Monday Poster Session
Category: Colorectal Cancer Prevention
P2662 - Current Dismorphisms of Rural and Urban Colon Cancer Screenings
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Gloria Erazo, MD (she/her/hers)
Texas Tech University
Odessa, TX
Presenting Author(s)
Gloria Erazo, MD1, Ooreoluwa Fasola, MD2, Jorge Rodriguez, MD3, Ahmed Bashir Sukhera, MD2, Daniel Guifarro Rivera, MD4, Romelia A. Barba Bernal, MD5, John Garza, PhD3, Kalyan Chakrala, DO2
1Texas Tech University, Odessa, TX; 2Texas Tech University Health Sciences Center, Odessa, TX; 3Texas Tech University Health Sciences Center - Permian Basin, Odessa, TX; 4Cook County Health and Hospital Systems, Chicago, IL; 5Texas Tech University Health Sciences Center, Lubbock, TX
Introduction: Colorectal cancer (CRC) is the fourth most common cancer by incidence in the US. Although overall rates have declined there are notable disparities, with rural populations experiencing higher cancer incidence and mortality rates compared to urban areas. We aimed to examine how social factors in different areas affect CRC screening.
Methods: The study analyzed colon cancer screening rates in Texas for residents aged 45–74 in 2021 using statewide data. Screenings were identified via CPT and HCPCS codes. Population estimates by age group and county were obtained from SEER, and counties were classified as urban (≥50,000) or rural (< 50,000) based on the 2013 NCHS Urban-Rural Classification. Age-adjusted screening rates (AASRs) per 100,000 were calculated using the 2000 U.S. standard population. Confidence intervals were estimated using the standard error formula (AASR divided by the square root of the number of screenings), and differences between rural and urban areas were assessed by comparing 95% confidence intervals. Subgroup analyses were conducted by age, sex, and race/ethnicity.
