Monday Poster Session
Category: Esophagus
P2836 - Atypical Presentation of Downhill Esophageal Varices: A Diagnostic Enigma
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Karim Al Annan, MD (he/him/his)
University of Connecticut Health Center
Hartford, CT
Presenting Author(s)
Karim Al Annan, MD1, Hira Khan, MD2, Marianna Scranton, DO3
1University of Connecticut Health Center, Hartford, CT; 2University of Connecticut Health Center, Farmington, CT; 3Hartford HealthCare, Hartford, CT
Introduction: Unlike the more common varices linked to portal hypertension, “downhill” esophageal varices (DEV) are rare, seen in about 0.5% of upper endoscopies. They result from impaired superior vena cava (SVC) drainage, due to causes ranging from catheter-related thrombosis to mediastinal tumors. We present a case of DEV with very atypical vascular etiology presenting as dysphagia.
Case Description/
Methods: A 75-year-old male with a history of gout, hypertension, hyperlipidemia, presented with a 6-month history of intermittent dysphagia to solids with globus sensation. An endoscopy revealed large ( > 5 mm) varices seen from the upper esophageal sphincter to 30 cm from the incisors in at least 2 columns, and not extending to the mid-esophagus (Fig.1). Preliminary workup including hepatic function testing, viral hepatitis panel, coagulation studies, alpha-1-antitrypsin, autoimmune panel were all unremarkable. Transient elastography showed no evidence of fibrosis (F0). Abdominal ultrasound showed normal liver contour without ascites, and hepatic vasculature was patent with normal flow dynamics. IR-guided transjugular liver biopsy was completed ultimately showing a normal hepatic venous pressure gradient of 2 mmHg along with absence of cirrhosis on liver histology. With high suspicion for DEV, a CTA and CTV of the chest, head & neck were performed and ruled out SVC syndrome. The findings were extensively reviewed by a multidisciplinary team including medicine, interventional radiology, vascular and thoracic surgery. Final interpretation revealed a patent SVC and IVC with no intrathoracic/mediastinal pathology (Fig.2), however there was evidence of right internal jugular vein (IJV) occlusion with possible azygous system compression which were thought to be the cause of the DEV although the reason for these findings remains unclear. The patient was planned for intervention by neuroradiology.
Discussion: DEV are rare and most often secondary to SVC syndrome. Although we did identify right IJV and azygous compression, the reason for these findings in our case is unclear. The patient's presentation with dysphagia, rather than bleeding, is also atypical for DEV. Our case, with an entirely negative hepatic workup and atypical vascular findings, appears to be the first documented instance of truly idiopathic DEV. This case underscores the diagnostic complexity of DEV in the absence of classic risk factors and highlights the need for greater awareness and further research into its pathogenesis and optimal management.
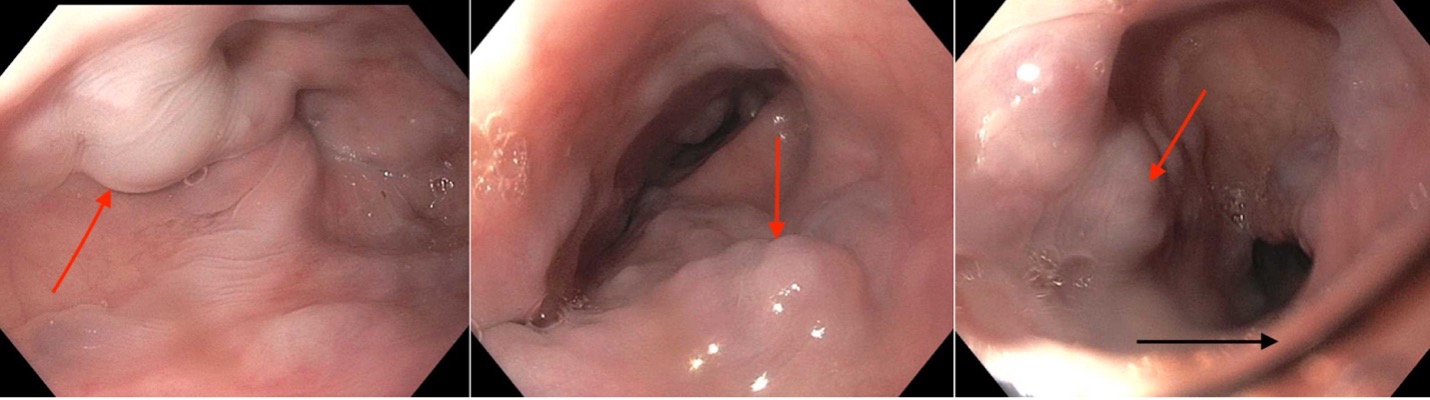
Figure: Figure 1 – Esophageal varices (red arrow) in the upper third of the esophagus at level of upper esophageal sphincter (black arrow)

Figure: Figure 2 – Patent super vena cava (arrow) on coronal section of CT venography of chest
Disclosures:
Karim Al Annan indicated no relevant financial relationships.
Hira Khan indicated no relevant financial relationships.
Marianna Scranton indicated no relevant financial relationships.
