Monday Poster Session
Category: Colorectal Cancer Prevention
P2659 - Demographic and Regional Trends of Cardiovascular Disease and Colorectal Cancer-Related Mortality in the United States, 1999–2020
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anmol Mohan, MD
Carle Foundation hospital
Urbana, Pakistan
Presenting Author(s)
Anmol Mohan, MD1, Dev Tanush, MBBS2, Abdullah Sultany, MD3
1Carle Foundation hospital, Urbana, IL; 2Ziauddin University, Ziauddin Medical College, Karachi, Sindh, Pakistan; 3Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA
Introduction: Colorectal cancer (CRC) is increasingly recognized as both a major public health concern and a potential risk factor for cardiovascular disease (CVD), highlighting a critical overlap between two leading causes of morbidity and mortality. This study examines demographic and regional trends in CRC- and CVD-related mortality in the United States from 1999 to 2020, offering insights into emerging patterns and disparities.
Methods: Mortality data were sourced from the Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) Multiple Cause of Death database for adults aged ≥25 years, and age-adjusted mortality rates (AAMRs) and crude mortality rates (CMRs) per 100,000 persons were calculated. To identify trends over time, we used Joinpoint regression to estimate the Average Annual Percent Change (AAPC) as a summary measure and calculated the Annual Percent Change (APC) to detect and quantify inflection points in mortality trends. Analyses were stratified by age, sex, race, region, and urbanization.
Results: From 1999 to 2020, 414,234 deaths related to CRC and CVD were recorded (199 ,839 women, 214 ,395 men). Mortality counts declined from 21 ,257 in 1999 (10 ,835 women, 10 ,422 men) to 19 ,363 in 2020 (8 ,629 women, 10 ,734 men). The AAMR decreased from 12.06 in 1999 to 7.18 in 2020, with an AAPC of -2.73 (95% CI: -2.95 to -2.56). Declines were most pronounced between 1999 and 2016 (APC: -3.54 [95% CI: -3.79 to -3.34]), but rates plateaued and slightly increased from 2016 to 2020 (APC: 