Monday Poster Session
Category: Colon
P2571 - Familial Adenomatous Polyposis Complicated by Immune Thrombocytopenia and Intestinal Malrotation

Sebastian Hermida Velasquez, DO
Palmetto General Hospital
Miami, FL
Presenting Author(s)
1Palmetto General Hospital, Hialeah, FL; 2Larkin Community Hospital, Hialeah, FL; 3Larkin Community Hospital, Miami, FL; 4Larkin Community Hospital, South Miami, FL; 5University of Miami Miller School of Medicine at Jackson Memorial Hospital, Miami, FL
Introduction: Familial adenomatous polyposis (FAP) is an autosomal dominant condition described by extreme colorectal polyposis and high risk of malignancy if left untreated. Colectomy remains a form of definitive treatment with some patients experiencing complications such as bleeding, bowel obstruction, or even extraintestinal manifestations. We present a case of FAP in a young Haitian male, complicated by immune thrombocytopenia (ITP) and intestinal malrotation, highlighting the diagnostic and therapeutic challenges of such high-risk patients.
Case Description/
Methods:
A 28-year-old Haitian male with no prior medical history presented with three weeks of hematochezia, weakness, abdominal pain and palpitations. On admission, labs revealed severe anemia (hemoglobin 3.3 g/dL) with thrombocytopenia (platelets 17,000/µL). The patient was directly admitted under ICU care and started on massive transfusion protocol. Hematological workup revealed patient meeting ITP criteria, subsequently started on high-dose steroids and IVIG. Given abdominal pain and hematochezia, CT imaging was obtained and revealed intestinal malrotation noted by an inverse superior mesenteric artery (SMA) and vein (SMV) relationship. Throughout the course of his hospitalization, the patient underwent colonoscopy revealing hundreds of polyps (5–20 mm) with two suspicious masses (ascending and sigmoid colon), biopsied as tubular adenomas; genetic testing confirming FAP. After hematologic stabilization, the patient underwent laparoscopic total colectomy with ileorectal anastomosis. However, his postoperative course was complicated by a closed-loop small bowel obstruction secondary to adhesions and malrotation. He required an emergent laparotomy with small bowel resection and diverting loop ileostomy and continued recovery in the ICU. This case represents an extremely rare convergence of FAB, ITP, and intestinal malrotation. These three conditions occurring in this situation posed significant treatment and diagnostic challenges. ITP exacerbated bleeding risk from extensive polyposis but also complicated preoperative planning. Underlying intestinal malrotation added an unexpected anatomic hurdle to GI and surgical interventions. What was initially a straightforward case of lower GI bleeding unraveled into a complex case requiring multidisciplinary cooperation. This case aims to be cautionary about the unpredictable nature of genetic syndromes and emphasizes the need for individualized approaches in patients with multiple comorbidities.
Discussion: 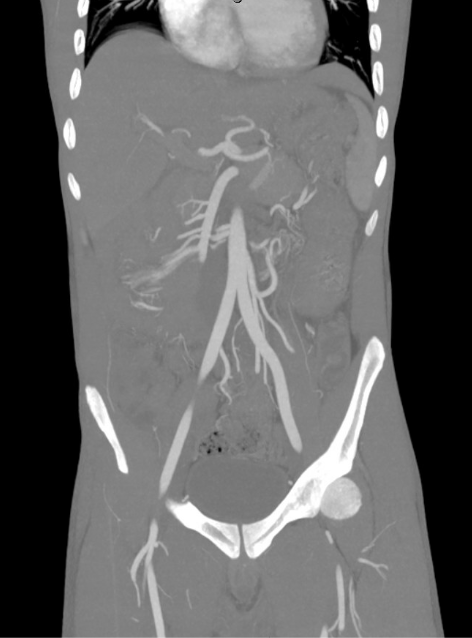
Figure: Figure 1.0: Contrast-enhanced CT abdomen reveals intestinal malrotation with characteristic inversion of the SMA (superior mesenteric artery) and IMV (inferior mesenteric vein) relationship, demonstrating left-sided colonic positioning. Notably absent is contrast extravasation, excluding active hemorrhage as the source of this FAP patient's hematochezia - an important distinction guiding management.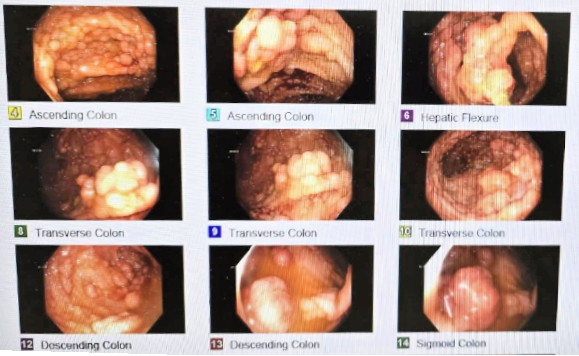
Figure: Figure 2.0: Pan-colonic polyposis in familial adenomatous polyposis (FAP); Endoscopic visualization of innumerable sessile and pedunculated polyps (5-20 mm) carpeting the colonic mucosa.
Disclosures:
Sebastian Hermida Velasquez indicated no relevant financial relationships.
Abelardo Broceta-Martinez indicated no relevant financial relationships.
Thatcher Huynh indicated no relevant financial relationships.
Joseph Caravella indicated no relevant financial relationships.
Natalia Martin indicated no relevant financial relationships.
Carlos Ramos Pachon indicated no relevant financial relationships.
William Rengifo indicated no relevant financial relationships.
Sebastian Hermida Velasquez, DO1, Abelardo Broceta-Martinez, MD2, Thatcher T. Huynh, DO2, Joseph W.. Caravella, DO3, Natalia Martin, DO4, Carlos M.. Ramos Pachon, MD5, William Rengifo, MD5. P2571 - Familial Adenomatous Polyposis Complicated by Immune Thrombocytopenia and Intestinal Malrotation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
