Monday Poster Session
Category: Biliary/Pancreas
P2388 - When the Brain Meets the Bile: A Rare Case of Ventriculo-Gallbladder Shunt Fistulization
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohamad Omar Diab, MD (he/him/his)
Canyon Vista Medical Center
Sierra Vista, AZ
Presenting Author(s)
Mohamad Omar Diab, MD1, Samuel Cheong, DO2, Brandon Witten, MD2, Jaime Scott, MD2
1Canyon Vista Medical Center, Sierra Vista, AZ; 2Banner - University of Arizona Tucson, Tucson, AZ
Introduction: A cholecystocutaneous fistula—an uncommon pathological communication between the gallbladder and skin—most frequently results from untreated calculous cholecystitis. We present a unique case of cholecystocutaneous fistula complicating a ventriculo-gallbladder (VGB) shunt.
Case Description/
Methods: A 60-year-old male with a history of congenital hydrocephalus status post ventriculoperitoneal (VP) shunt—later revised to a VGB shunt—presented to the emergency department with nausea, vomiting, abdominal pain, fever, and right upper quadrant (RUQ) bilious discharge, raising concern for a cholecystocutaneous fistula and shunt obstruction. A multidisciplinary team, including Neurosurgery, General Surgery, Neurology, Infectious Disease, and Interventional GI, was consulted.
Due to a frozen abdomen, the patient was deemed ineligible for abdominal surgery. Cerebrospinal fluid (CSF) cultures identified Staphylococcus mitis, prompting antibiotic therapy with vancomycin, ceftriaxone, and metronidazole. On 5/12/2025, shunt externalization with ventricular drains was performed. Despite persistent bilious output from a RUQ ostomy, magnetic resonance cholangiopancreatography (MRCP) showed no biliary leak. Contrast-enhanced CT demonstrated retracted ventriculo-cystic shunt tubing herniating through the gallbladder fundus. The retained ventriculo-cystic shunt tubing was surgically removed, and the patient underwent a right parietal endoscopic third ventriculostomy on 5/20/2025. Biliary stenting was considered beneficial after shunt removal, and the patient underwent ERCP on 5/22/2025 with sphincterotomy and placement of one biliary stent in the common bile duct.
The patient was subsequently transferred from the neurosurgical ICU to the medical-surgical floor, with resolution of bilious ostomy output. Outpatient follow-up was arranged for ongoing management.
Discussion: While ventriculo-enteric fistulas have been documented as a complication of VGB shunts, cholecystocutaneous fistulas remain unreported in the literature. Although rare today, patients presenting with RUQ bilious discharge warrant thorough evaluation. Initial management involves drainage and antibiotic therapy, with definitive treatment consisting of open cholecystectomy and excision of the fistulous tract. However, in patients who are too debilitated for surgery, we propose that removing the distal VGB shunt apparatus alongside biliary stenting may reduce biliary flow through the fistula, promoting spontaneous closure.
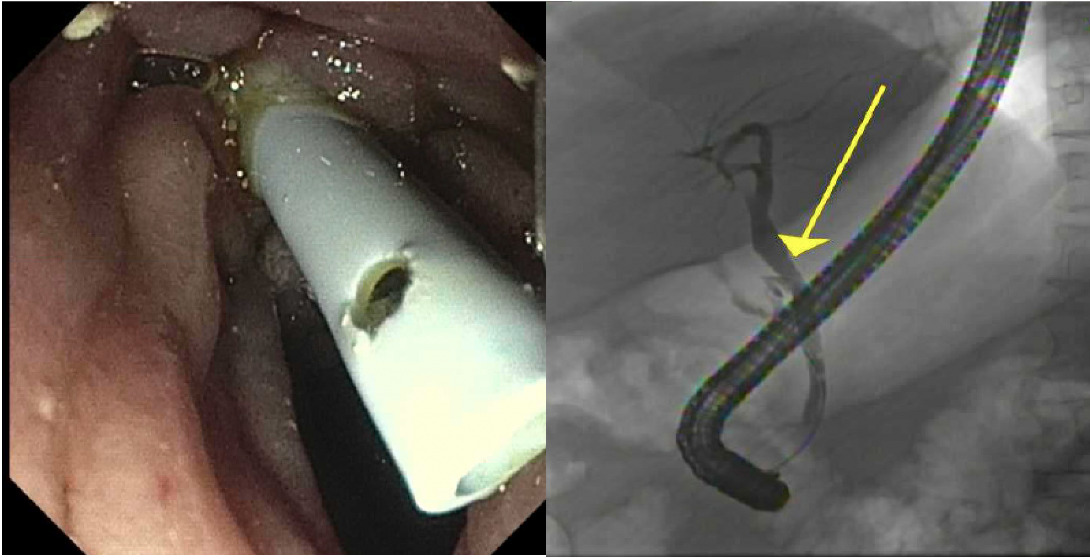
Figure: Image 1: ERCP stent placement.
Disclosures:
Mohamad Omar Diab indicated no relevant financial relationships.
Samuel Cheong indicated no relevant financial relationships.
Brandon Witten indicated no relevant financial relationships.
Jaime Scott indicated no relevant financial relationships.