0.77 [95% CI: -0.87 to 4.23]). Males had higher AAMRs than Females (10.95 vs 7.07). Among racial groups, the non-Hispanic (NH) Black population had the highest AAMR (12.06), followed by NH Whites (8.53), NH American Indians (7.57), Hispanics (6.84), and NH Asians (6.10). Age-specific analyses showed the highest CMRs in older adults (37.55), followed by middle-aged (3.58) and young adults (0.27). Regionally, the Northeast led with an AAMR of 10.37, the South was lowest at 7.79, and nonmetropolitan areas exceeded metropolitan ones (9.73 vs 8.47). States in the 90th percentile for AAMR were New York, Nebraska, Mississippi, West Virginia, and California.
Discussion: While mortality rates linked to CRC and CVD decreased throughout the study period, a slight uptick in recent years suggests changing disease trends. This highlights the importance of continued research to uncover root causes and guide public health efforts tailored to different populations and regions.
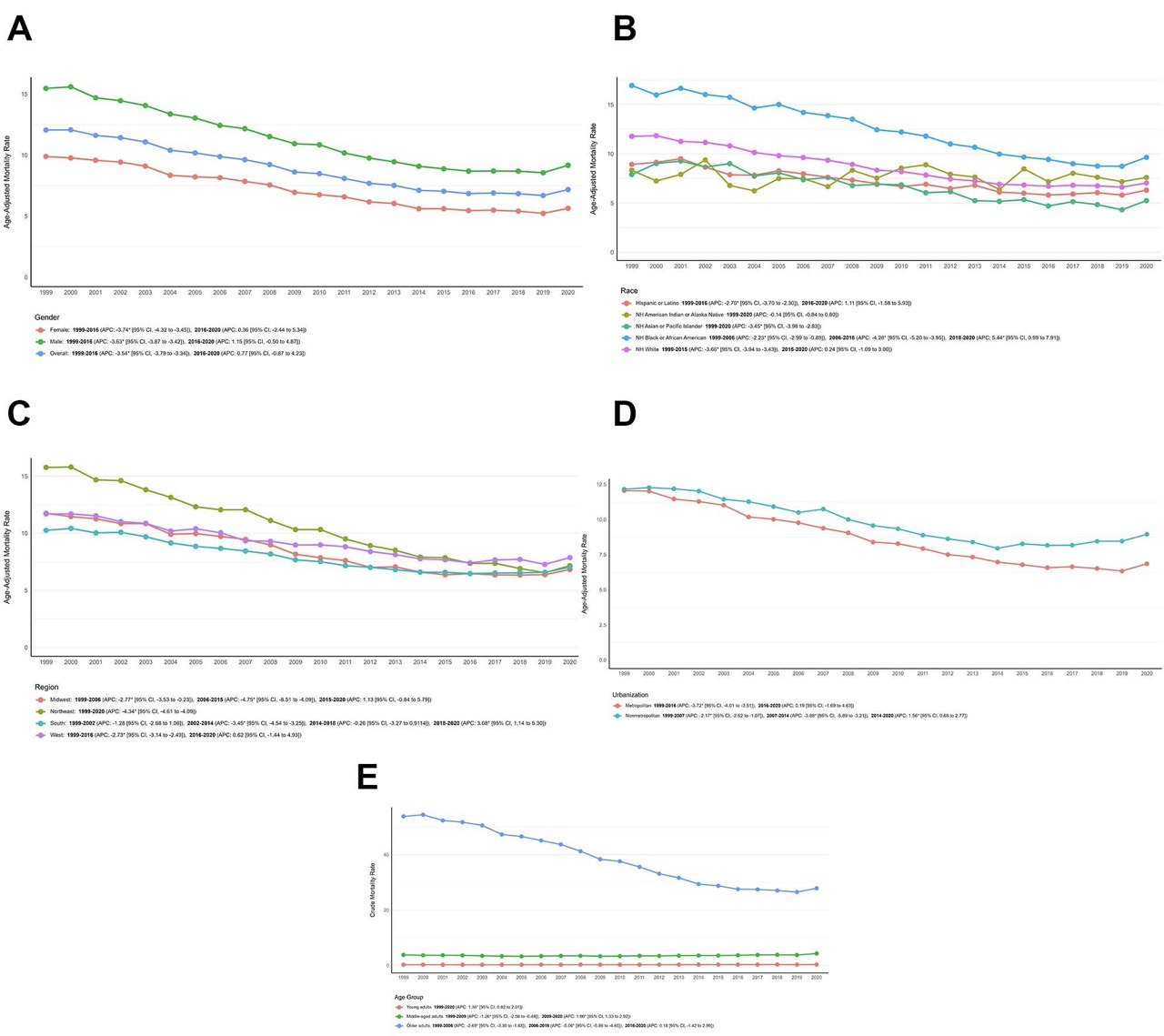
Figure: Figure 1. CVD and CRC-related AAMRs per 100,000 stratified by (A) Overall and Sex (B) Race
(C) Census Region (D) Urbanization and (E) Age Group in the United States, 1999 to 2020.
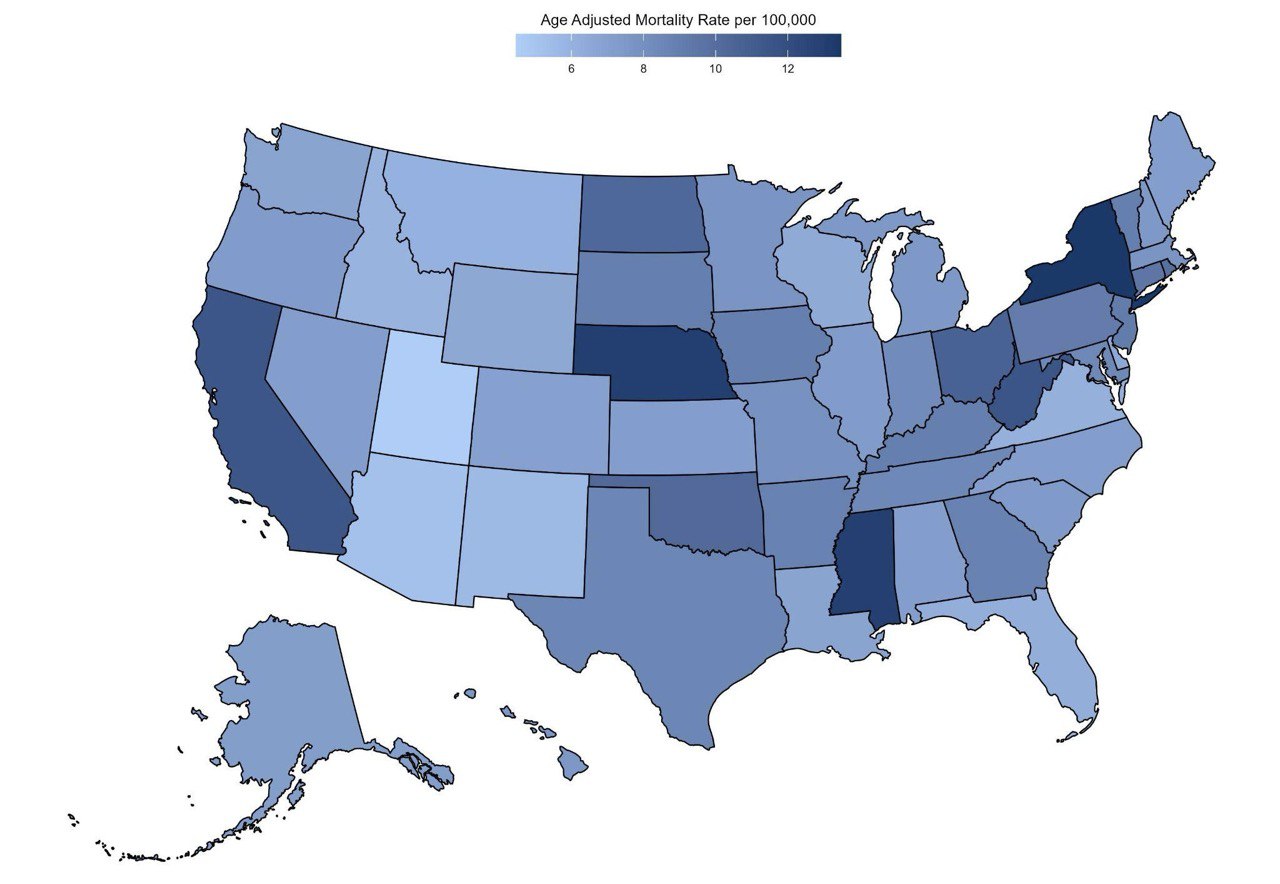
Figure: Figure 2. CVD and CRC-related AAMRs per 100,000 stratified by State in the United States, 1999 to 2020.
Disclosures:
Anmol Mohan indicated no relevant financial relationships.
Dev Tanush indicated no relevant financial relationships.
Abdullah Sultany indicated no relevant financial relationships.
Anmol Mohan, MD1, Dev Tanush, MBBS2, Abdullah Sultany, MD3. P2659 - Demographic and Regional Trends of Cardiovascular Disease and Colorectal Cancer-Related Mortality in the United States, 1999–2020, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Carle Foundation hospital, Urbana, IL; 2Ziauddin University, Ziauddin Medical College, Karachi, Sindh, Pakistan; 3Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA
Introduction: Colorectal cancer (CRC) is increasingly recognized as both a major public health concern and a potential risk factor for cardiovascular disease (CVD), highlighting a critical overlap between two leading causes of morbidity and mortality. This study examines demographic and regional trends in CRC- and CVD-related mortality in the United States from 1999 to 2020, offering insights into emerging patterns and disparities.
Methods: Mortality data were sourced from the Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) Multiple Cause of Death database for adults aged ≥25 years, and age-adjusted mortality rates (AAMRs) and crude mortality rates (CMRs) per 100,000 persons were calculated. To identify trends over time, we used Joinpoint regression to estimate the Average Annual Percent Change (AAPC) as a summary measure and calculated the Annual Percent Change (APC) to detect and quantify inflection points in mortality trends. Analyses were stratified by age, sex, race, region, and urbanization.
Results: From 1999 to 2020, 414,234 deaths related to CRC and CVD were recorded (199 ,839 women, 214 ,395 men). Mortality counts declined from 21 ,257 in 1999 (10 ,835 women, 10 ,422 men) to 19 ,363 in 2020 (8 ,629 women, 10 ,734 men). The AAMR decreased from 12.06 in 1999 to 7.18 in 2020, with an AAPC of -2.73 (95% CI: -2.95 to -2.56). Declines were most pronounced between 1999 and 2016 (APC: -3.54 [95% CI: -3.79 to -3.34]), but rates plateaued and slightly increased from 2016 to 2020 (APC: 0.77 [95% CI: -0.87 to 4.23]). Males had higher AAMRs than Females (10.95 vs 7.07). Among racial groups, the non-Hispanic (NH) Black population had the highest AAMR (12.06), followed by NH Whites (8.53), NH American Indians (7.57), Hispanics (6.84), and NH Asians (6.10). Age-specific analyses showed the highest CMRs in older adults (37.55), followed by middle-aged (3.58) and young adults (0.27). Regionally, the Northeast led with an AAMR of 10.37, the South was lowest at 7.79, and nonmetropolitan areas exceeded metropolitan ones (9.73 vs 8.47). States in the 90th percentile for AAMR were New York, Nebraska, Mississippi, West Virginia, and California.
