Monday Poster Session
Category: Esophagus
P2831 - Dilate, Paralyze, Relieve: Multimodal Management of EGJOO in an Elderly Patient
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Yuting Huang, MD, PhD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Yan Yan, MD, PhD1, Osayande Osagiede, MBBS, MPH2, Yichen Wang, MD3, Maoyin Pang, MD, PhD1, Yuting Huang, MD, PhD1
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic, Jacksonville, FL, US, Jacksonville, FL; 3Hospital of the University of Pennsylvania, Philadelphia, PA
Introduction: Esophagogastric junction outflow obstruction (EGJOO) is a primary esophageal motility disorder characterized by the impaired relaxation of the esophagogastric junction (EGJ) in conjunction with elevated intrabolus pressure while preserving some degree of normal peristalsis that does not fit with achalasia criteria. The EGJOO is detected in up to 14% of high-resolution manometry (HRM) studies, predominantly affecting females with an age range of 51 to 69 years old.
Case Description/
Methods: A 72-year-old woman with past medical history of restless leg syndrome, hypertension, hypothyroidism, and breast cancer with breast lumpectomy, presented with a 5-month history of dysphagia, odynophagia, and nocturnal nausea. Her symptom persisted despite empiric treatment with omeprazole, hyoscyamine, and diazepam. Initial evaluation with barium esophagram demonstrated mild to moderate focal narrowing in the midthoracic esophagus. Episodes of esophageal spasm were observed distal to the narrowing (Figure 1A, blue arrow). Esophageal manometry revealed an elevated integrated relaxation pressure (IRP) of 18.7 mmHg. Contractile activity was detected in the mid and lower segments of the esophagus (Figure 1B). Subsequent