Monday Poster Session
Category: Biliary/Pancreas
P2383 - Severe Pancreatitis in Systemic Lupus Erythematosus: A Diagnostic and Therapeutic Challenge
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- GS
Gengqing Song, MD (he/him/his)
Division of Gastroenterology and Hepatology, Metrohealth Medical Center
Cleveland, OH
Presenting Author(s)
Thai Hau Koo, MD1, Venkata Sunkesula, MD2, Mengdan Xie, MD3, Gengqing Song, MD4
1University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3MetroHealth Medical Center, Cleveland, OH; 4Division of Gastroenterology and Hepatology, Metrohealth Medical Center, Cleveland, OH
Introduction: Acute pancreatitis (AP), including lupus-associated pancreatitis (LAP), occurring during lupus flares, is uncommon but may progress to severe necrotizing pancreatitis (NP). The etiologies of AP in lupus patients are complex and often overlap.
Case Description/
Methods: A 27-year-old female with SLE, previously lost to follow-up, presented with fever, anorexia, diffuse myalgia, and right upper quadrant pain. Laboratory findings revealed leukocytosis (16.7 × 10⁹/L), anemia (8.4 g/dL), elevated creatinine (2.28 mg/dL), and lipase (400 U/L). Autoimmune markers confirmed active SLE with ANA (1:320 titer), anti-dsDNA, anti-Smith, and anti-RNP positivity, and low complement levels (C3, 30 mg/dL; C4, < 8 mg/dL). Computed tomography (CT) showed necrotizing pneumonia and an enlarged, edematous pancreas with decreased enhancement, consistent with acute pancreatitis [Fig. 1]. The initial treatment included high-dose intravenous methylprednisolone (1000 mg), hydroxychloroquine (200 mg daily), and empiric antibiotics for pneumonia. MRCP excluded obstruction and revealed a large necrotic peripancreatic fluid collection [Fig. 2]. The patient’s condition deteriorated in the ICU, requiring mechanical ventilation and norepinephrine for hemodynamic support. Negative cultures led to the discontinuation of empiric antibiotics. Despite steroids and mycophenolate mofetil, the persistent symptoms prompted therapeutic plasma exchange (TPE). Following five sessions of TPE, her clinical status improved, with resolution of respiratory failure, stabilization of renal function, and discharge to a rehabilitation facility. Follow-up imaging revealed a small pseudocyst without signs of AP [Fig. 3].
Discussion: AP in SLE presents a diagnostic dilemma, especially when features of lupus flare and AP overlap. In this case, no definitive etiology could be confirmed, but the severity of the illness necessitated prompt intervention. Owing to the patient’s rapid clinical decline, we initiated high-dose corticosteroids, hydroxychloroquine, and empiric antibiotics without delay. Despite standard immunosuppressive therapy, her condition deteriorated, prompting escalation to TPE. The patient’s marked clinical improvement after TPE suggests a potential benefit in refractory cases, although its precise role requires further investigation. This case underscores the importance of early empirical treatment in critically ill patients with suspected LAP, even in the absence of diagnostic certainty.
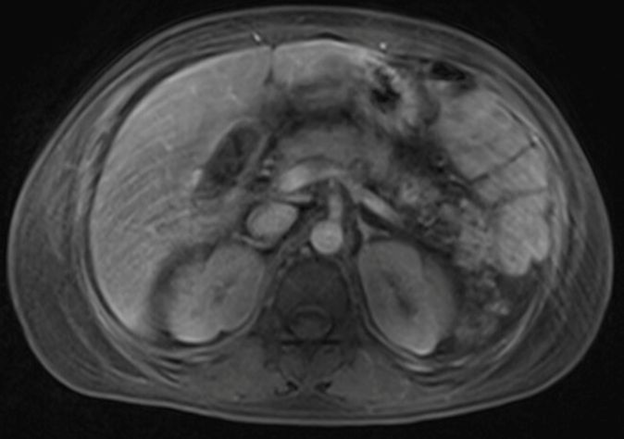
Figure: Figure 1A. CT of the abdomen and pelvis with contrast showed an edematous pancreas with decreased enhancement at the tail of the pancreas, consistent with acute pancreatitis. Figure 1B. A follow-up CT of the abdomen and pelvis with contrast showed a pancreatic pseudocyst with no evidence of acute pancreatitis.