Discussion: While mortality rates linked to CRC and CVD decreased throughout the study period, a slight uptick in recent years suggests changing disease trends. This highlights the importance of continued research to uncover root causes and guide public health efforts tailored to different populations and regions.
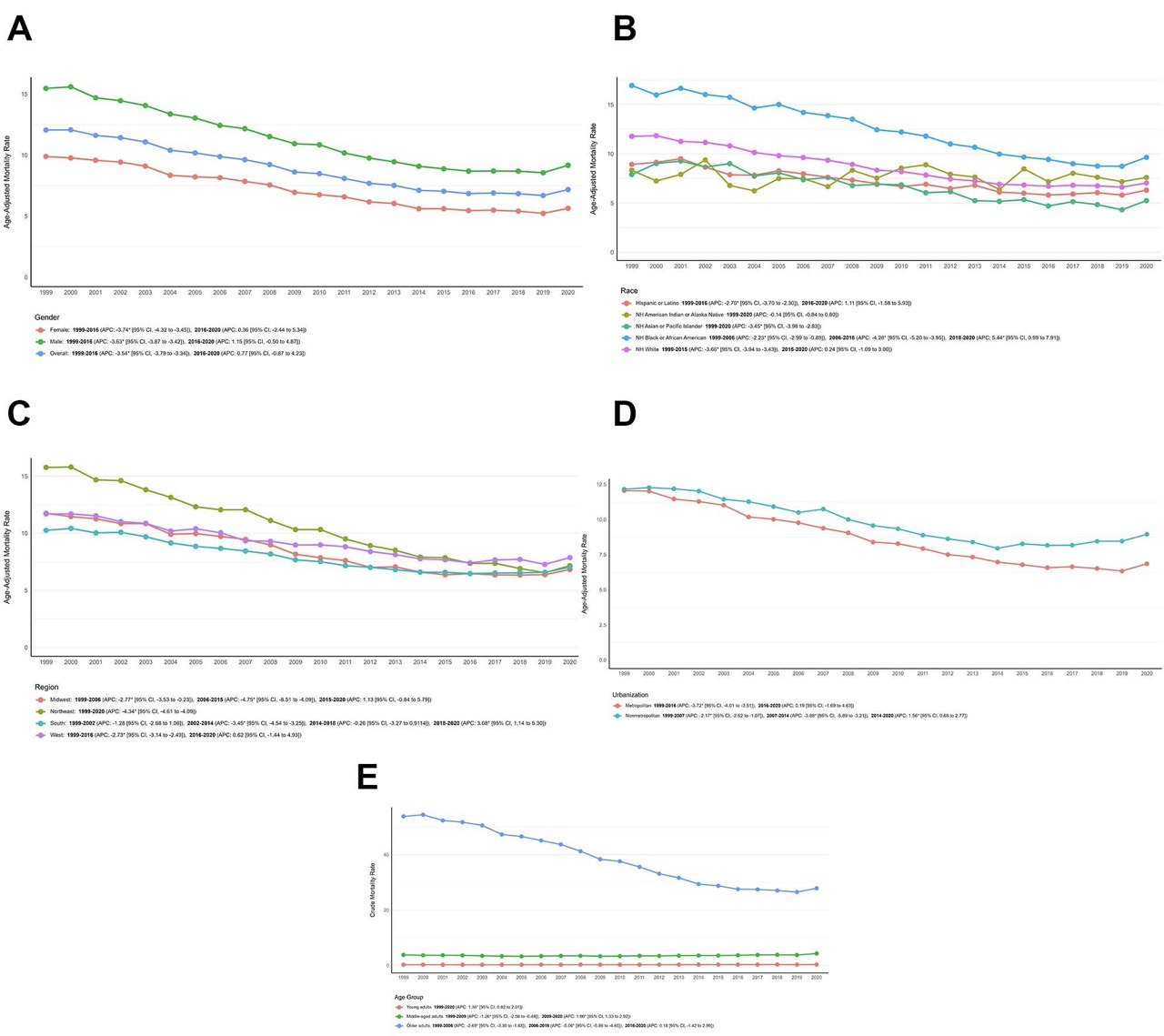
Figure: Figure 1. CVD and CRC-related AAMRs per 100,000 stratified by (A) Overall and Sex (B) Race
(C) Census Region (D) Urbanization and (E) Age Group in the United States, 1999 to 2020.
