Monday Poster Session
Category: Colorectal Cancer Prevention
P2660 - Risks of Advanced Adenomas and Colorectal Cancers in Patients With Negative Versus Positive Fecal Immunochemical Tests and Implications in Clinical Practice: Real-World Experience From Urban Public Hospitals
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- CG
Changlin Gong, MD
NYC Health + Hospitals/Jacobi
Bronx, NY
Presenting Author(s)
Changlin Gong, MD1, Maria Felix Torres Nolasco, MD1, Rahul Kumar, MD2, Adejoke Johnson, MD2, Dharshana Prem Anand, MD1, Donald P. Kotler, MD1
1NYC Health + Hospitals/Jacobi, Bronx, NY; 2North Central Bronx Hospital, Bronx, NY
Introduction: The United States Preventive Services Task Force (USPSTF) lowered the age of colorectal cancer screening to 45 years old in 2021, which greatly increased the demand for colonoscopy. In US public hospitals that serve underprivileged populations, the waiting time for colonoscopy often is up to 1 year and primary care providers may send a fecal immunochemical test (FIT) while waiting.
Methods: We retrospectively examined colonoscopy results from patients in 2 urban public hospitals who previously received FIT testing, focusing on the risk of colorectal cancer and advanced adenoma, which has high risk of progression into cancer if not removed.
Results: A total of 439 FIT-negative and 137 FIT-positive patients were included. Significantly higher detection rates of advanced adenoma (21.2% vs 4.3%, P < 0.001) and colorectal cancer (5.1% vs 0.5%, P = 0.001) were found in FIT-positives. Two (0.5%) FIT-negative patients were found to have cancer but both had significant anemia (HGB 7.8 and 8.6 g/dL). No significant differences were found in the risks of nonadvanced adenomas (29.9% vs 24.8%, P = 0.235) or hyperplastic polyps (19% vs 18.7%, P = 0.938). Among patients without symptoms (rectal bleeding, refractory constipation, and weight loss) or anemia, cancer was detected in 3 patients, all tested positive for FIT, and 20.5% of FIT-positive patients as well as 3.2% of FIT-negative patients were found to have advanced adenoma (P < 0.001), equivalent to a negative predictive value of 96.8%. For FIT-negative patients, when comparing those who received colonoscopy within 1 year and those who received colonoscopy between 1-2 years, no significant difference was found in the detection rate of advanced adenoma (4.6% vs 4.1%, P = 0.823). Among FIT-negative patients, no difference was found in FIT to colonoscopy interval between those who had advanced adenoma vs those who did not (313 (210-440.5) days vs 267.5 (144-448) days, P = 0.6). No difference was found among FIT-positive patients, either (84 (55-164) days vs 80.5 (53-137.5) days, P = 0.889).
Discussion: The negative predictive value of FIT results (96.8% in asymptomatic patients) in our patient population is similar to previous reports (93.6-96.6%). FIT cannot effectively detect nonadvanced adenomas or hyperplastic polyps. Simultaneously ordering FIT and colonoscopy may not be necessary. Interval between FIT and colonoscopy (1 vs 2 years) did not affect the risk of advanced adenoma. Routine FIT frequency can be reduced to every 2 years.