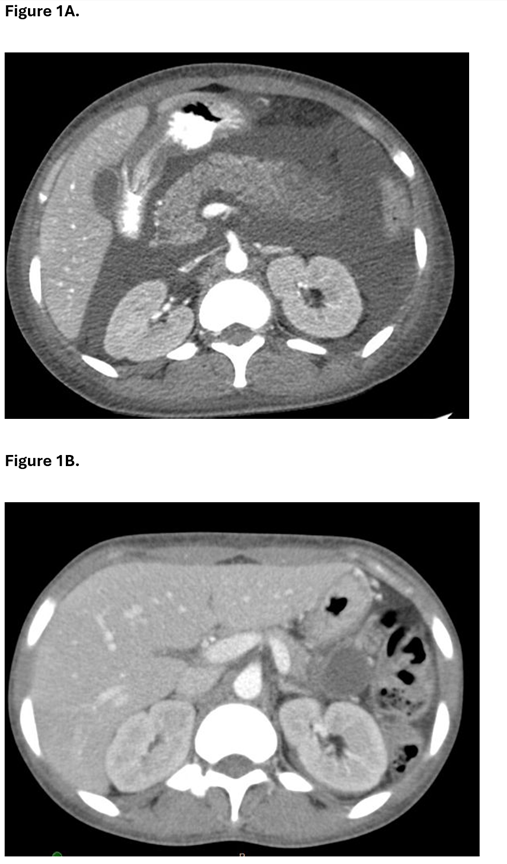
Figure: Figure 2. MRCP with and without contrast showed peripancreatic fluid consistent with acute necrotic fluid collection.
Disclosures:
Thai Hau Koo indicated no relevant financial relationships.
Venkata Sunkesula indicated no relevant financial relationships.
Mengdan Xie indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Thai Hau Koo, MD1, Venkata Sunkesula, MD2, Mengdan Xie, MD3, Gengqing Song, MD4. P2383 - Severe Pancreatitis in Systemic Lupus Erythematosus: A Diagnostic and Therapeutic Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3MetroHealth Medical Center, Cleveland, OH; 4Division of Gastroenterology and Hepatology, Metrohealth Medical Center, Cleveland, OH
Introduction: Acute pancreatitis (AP), including lupus-associated pancreatitis (LAP), occurring during lupus flares, is uncommon but may progress to severe necrotizing pancreatitis (NP). The etiologies of AP in lupus patients are complex and often overlap.
Case Description/
Methods: A 27-year-old female with SLE, previously lost to follow-up, presented with fever, anorexia, diffuse myalgia, and right upper quadrant pain. Laboratory findings revealed leukocytosis (16.7 × 10⁹/L), anemia (8.4 g/dL), elevated creatinine (2.28 mg/dL), and lipase (400 U/L). Autoimmune markers confirmed active SLE with ANA (1:320 titer), anti-dsDNA, anti-Smith, and anti-RNP positivity, and low complement levels (C3, 30 mg/dL; C4, < 8 mg/dL). Computed tomography (CT) showed necrotizing pneumonia and an enlarged, edematous pancreas with decreased enhancement, consistent with acute pancreatitis [Fig. 1]. The initial treatment included high-dose intravenous methylprednisolone (1000 mg), hydroxychloroquine (200 mg daily), and empiric antibiotics for pneumonia. MRCP excluded obstruction and revealed a large necrotic peripancreatic fluid collection [Fig. 2]. The patient’s condition deteriorated in the ICU, requiring mechanical ventilation and norepinephrine for hemodynamic support. Negative cultures led to the discontinuation of empiric antibiotics. Despite steroids and mycophenolate mofetil, the persistent symptoms prompted therapeutic plasma exchange (TPE). Following five sessions of TPE, her clinical status improved, with resolution of respiratory failure, stabilization of renal function, and discharge to a rehabilitation facility. Follow-up imaging revealed a small pseudocyst without signs of AP [Fig. 3].