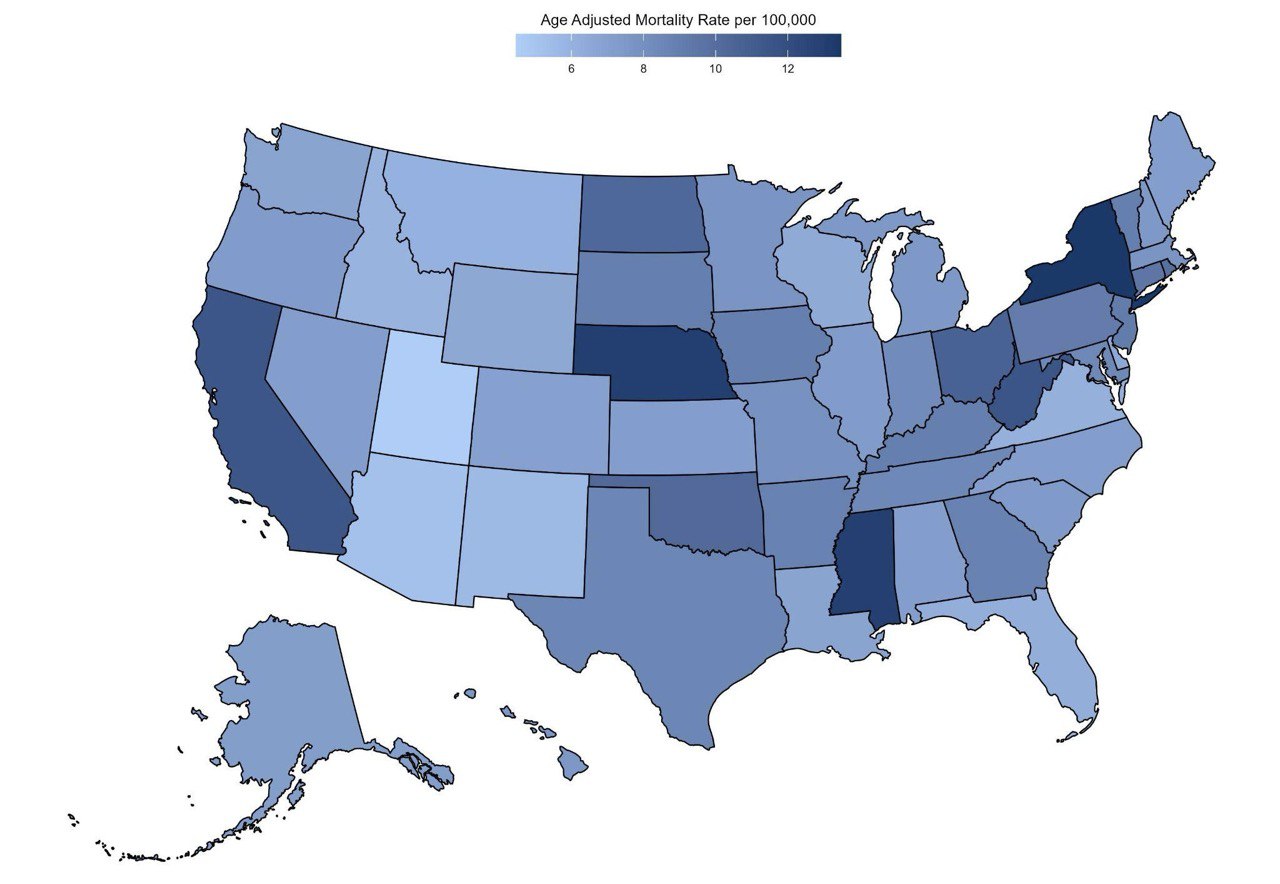
Figure: Figure 2. CVD and CRC-related AAMRs per 100,000 stratified by State in the United States, 1999 to 2020.
Disclosures:
Anmol Mohan indicated no relevant financial relationships.
Dev Tanush indicated no relevant financial relationships.
Abdullah Sultany indicated no relevant financial relationships.
Anmol Mohan, MD1, Dev Tanush, MBBS2, Abdullah Sultany, MD3. P2659 - Demographic and Regional Trends of Cardiovascular Disease and Colorectal Cancer-Related Mortality in the United States, 1999–2020, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
