez indicated no relevant financial relationships.
Omar Alkasabrah indicated no relevant financial relationships.
Ritu Tated indicated no relevant financial relationships.
Dhruvi Joshi indicated no relevant financial relationships.
Siddharth Agrawal indicated no relevant financial relationships.
Mangesh Kritya indicated no relevant financial relationships.
Jatin Thukral indicated no relevant financial relationships.
Hamza Ansari indicated no relevant financial relationships.
Abdullah Hafeez, MD1, Omar Alkasabrah, MD1, Ritu Tated, MD2, Dhruvi Joshi, MBBS3, Siddharth Agrawal, MD1, Mangesh Kritya, MBBS4, Jatin Thukral, MD1, Hamza Ansari, MD5. P2400 - When Gut Meets Heart: Endocarditis Significantly Worsens Outcomes in Diverticulitis Admissions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Landmark Medical Center, Woonsocket, RI; 2New York Medical College, New York, NY; 3Narendra Modi Medical College, Ahmedabad, Gujarat, India; 4Houston Methodist Research Institute, Houston, TX; 5NYMC St. Mary's and St. Clare, Denville, NJ
Introduction: Diverticulitis is a prevalent gastrointestinal condition that frequently necessitates hospitalization, particularly among older adults. While the disease typically remains localized, systemic complications can arise, especially in the presence of comorbid conditions. This study aimed to evaluate the impact of concurrent endocarditis on clinical outcomes and healthcare resource utilization in patients hospitalized with diverticulitis.
Methods: We conducted a retrospective cohort analysis using the National Inpatient Sample (NIS) database from 2016 to 2022. Adult patients hospitalized with a primary diagnosis of diverticulitis were identified and stratified based on the presence or absence of a secondary diagnosis of endocarditis. Baseline demographics, comorbidities, hospital characteristics, and outcomes were compared between the two groups. Multivariate logistic regression analyses were performed to assess the independent association of endocarditis with in-hospital mortality, sepsis, septic shock, length of stay (LOS), and total hospital charges, adjusting for potential confounders including age, sex, comorbidity burden, and hospital teaching status.
Results: Among 3,423,274 hospitalizations for diverticulitis, 6,435 (0.19%) had a concurrent diagnosis of endocarditis. Patients with endocarditis were more likely to be male (62.5% vs. 25.2%, p < 0.0001) and had higher rates of comorbid conditions such as chronic kidney disease and coronary artery disease. After adjustment, endocarditis was independently associated with increased odds of in-hospital mortality (OR 2.93; 95% CI, 2.30–3.72; p < 0.0001), sepsis (OR 5.87; 95% CI, 5.22–6.60; p < 0.0001), and septic shock (OR 4.12; 95% CI, 3.39–5.00; p < 0.0001). Additionally, patients with endocarditis had a significantly longer LOS (mean 12.92 vs. 5.33 days; p < 0.0001) and higher total hospital charges (mean $173,925 vs. $66,811; p < 0.0001).
Discussion: In conclusion, the presence of endocarditis in patients hospitalized with diverticulitis is associated with markedly worse clinical outcomes and substantially increased healthcare resource utilization. These findings underscore the importance of early recognition and aggressive management of endocarditis in this patient population. Further research is warranted to develop targeted strategies aimed at improving outcomes and optimizing resource use in patients with coexisting diverticulitis and endocarditis.