Discussion: AP in SLE presents a diagnostic dilemma, especially when features of lupus flare and AP overlap. In this case, no definitive etiology could be confirmed, but the severity of the illness necessitated prompt intervention. Owing to the patient’s rapid clinical decline, we initiated high-dose corticosteroids, hydroxychloroquine, and empiric antibiotics without delay. Despite standard immunosuppressive therapy, her condition deteriorated, prompting escalation to TPE. The patient’s marked clinical improvement after TPE suggests a potential benefit in refractory cases, although its precise role requires further investigation. This case underscores the importance of early empirical treatment in critically ill patients with suspected LAP, even in the absence of diagnostic certainty.
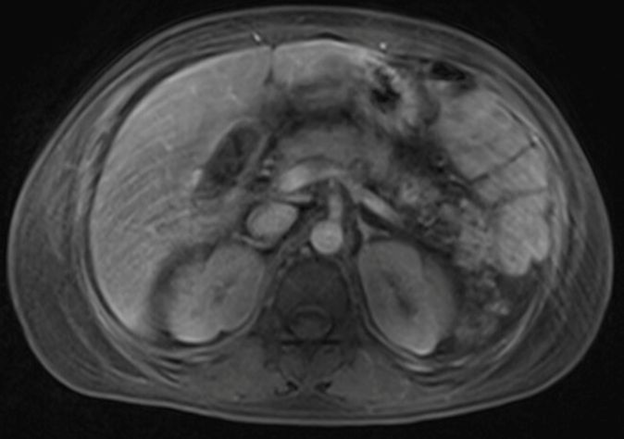
Figure: Figure 1A. CT of the abdomen and pelvis with contrast showed an edematous pancreas with decreased enhancement at the tail of the pancreas, consistent with acute pancreatitis. Figure 1B. A follow-up CT of the abdomen and pelvis with contrast showed a pancreatic pseudocyst with no evidence of acute pancreatitis.
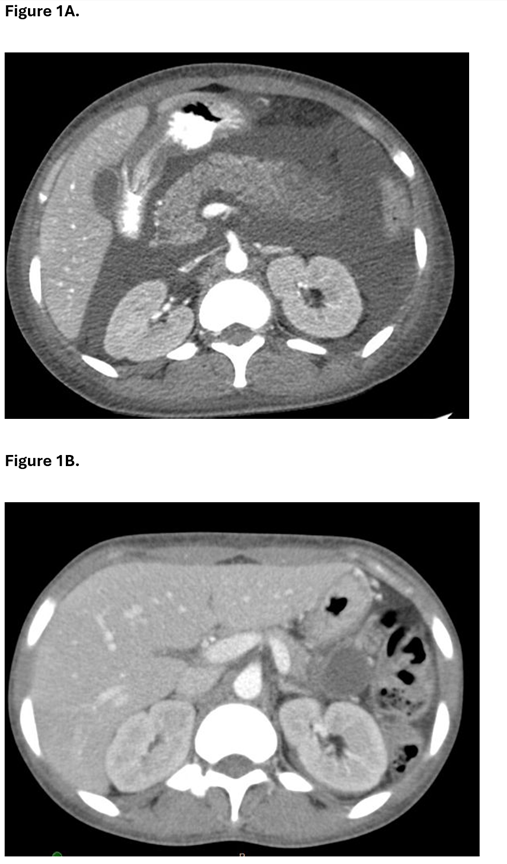
Figure: Figure 2. MRCP with and without contrast showed peripancreatic fluid consistent with acute necrotic fluid collection.
Disclosures:
Thai Hau Koo indicated no relevant financial relationships.
Venkata Sunkesula indicated no relevant financial relationships.
Mengdan Xie indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Thai Hau Koo, MD1, Venkata Sunkesula, MD2, Mengdan Xie, MD3, Gengqing Song, MD4. P2383 - Severe Pancreatitis in Systemic Lupus Erythematosus: A Diagnostic and Therapeutic Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