Results: We included 7,080,602 residents, 841,312 (11.9%) lived in rural areas. A total of 494,437 CRC screenings were identified with 42,612 (8.6%) for rural residents and 451,825 (91.4%) for urban. The overall statewide AASR was 6071.5 (95% CI 6054.6 to 6088.4). The urban AASR 6297.0 (95% CI 6278.6 to 6315.3) was substantially greater than the rural AASR 4182.7 (95% CI 4143.0 to 4222.4). Out of 172 rural counties, 160 (93.0%) had AASR below the statewide AASR. The association of rural residence and AASR remained consistent within each of the examined subgroups. Within rural areas, females had higher AASR than males and Whites had substantially higher AASR compared to other races. The highest rate was measured for urban whites AASR 7039.1 (95% CI 7012.0 to 7066.2) while the lowest rate was for rural Native Americans AASR 471.8 (95% CI 308.3 to 635.2).
Discussion: There is a significant disparity in CRC screening rates between urban and rural populations in Texas, with rural areas showing lower screening rates. The findings emphasize the need for targeted efforts to improve screening access and rates in rural communities. Improving survival rates for CRC may be achieved through collaboration among healthcare providers, patients, and communities to increase awareness and early detection.
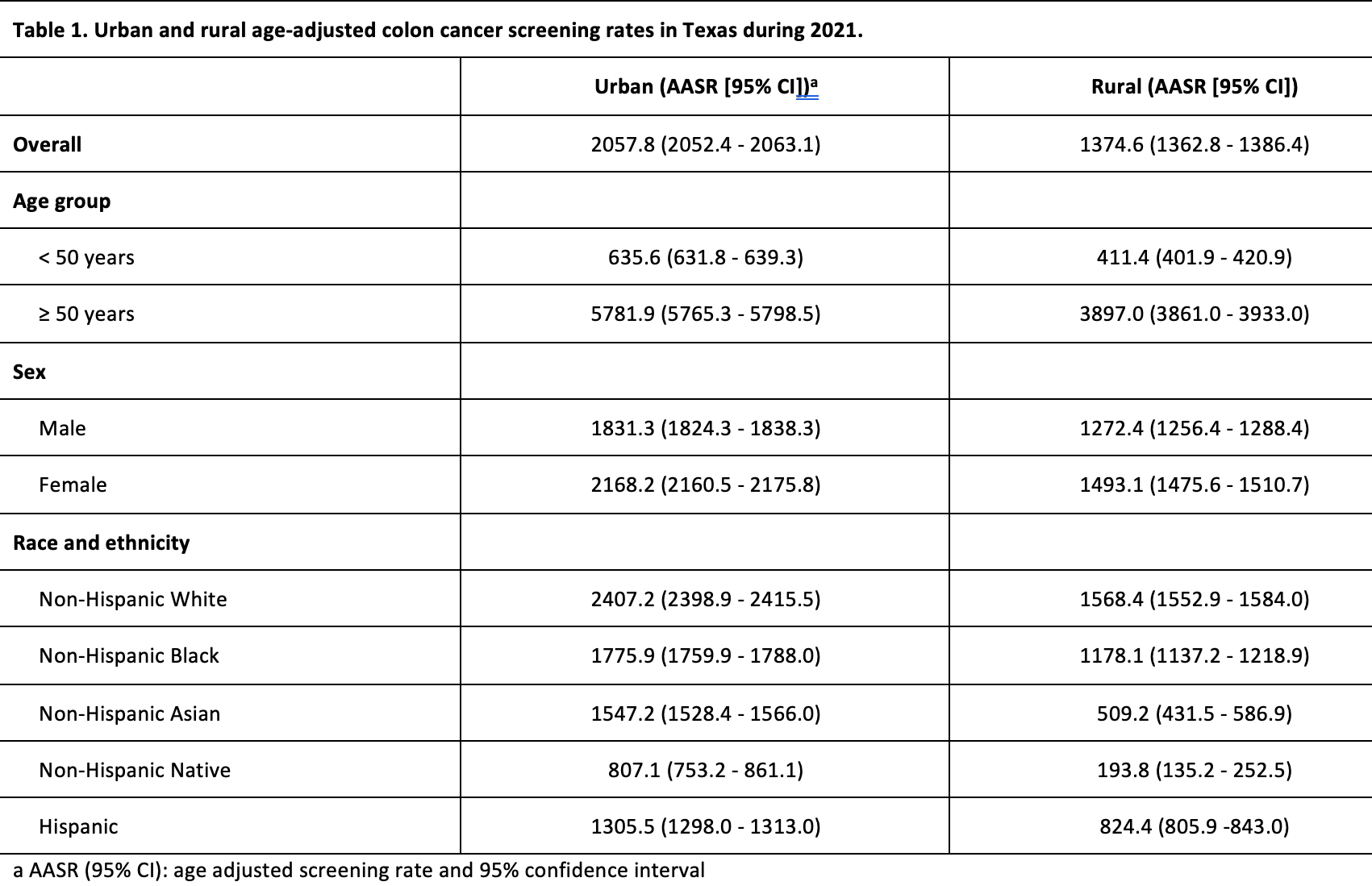
Figure: Urban and rural age-adjusted CRC screening rates in Texas during 2021.
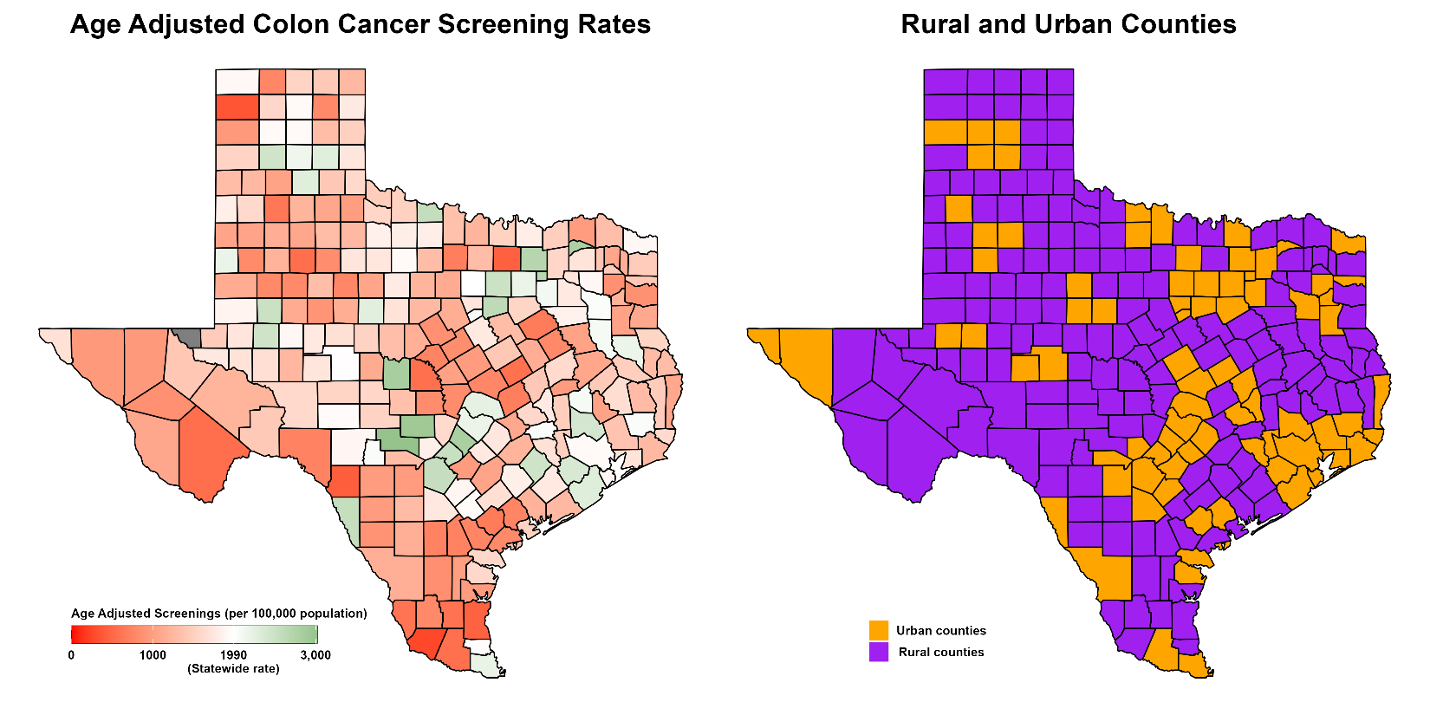
Figure: Urban and rural age-adjusted CRC screening rates in Texas during 2021.
Disclosures:
Gloria Erazo indicated no relevant financial relationships.
Ooreoluwa Fasola indicated no relevant financial relationships.
Jorge Rodriguez indicated no relevant financial relationships.
Ahmed Bashir Sukhera indicated no relevant financial relationships.
Daniel Guifarro Rivera indicated no relevant financial relationships.
Romelia Barba Bernal indicated no relevant financial relationships.
John Garza indicated no relevant financial relationships.
Kalyan Chakrala indicated no relevant financial relationships.
Gloria Erazo, MD1, Ooreoluwa Fasola, MD2, Jorge Rodriguez, MD3, Ahmed Bashir Sukhera, MD2, Daniel Guifarro Rivera, MD4, Romelia A. Barba Bernal, MD5, John Garza, PhD3, Kalyan Chakrala, DO2. P2662 - Current Dismorphisms of Rural and Urban Colon Cancer Screenings, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Tech University, Odessa, TX; 2Texas Tech University Health Sciences Center, Odessa, TX; 3Texas Tech University Health Sciences Center - Permian Basin, Odessa, TX; 4Cook County Health and Hospital Systems, Chicago, IL; 5Texas Tech University Health Sciences Center, Lubbock, TX