esophagogastroduodenoscopy (EGD) revealed a hypertonic lower esophageal sphincter (LES), diminished peristaltic activity, and normal mucosa in the entire esophagus (Figure 2). She was managed with sildenafil, endoscopic balloon dilation of the entire esophagus. Besides, the patient underwent two botulinum toxin injections targeting the lower and distal one-third of esophageal sphincter (LES). During follow-up, the patient reported modest symptom relief and improved tolerance of oral intake.
Discussion: The diagnosis of EGJOO was established based on clinical presentation, esophagram findings, and manometric evidence. Pharmacologic therapies, the first-line treatment of EGJOO, may offer symptomatic relief but do not correct the underlying esophageal motility disorder. Interventions targeting esophageal dysmotility include botulinum toxin injection, Pneumatic balloon dilation, laparoscopic Heller myotomy with Dor fundoplication, and POEM.
This case highlights the complexity and individualized nature of managing EGJOO, underscoring the need for further research to generate evidence-based recommendations for optimal treatment selection. A personalized treatment strategy and shared decision-making play a critical role in guiding the management of this condition.
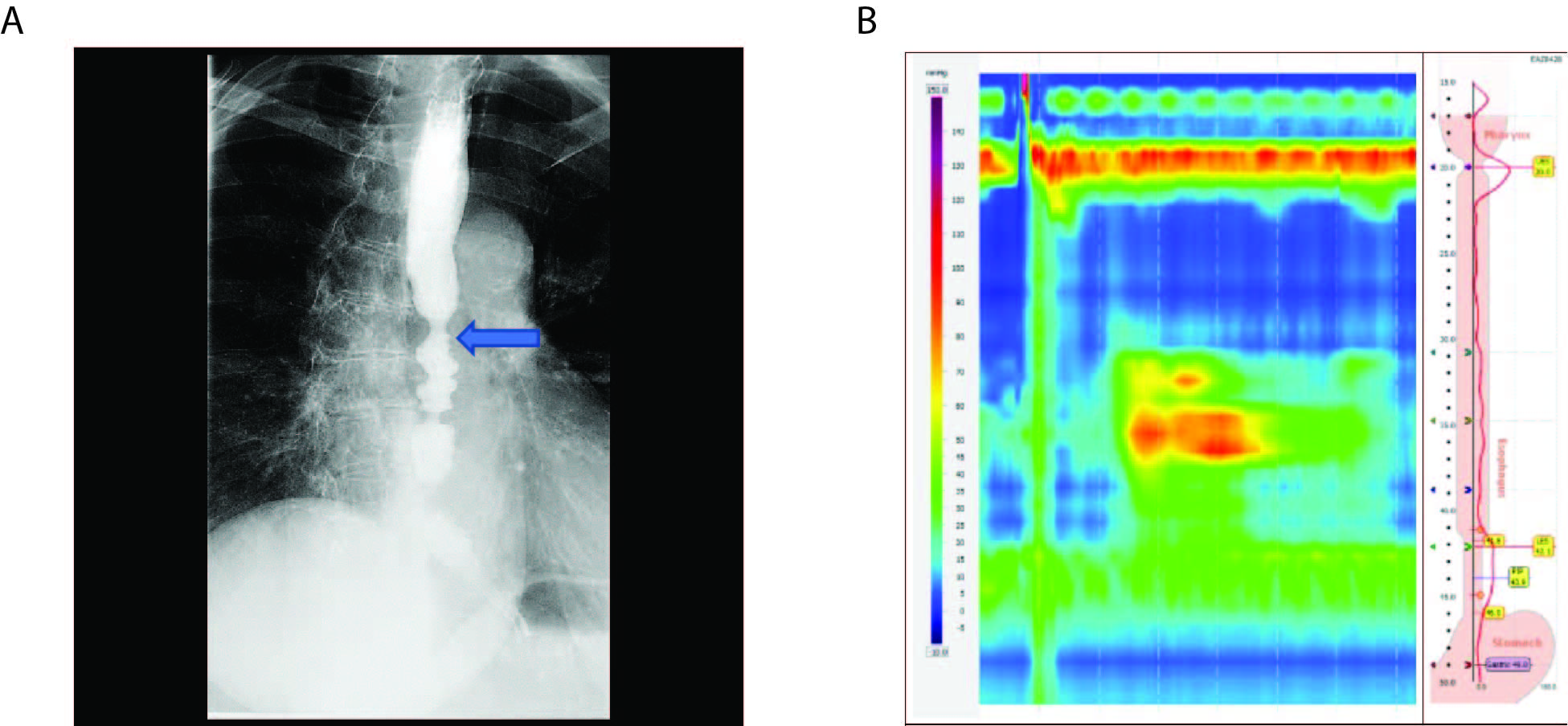
Figure: Figure 1: barium esophagram and esophageal manometry examination. (A) Barium esophagram demonstrated mild to moderate focal narrowing in the midthoracic esophagus. Episodes of esophageal spasm were observed distal to the narrowing marked with the blue arrow. (B) Esophageal manometry revealed a contractile activity in the mid and lower segments of the esophagus, characterized by an uncoordinated peristaltic sequence and pan-esophageal pressurization.