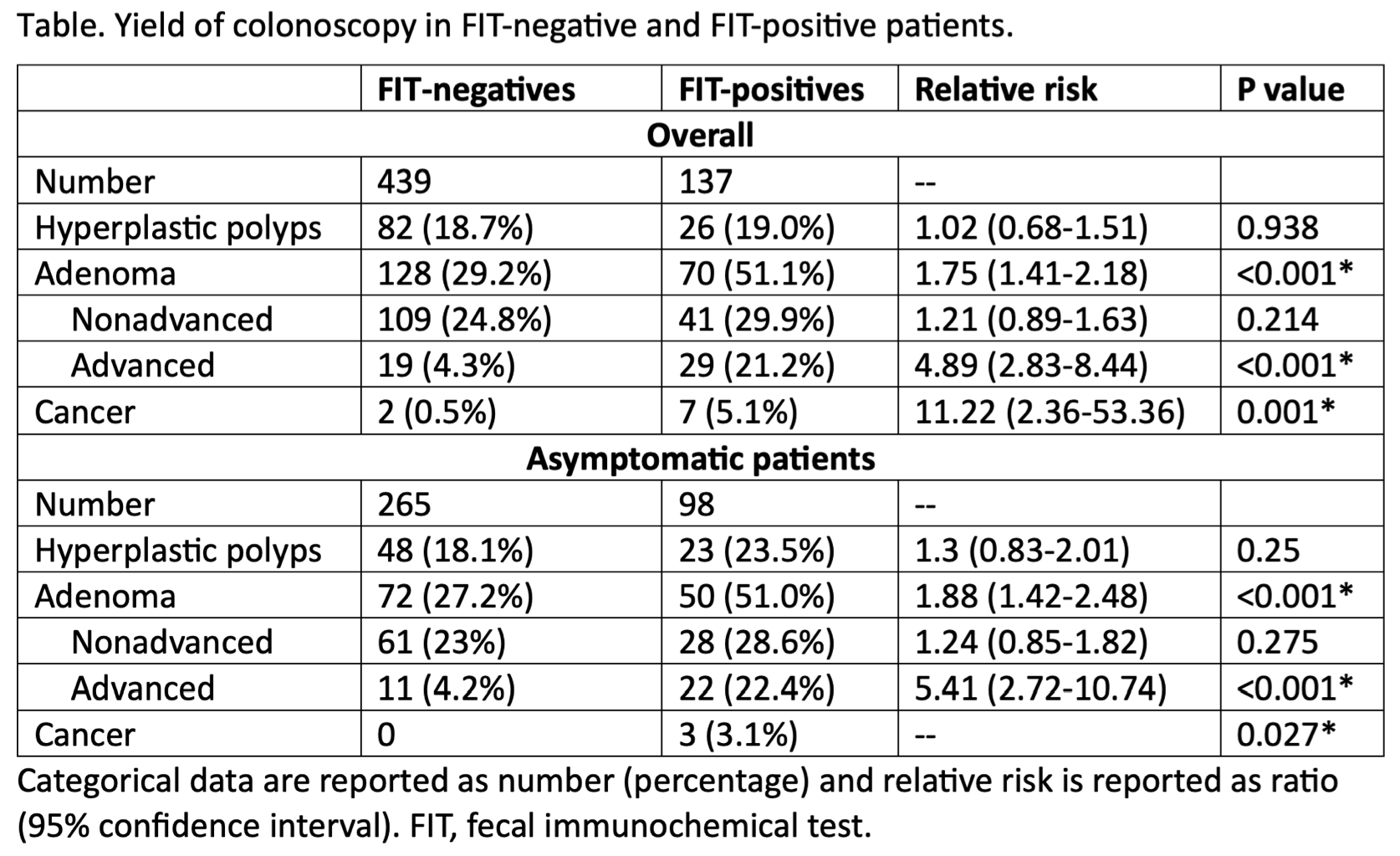
Figure: Yield of colonoscopy in FIT-negative and FIT-positive patients
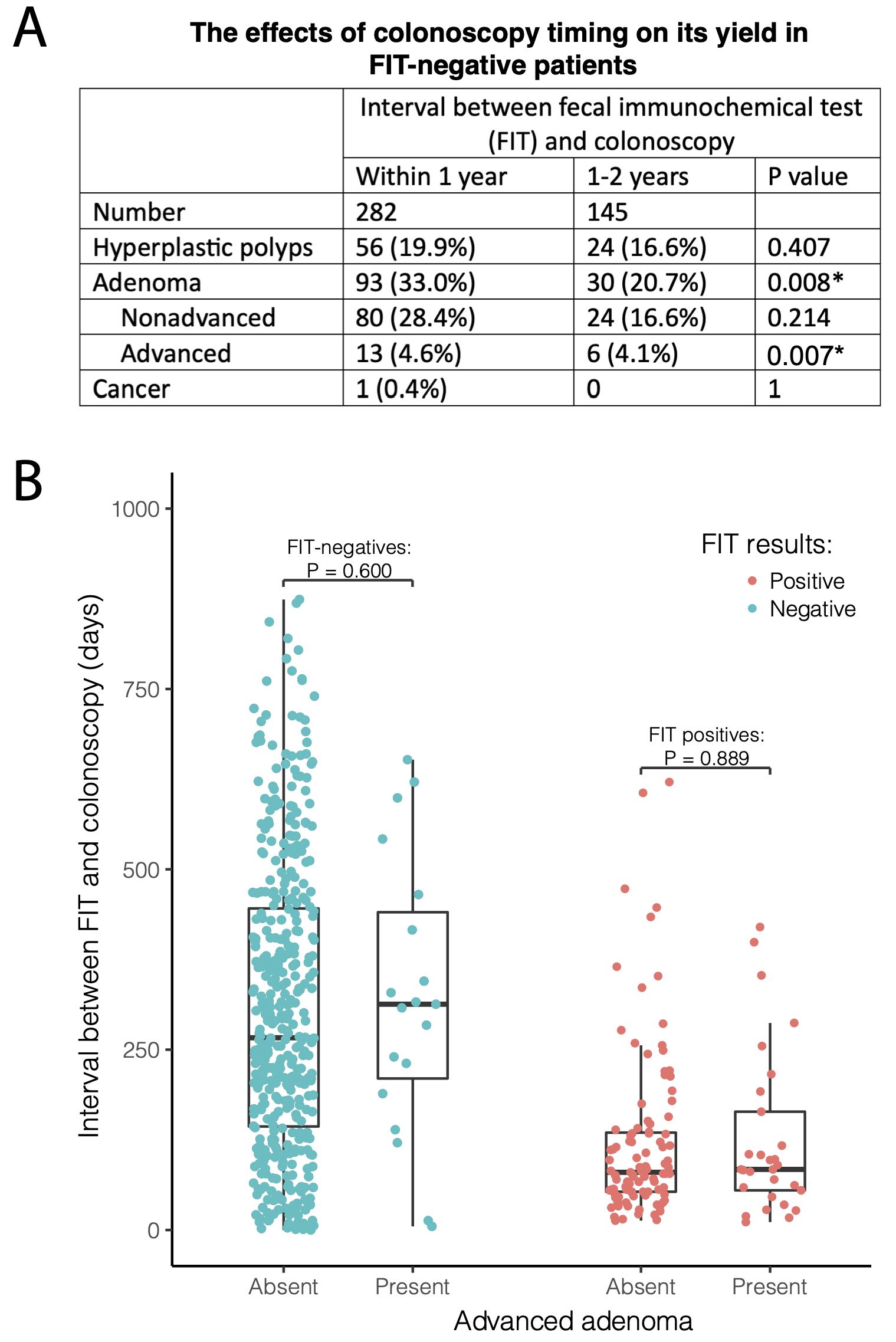
Figure: Colonoscopy timing and yield. A) Comparison of colonoscopy yield in FIT-negative patients who completed colonoscopy within 1 year vs those who completed colonoscopy between 1-2 years. B) Comparison of the interval between FIT and colonoscopy in patients who were found to have advanced adenomas vs those who were not. FIT, fecal immunochemical test.
Disclosures:
Changlin Gong indicated no relevant financial relationships.
Maria Felix Torres Nolasco indicated no relevant financial relationships.
Rahul Kumar indicated no relevant financial relationships.
Adejoke Johnson indicated no relevant financial relationships.
Dharshana Prem Anand indicated no relevant financial relationships.
Donald Kotler indicated no relevant financial relationships.