Introduction: Colorectal cancer (CRC) is the fourth most common cancer by incidence in the US. Although overall rates have declined there are notable disparities, with rural populations experiencing higher cancer incidence and mortality rates compared to urban areas. We aimed to examine how social factors in different areas affect CRC screening.
Methods: The study analyzed colon cancer screening rates in Texas for residents aged 45–74 in 2021 using statewide data. Screenings were identified via CPT and HCPCS codes. Population estimates by age group and county were obtained from SEER, and counties were classified as urban (≥50,000) or rural (< 50,000) based on the 2013 NCHS Urban-Rural Classification. Age-adjusted screening rates (AASRs) per 100,000 were calculated using the 2000 U.S. standard population. Confidence intervals were estimated using the standard error formula (AASR divided by the square root of the number of screenings), and differences between rural and urban areas were assessed by comparing 95% confidence intervals. Subgroup analyses were conducted by age, sex, and race/ethnicity.
Results: We included 7,080,602 residents, 841,312 (11.9%) lived in rural areas. A total of 494,437 CRC screenings were identified with 42,612 (8.6%) for rural residents and 451,825 (91.4%) for urban. The overall statewide AASR was 6071.5 (95% CI 6054.6 to 6088.4). The urban AASR 6297.0 (95% CI 6278.6 to 6315.3) was substantially greater than the rural AASR 4182.7 (95% CI 4143.0 to 4222.4). Out of 172 rural counties, 160 (93.0%) had AASR below the statewide AASR. The association of rural residence and AASR remained consistent within each of the examined subgroups. Within rural areas, females had higher AASR than males and Whites had substantially higher AASR compared to other races. The highest rate was measured for urban whites AASR 7039.1 (95% CI 7012.0 to 7066.2) while the lowest rate was for rural Native Americans AASR 471.8 (95% CI 308.3 to 635.2).
