Monday Poster Session
Category: Esophagus
P2840 - Herpes Esophagitis Due to Cirrhosis-Associated Immune Dysfunction
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ali Emre Bardak, MD
St. Elizabeth's Medical Center, Boston University School of Medicine
Boston, MA
Presenting Author(s)
Ali Emre Bardak, MD1, Kanan Nuriyev, MD2, Bilger Cavus, MD2, Asli Cifcibasi Ormeci, MD2, Sabahattin Kaymakoglu, MD2
1St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA; 2Istanbul University, Istanbul, Istanbul, Turkey
Introduction: Cirrhosis-associated immune dysfunction (CAID) is a broad term covering alterations in the immune system linked to end-stage liver disease. Major components of CAID include immunodeficiency and systemic inflammation, and the severity of the condition correlates with the stage of liver cirrhosis. Although often underrecognized, this condition contributes substantially to morbidity and mortality in patients with cirrhosis, primarily by predisposing them to opportunistic infections.
Case Description/
Methods: A 57-year-old male patient with alcohol-related liver cirrhosis, which is decompensated with ascites and a history of esophageal variceal hemorrhage, presented to our clinic with complaints of difficulty in swallowing and retrosternal chest pain. Upper gastrointestinal endoscopy revealed shallow ulcers across the esophagus with normal-looking mucosa in between, suggesting viral esophagitis (Figure 1). The subsequent pathology report confirmed the diagnosis of herpes simplex virus esophagitis. No immunosuppressive condition other than cirrhosis was found when the patient's comorbidities and medications were assessed. The ulcers markedly receded following intravenous acyclovir 5 mg/kg every 8 hours for 14 days (Figure 2).
Discussion: Opportunistic infections can develop in a patient with cirrhosis without any other immunosuppressive condition. This is because cirrhosis itself is associated with immune dysfunction. In our case, the patient had no other diseases or medications affecting immune function; therefore, herpes esophagitis, typically seen in immunocompromised individuals, was considered to have developed in the setting of CAID. Several approaches are currently under investigation to modulate CAID, including targeting bacterial translocation, humoral factors, the bone marrow, and directly targeting immune cells.
The differential diagnosis for esophageal ulcers includes reflux esophagitis, peptic ulcer disease, Crohn's disease, Behçet's disease, and drug-induced esophagitis. In our case, the diagnosis of herpes esophagitis is made based on the clinical presentation, endoscopic findings, and histopathological examination. Herpes esophagitis is a serious condition that can cause significant morbidity and mortality. When diagnosed and treated early, patients usually have a good prognosis. However, complications such as esophageal strictures or perforations may develop in some cases.
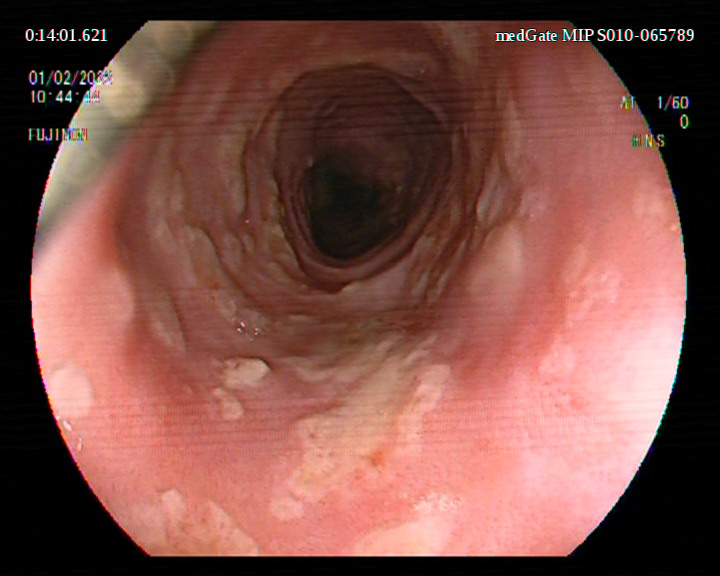
Figure: Figure 1: Multiple shallow esophageal ulcers separated by normal-appearing mucosa, a pattern suggestive of a viral etiology, most consistent with herpes esophagitis.