Changlin Gong, MD1, Maria Felix Torres Nolasco, MD1, Rahul Kumar, MD2, Adejoke Johnson, MD2, Dharshana Prem Anand, MD1, Donald P. Kotler, MD1. P2660 - Risks of Advanced Adenomas and Colorectal Cancers in Patients With Negative Versus Positive Fecal Immunochemical Tests and Implications in Clinical Practice: Real-World Experience From Urban Public Hospitals, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYC Health + Hospitals/Jacobi, Bronx, NY; 2North Central Bronx Hospital, Bronx, NY
Introduction: The United States Preventive Services Task Force (USPSTF) lowered the age of colorectal cancer screening to 45 years old in 2021, which greatly increased the demand for colonoscopy. In US public hospitals that serve underprivileged populations, the waiting time for colonoscopy often is up to 1 year and primary care providers may send a fecal immunochemical test (FIT) while waiting.
Methods: We retrospectively examined colonoscopy results from patients in 2 urban public hospitals who previously received FIT testing, focusing on the risk of colorectal cancer and advanced adenoma, which has high risk of progression into cancer if not removed.
Results: A total of 439 FIT-negative and 137 FIT-positive patients were included. Significantly higher detection rates of advanced adenoma (21.2% vs 4.3%, P < 0.001) and colorectal cancer (5.1% vs 0.5%, P = 0.001) were found in FIT-positives. Two (0.5%) FIT-negative patients were found to have cancer but both had significant anemia (HGB 7.8 and 8.6 g/dL). No significant differences were found in the risks of nonadvanced adenomas (29.9% vs 24.8%, P = 0.235) or hyperplastic polyps (19% vs 18.7%, P = 0.938). Among patients without symptoms (rectal bleeding, refractory constipation, and weight loss) or anemia, cancer was detected in 3 patients, all tested positive for FIT, and 20.5% of FIT-positive patients as well as 3.2% of FIT-negative patients were found to have advanced adenoma (P < 0.001), equivalent to a negative predictive value of 96.8%. For FIT-negative patients, when comparing those who received colonoscopy within 1 year and those who received colonoscopy between 1-2 years, no significant difference was found in the detection rate of advanced adenoma (4.6% vs 4.1%, P = 0.823). Among FIT-negative patients, no difference was found in FIT to colonoscopy interval between those who had advanced adenoma vs those who did not (313 (210-440.5) days vs 267.5 (144-448) days, P = 0.6). No difference was found among FIT-positive patients, either (84 (55-164) days vs 80.5 (53-137.5) days, P = 0.889).
Discussion: The negative predictive value of FIT results (96.8% in asymptomatic patients) in our patient population is similar to previous reports (93.6-96.6%). FIT cannot effectively detect nonadvanced adenomas or hyperplastic polyps. Simultaneously ordering FIT and colonoscopy may not be necessary. Interval between FIT and colonoscopy (1 vs 2 years) did not affect the risk of advanced adenoma. Routine FIT frequency can be reduced to every 2 years.