Discussion: There is a significant disparity in CRC screening rates between urban and rural populations in Texas, with rural areas showing lower screening rates. The findings emphasize the need for targeted efforts to improve screening access and rates in rural communities. Improving survival rates for CRC may be achieved through collaboration among healthcare providers, patients, and communities to increase awareness and early detection.
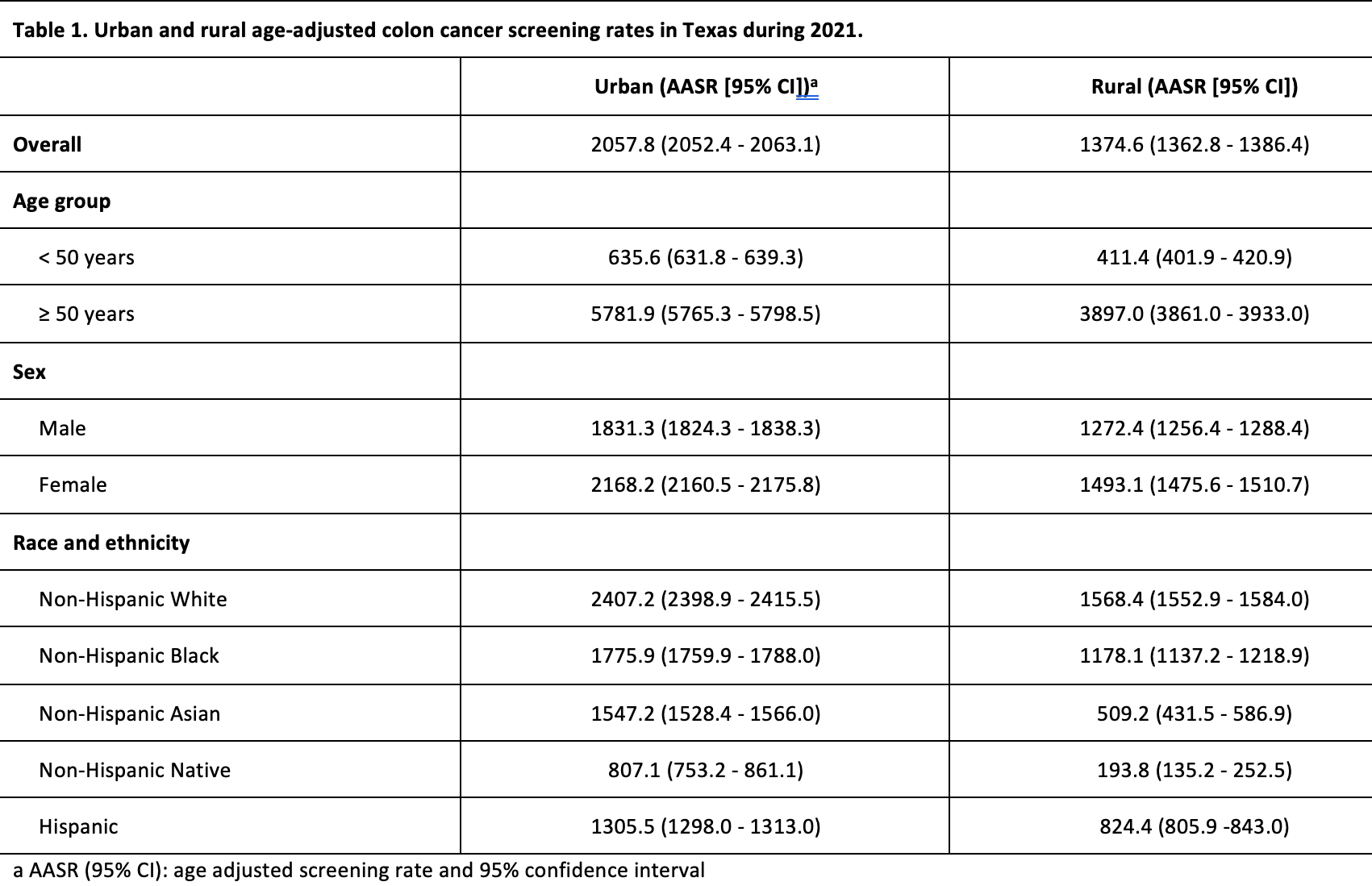
Figure: Urban and rural age-adjusted CRC screening rates in Texas during 2021.