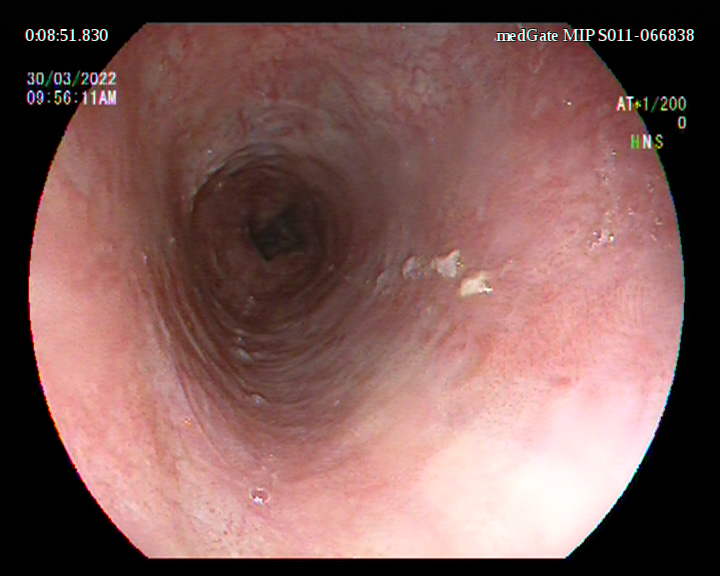
Figure: Figure 2: Following intravenous acyclovir therapy, the ulcers significantly receded.
Disclosures:
Ali Emre Bardak indicated no relevant financial relationships.
Kanan Nuriyev indicated no relevant financial relationships.
Bilger Cavus indicated no relevant financial relationships.
Asli Cifcibasi Ormeci indicated no relevant financial relationships.
Sabahattin Kaymakoglu indicated no relevant financial relationships.
Ali Emre Bardak, MD1, Kanan Nuriyev, MD2, Bilger Cavus, MD2, Asli Cifcibasi Ormeci, MD2, Sabahattin Kaymakoglu, MD2. P2840 - Herpes Esophagitis Due to Cirrhosis-Associated Immune Dysfunction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA; 2Istanbul University, Istanbul, Istanbul, Turkey
Introduction: Cirrhosis-associated immune dysfunction (CAID) is a broad term covering alterations in the immune system linked to end-stage liver disease. Major components of CAID include immunodeficiency and systemic inflammation, and the severity of the condition correlates with the stage of liver cirrhosis. Although often underrecognized, this condition contributes substantially to morbidity and mortality in patients with cirrhosis, primarily by predisposing them to opportunistic infections.
Case Description/
Methods: A 57-year-old male patient with alcohol-related liver cirrhosis, which is decompensated with ascites and a history of esophageal variceal hemorrhage, presented to our clinic with complaints of difficulty in swallowing and retrosternal chest pain. Upper gastrointestinal endoscopy revealed shallow ulcers across the esophagus with normal-looking mucosa in between, suggesting viral esophagitis (Figure 1). The subsequent pathology report confirmed the diagnosis of herpes simplex virus esophagitis. No immunosuppressive condition other than cirrhosis was found when the patient's comorbidities and medications were assessed. The ulcers markedly receded following intravenous acyclovir 5 mg/kg every 8 hours for 14 days (Figure 2).
Discussion: Opportunistic infections can develop in a patient with cirrhosis without any other immunosuppressive condition. This is because cirrhosis itself is associated with immune dysfunction. In our case, the patient had no other diseases or medications affecting immune function; therefore, herpes esophagitis, typically seen in immunocompromised individuals, was considered to have developed in the setting of CAID. Several approaches are currently under investigation to modulate CAID, including targeting bacterial translocation, humoral factors, the bone marrow, and directly targeting immune cells.