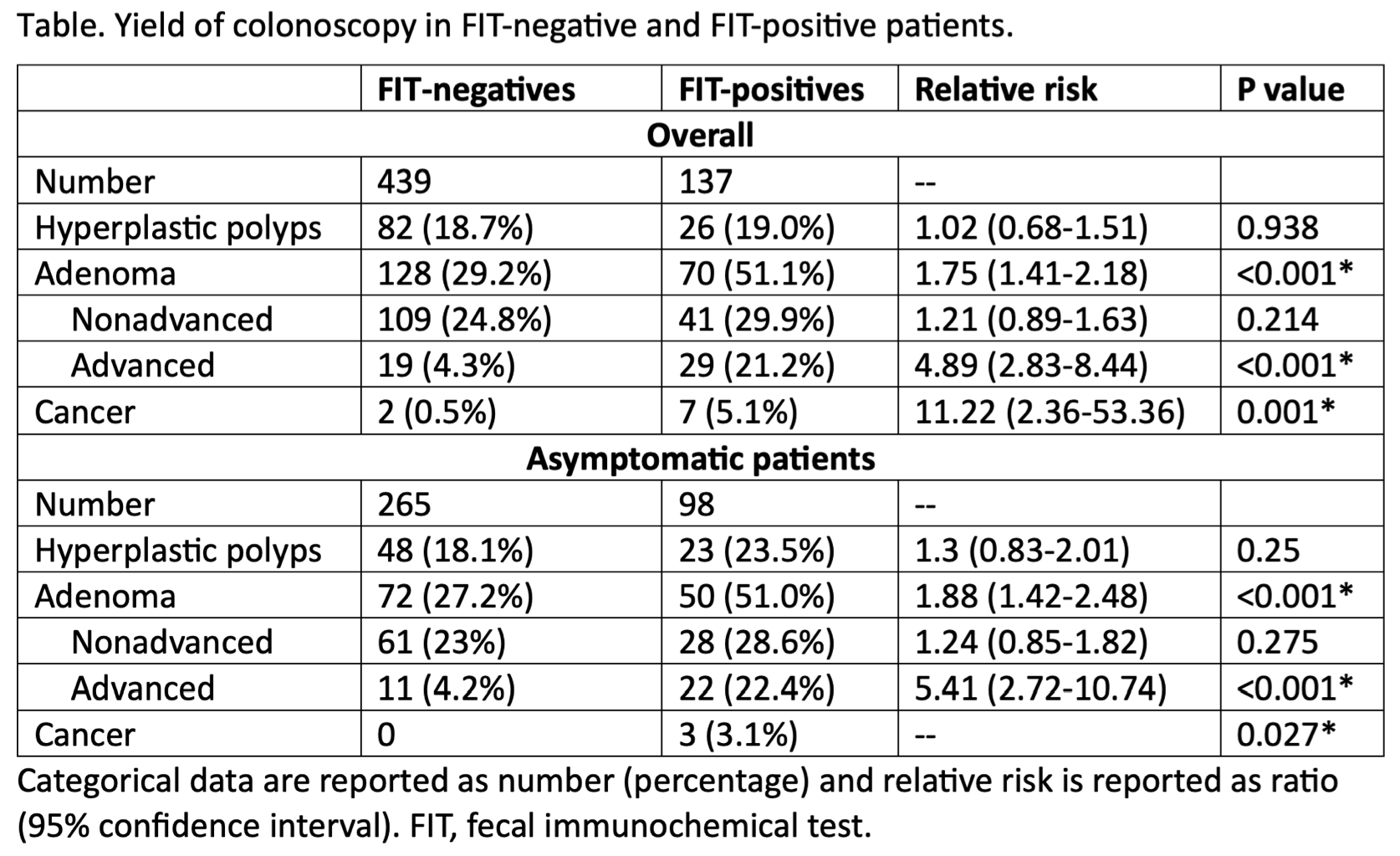
Figure: Yield of colonoscopy in FIT-negative and FIT-positive patients
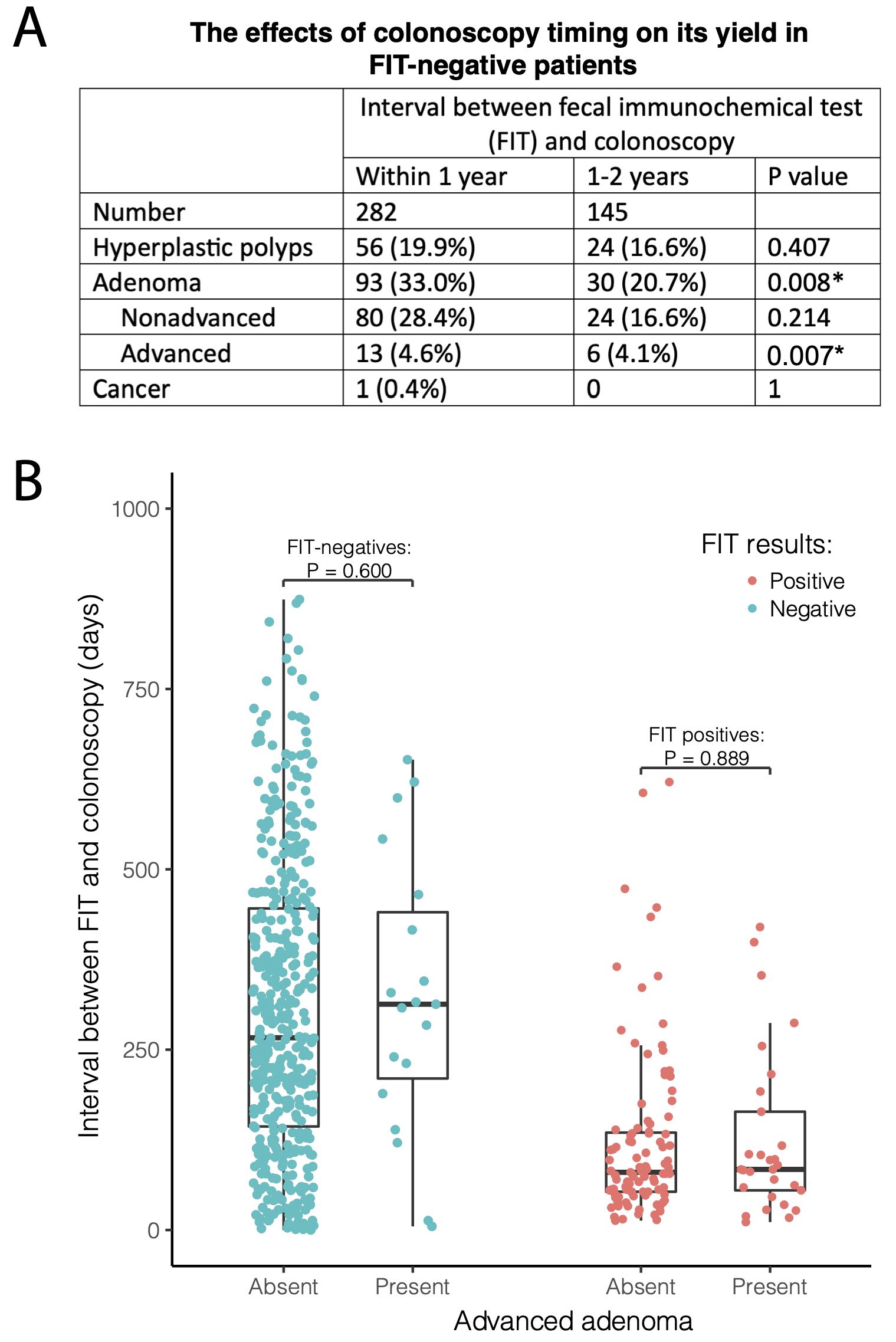
Figure: Colonoscopy timing and yield. A) Comparison of colonoscopy yield in FIT-negative patients who completed colonoscopy within 1 year vs those who completed colonoscopy between 1-2 years. B) Comparison of the interval between FIT and colonoscopy in patients who were found to have advanced adenomas vs those who were not. FIT, fecal immunochemical test.
Disclosures:
Changlin Gong indicated no relevant financial relationships.
Maria Felix Torres Nolasco indicated no relevant financial relationships.
Rahul Kumar indicated no relevant financial relationships.
Adejoke Johnson indicated no relevant financial relationships.
Dharshana Prem Anand indicated no relevant financial relationships.
Donald Kotler indicated no relevant financial relationships.
Changlin Gong, MD1, Maria Felix Torres Nolasco, MD1, Rahul Kumar, MD2, Adejoke Johnson, MD2, Dharshana Prem Anand, MD1, Donald P. Kotler, MD1. P2660 - Risks of Advanced Adenomas and Colorectal Cancers in Patients With Negative Versus Positive Fecal Immunochemical Tests and Implications in Clinical Practice: Real-World Experience From Urban Public Hospitals, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