Mohamad Omar Diab, MD1, Samuel Cheong, DO2, Brandon Witten, MD2, Jaime Scott, MD2. P2388 - When the Brain Meets the Bile: A Rare Case of Ventriculo-Gallbladder Shunt Fistulization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Canyon Vista Medical Center, Sierra Vista, AZ; 2Banner - University of Arizona Tucson, Tucson, AZ
Introduction: A cholecystocutaneous fistula—an uncommon pathological communication between the gallbladder and skin—most frequently results from untreated calculous cholecystitis. We present a unique case of cholecystocutaneous fistula complicating a ventriculo-gallbladder (VGB) shunt.
Case Description/
Methods: A 60-year-old male with a history of congenital hydrocephalus status post ventriculoperitoneal (VP) shunt—later revised to a VGB shunt—presented to the emergency department with nausea, vomiting, abdominal pain, fever, and right upper quadrant (RUQ) bilious discharge, raising concern for a cholecystocutaneous fistula and shunt obstruction. A multidisciplinary team, including Neurosurgery, General Surgery, Neurology, Infectious Disease, and Interventional GI, was consulted.
Due to a frozen abdomen, the patient was deemed ineligible for abdominal surgery. Cerebrospinal fluid (CSF) cultures identified Staphylococcus mitis, prompting antibiotic therapy with vancomycin, ceftriaxone, and metronidazole. On 5/12/2025, shunt externalization with ventricular drains was performed. Despite persistent bilious output from a RUQ ostomy, magnetic resonance cholangiopancreatography (MRCP) showed no biliary leak. Contrast-enhanced CT demonstrated retracted ventriculo-cystic shunt tubing herniating through the gallbladder fundus. The retained ventriculo-cystic shunt tubing was surgically removed, and the patient underwent a right parietal endoscopic third ventriculostomy on 5/20/2025. Biliary stenting was considered beneficial after shunt removal, and the patient underwent ERCP on 5/22/2025 with sphincterotomy and placement of one biliary stent in the common bile duct.
The patient was subsequently transferred from the neurosurgical ICU to the medical-surgical floor, with resolution of bilious ostomy output. Outpatient follow-up was arranged for ongoing management.
Discussion: While ventriculo-enteric fistulas have been documented as a complication of VGB shunts, cholecystocutaneous fistulas remain unreported in the literature. Although rare today, patients presenting with RUQ bilious discharge warrant thorough evaluation. Initial management involves drainage and antibiotic therapy, with definitive treatment consisting of open cholecystectomy and excision of the fistulous tract. However, in patients who are too debilitated for surgery, we propose that removing the distal VGB shunt apparatus alongside biliary stenting may reduce biliary flow through the fistula, promoting spontaneous closure.
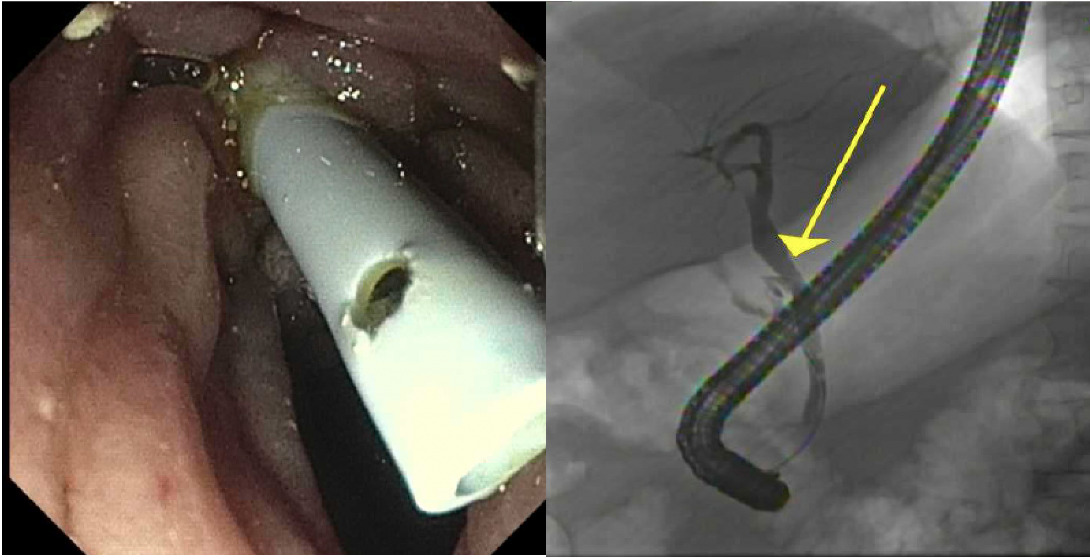
Figure: Image 1: ERCP stent placement.
Disclosures:
Mohamad Omar Diab indicated no relevant financial relationships.
Samuel Cheong indicated no relevant financial relationships.
Brandon Witten indicated no relevant financial relationships.
Jaime Scott indicated no relevant financial relationships.
Mohamad Omar Diab, MD1, Samuel Cheong, DO2, Brandon Witten, MD2, Jaime Scott, MD2. P2388 - When the Brain Meets the Bile: A Rare Case of Ventriculo-Gallbladder Shunt Fistulization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