The differential diagnosis for esophageal ulcers includes reflux esophagitis, peptic ulcer disease, Crohn's disease, Behçet's disease, and drug-induced esophagitis. In our case, the diagnosis of herpes esophagitis is made based on the clinical presentation, endoscopic findings, and histopathological examination. Herpes esophagitis is a serious condition that can cause significant morbidity and mortality. When diagnosed and treated early, patients usually have a good prognosis. However, complications such as esophageal strictures or perforations may develop in some cases.
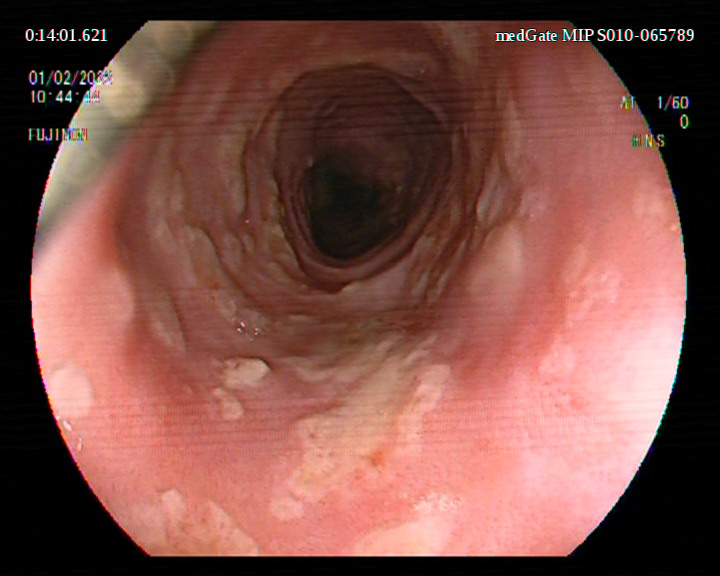
Figure: Figure 1: Multiple shallow esophageal ulcers separated by normal-appearing mucosa, a pattern suggestive of a viral etiology, most consistent with herpes esophagitis.
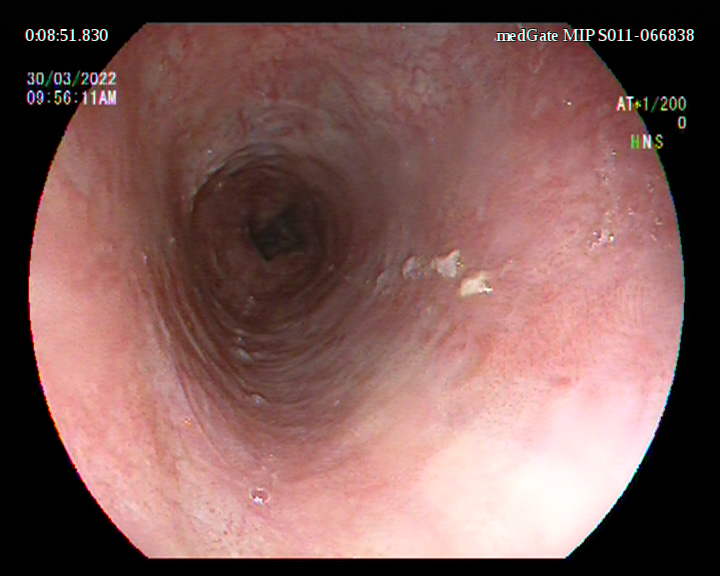
Figure: Figure 2: Following intravenous acyclovir therapy, the ulcers significantly receded.
Disclosures:
Ali Emre Bardak indicated no relevant financial relationships.
Kanan Nuriyev indicated no relevant financial relationships.
Bilger Cavus indicated no relevant financial relationships.
Asli Cifcibasi Ormeci indicated no relevant financial relationships.
Sabahattin Kaymakoglu indicated no relevant financial relationships.
Ali Emre Bardak, MD1, Kanan Nuriyev, MD2, Bilger Cavus, MD2, Asli Cifcibasi Ormeci, MD2, Sabahattin Kaymakoglu, MD2. P2840 - Herpes Esophagitis Due to Cirrhosis-Associated Immune Dysfunction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