Karim Al Annan, MD1, Hira Khan, MD2, Marianna Scranton, DO3. P2836 - Atypical Presentation of Downhill Esophageal Varices: A Diagnostic Enigma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health Center, Hartford, CT; 2University of Connecticut Health Center, Farmington, CT; 3Hartford HealthCare, Hartford, CT
Introduction: Unlike the more common varices linked to portal hypertension, “downhill” esophageal varices (DEV) are rare, seen in about 0.5% of upper endoscopies. They result from impaired superior vena cava (SVC) drainage, due to causes ranging from catheter-related thrombosis to mediastinal tumors. We present a case of DEV with very atypical vascular etiology presenting as dysphagia.
Case Description/
Methods: A 75-year-old male with a history of gout, hypertension, hyperlipidemia, presented with a 6-month history of intermittent dysphagia to solids with globus sensation. An endoscopy revealed large ( > 5 mm) varices seen from the upper esophageal sphincter to 30 cm from the incisors in at least 2 columns, and not extending to the mid-esophagus (Fig.1). Preliminary workup including hepatic function testing, viral hepatitis panel, coagulation studies, alpha-1-antitrypsin, autoimmune panel were all unremarkable. Transient elastography showed no evidence of fibrosis (F0). Abdominal ultrasound showed normal liver contour without ascites, and hepatic vasculature was patent with normal flow dynamics. IR-guided transjugular liver biopsy was completed ultimately showing a normal hepatic venous pressure gradient of 2 mmHg along with absence of cirrhosis on liver histology. With high suspicion for DEV, a CTA and CTV of the chest, head & neck were performed and ruled out SVC syndrome. The findings were extensively reviewed by a multidisciplinary team including medicine, interventional radiology, vascular and thoracic surgery. Final interpretation revealed a patent SVC and IVC with no intrathoracic/mediastinal pathology (Fig.2), however there was evidence of right internal jugular vein (IJV) occlusion with possible azygous system compression which were thought to be the cause of the DEV although the reason for these findings remains unclear. The patient was planned for intervention by neuroradiology.
Discussion: DEV are rare and most often secondary to SVC syndrome. Although we did identify right IJV and azygous compression, the reason for these findings in our case is unclear. The patient's presentation with dysphagia, rather than bleeding, is also atypical for DEV. Our case, with an entirely negative hepatic workup and atypical vascular findings, appears to be the first documented instance of truly idiopathic DEV. This case underscores the diagnostic complexity of DEV in the absence of classic risk factors and highlights the need for greater awareness and further research into its pathogenesis and optimal management.
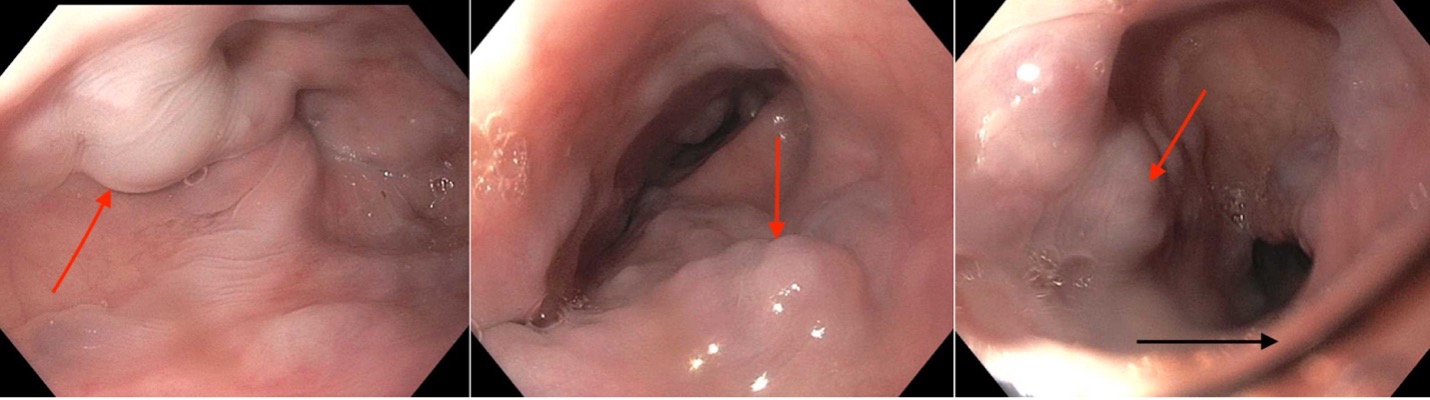
Figure: Figure 1 – Esophageal varices (red arrow) in the upper third of the esophagus at level of upper esophageal sphincter (black arrow)

Figure: Figure 2 – Patent super vena cava (arrow) on coronal section of CT venography of chest
Disclosures:
Karim Al Annan indicated no relevant financial relationships.
Hira Khan indicated no relevant financial relationships.
Marianna Scranton indicated no relevant financial relationships.
Karim Al Annan, MD1, Hira Khan, MD2, Marianna Scranton, DO3. P2836 - Atypical Presentation of Downhill Esophageal Varices: A Diagnostic Enigma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