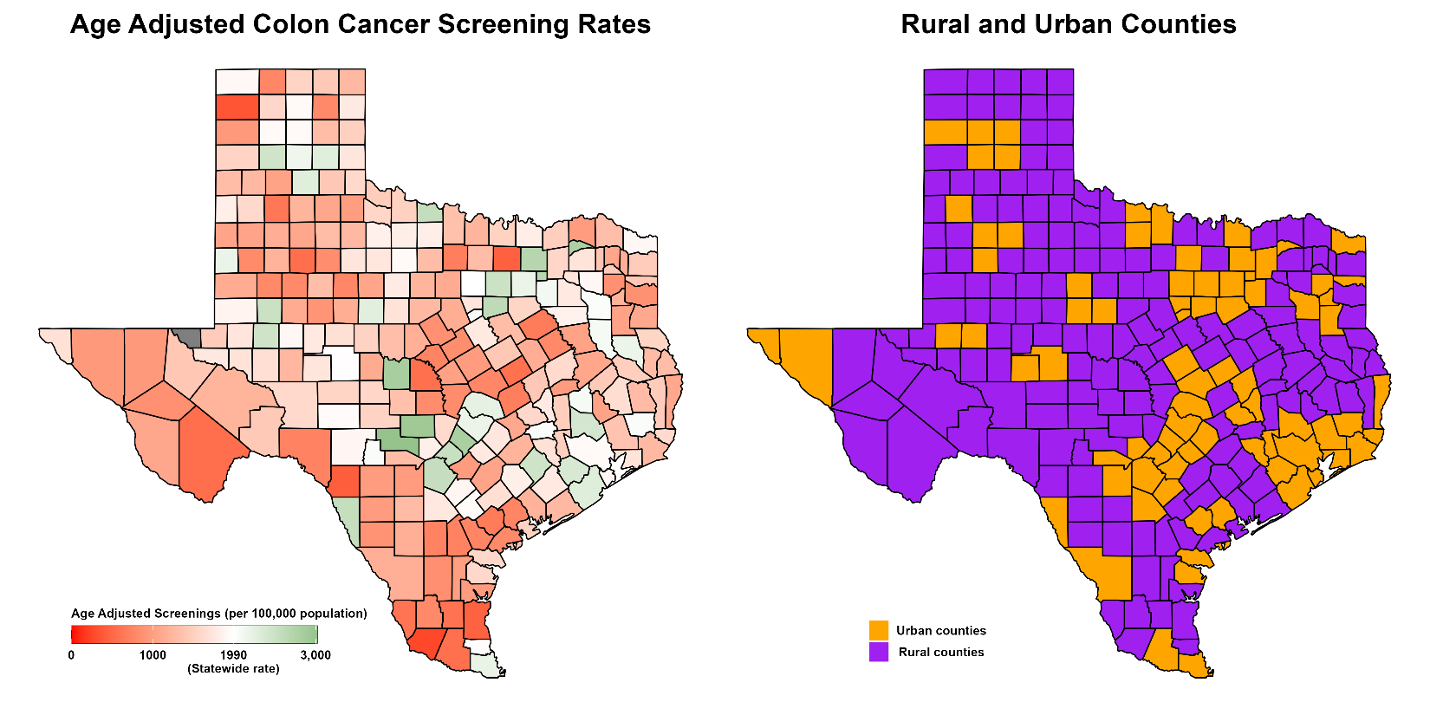
Figure: Urban and rural age-adjusted CRC screening rates in Texas during 2021.
Disclosures:
Gloria Erazo indicated no relevant financial relationships.
Ooreoluwa Fasola indicated no relevant financial relationships.
Jorge Rodriguez indicated no relevant financial relationships.
Ahmed Bashir Sukhera indicated no relevant financial relationships.
Daniel Guifarro Rivera indicated no relevant financial relationships.
Romelia Barba Bernal indicated no relevant financial relationships.
John Garza indicated no relevant financial relationships.
Kalyan Chakrala indicated no relevant financial relationships.
Gloria Erazo, MD1, Ooreoluwa Fasola, MD2, Jorge Rodriguez, MD3, Ahmed Bashir Sukhera, MD2, Daniel Guifarro Rivera, MD4, Romelia A. Barba Bernal, MD5, John Garza, PhD3, Kalyan Chakrala, DO2. P2662 - Current Dismorphisms of Rural and Urban Colon Cancer Screenings, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