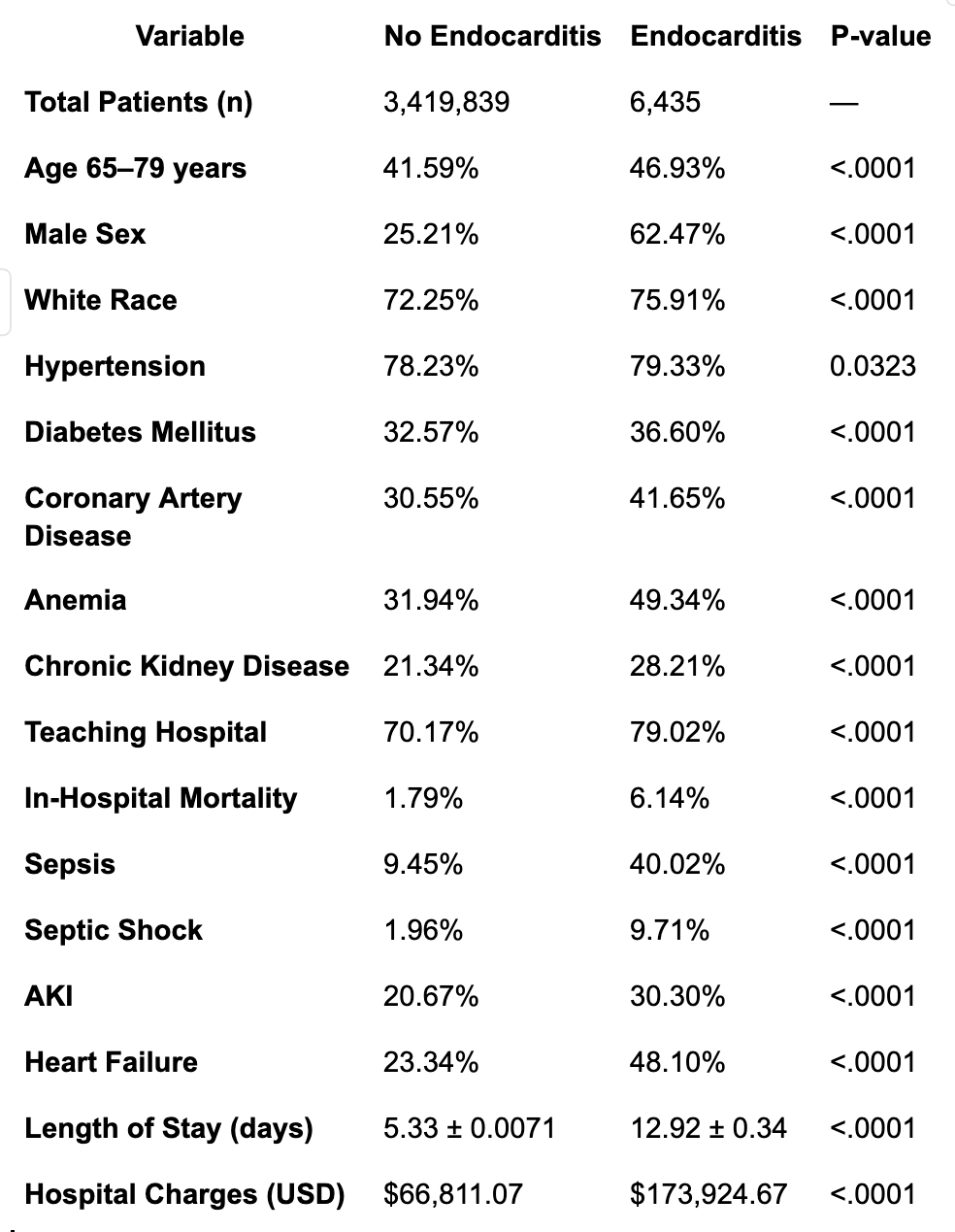
Figure: Table: Baseline Characteristics and Outcomes in Patients with Diverticulitis, Stratified by Endocarditis Status

Figure: Table: Adjusted Odds Ratios for Clinical Outcomes in Diverticulitis Patients with and without Endocarditis (2016–2022)
Disclosures:
Abdullah Hafeez indicated no relevant financial relationships.
Omar Alkasabrah indicated no relevant financial relationships.
Ritu Tated indicated no relevant financial relationships.
Dhruvi Joshi indicated no relevant financial relationships.
Siddharth Agrawal indicated no relevant financial relationships.
Mangesh Kritya indicated no relevant financial relationships.
Jatin Thukral indicated no relevant financial relationships.
Hamza Ansari indicated no relevant financial relationships.
Abdullah Hafeez, MD1, Omar Alkasabrah, MD1, Ritu Tated, MD2, Dhruvi Joshi, MBBS3, Siddharth Agrawal, MD1, Mangesh Kritya, MBBS4, Jatin Thukral, MD1, Hamza Ansari, MD5. P2400 - When Gut Meets Heart: Endocarditis Significantly Worsens Outcomes in Diverticulitis Admissions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