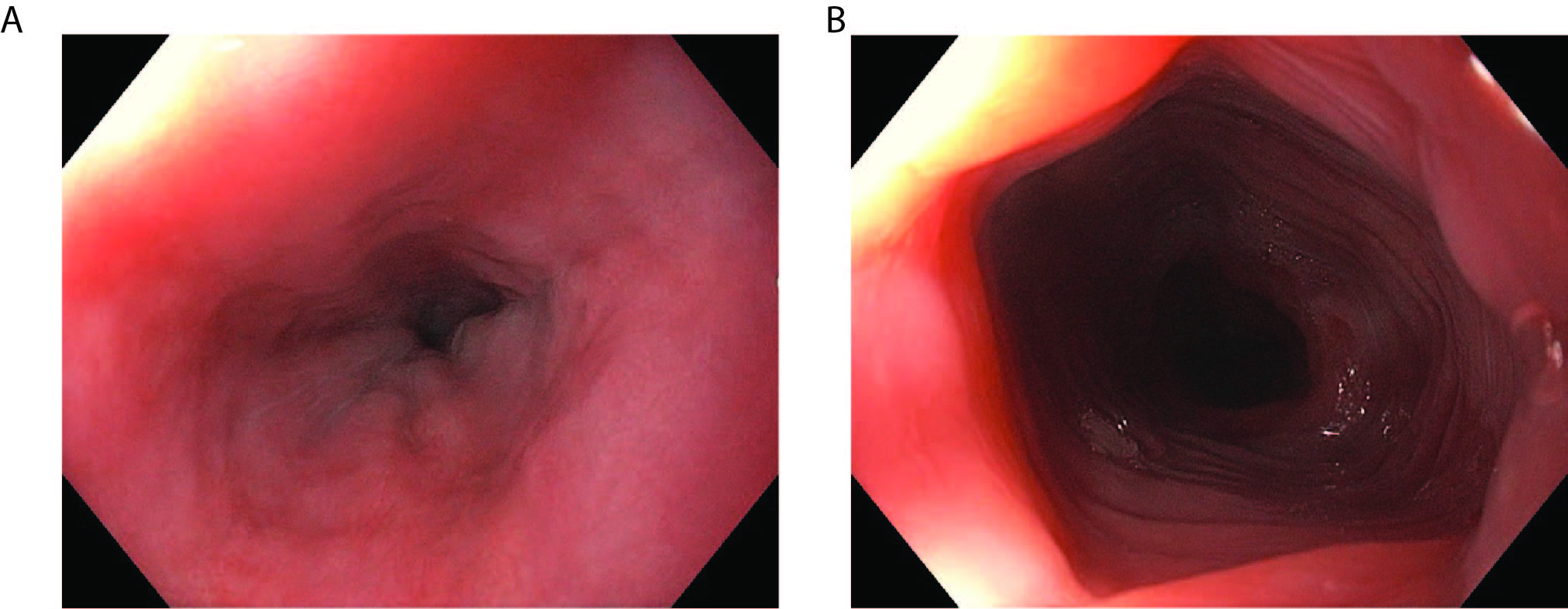
Figure:
Figure 2. Esophagogastroduodenoscopy (EGD) showed a normal mucosa throughout the entire esophagus.
Disclosures:
Yan Yan indicated no relevant financial relationships.
Osayande Osagiede indicated no relevant financial relationships.
Yichen Wang indicated no relevant financial relationships.
Maoyin Pang indicated no relevant financial relationships.
Yuting Huang indicated no relevant financial relationships.
Yan Yan, MD, PhD1, Osayande Osagiede, MBBS, MPH2, Yichen Wang, MD3, Maoyin Pang, MD, PhD1, Yuting Huang, MD, PhD1. P2831 - Dilate, Paralyze, Relieve: Multimodal Management of EGJOO in an Elderly Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic, Jacksonville, FL, US, Jacksonville, FL; 3Hospital of the University of Pennsylvania, Philadelphia, PA
Introduction: Esophagogastric junction outflow obstruction (EGJOO) is a primary esophageal motility disorder characterized by the impaired relaxation of the esophagogastric junction (EGJ) in conjunction with elevated intrabolus pressure while preserving some degree of normal peristalsis that does not fit with achalasia criteria. The EGJOO is detected in up to 14% of high-resolution manometry (HRM) studies, predominantly affecting females with an age range of 51 to 69 years old.
Case Description/
Methods: A 72-year-old woman with past medical history of restless leg syndrome, hypertension, hypothyroidism, and breast cancer with breast lumpectomy, presented with a 5-month history of dysphagia, odynophagia, and nocturnal nausea. Her symptom persisted despite empiric treatment with omeprazole, hyoscyamine, and diazepam. Initial evaluation with barium esophagram demonstrated mild to moderate focal narrowing in the midthoracic esophagus. Episodes of esophageal spasm were observed distal to the narrowing (Figure 1A, blue arrow). Esophageal manometry revealed an elevated integrated relaxation pressure (IRP) of 18.7 mmHg. Contractile activity was detected in the mid and lower segments of the esophagus (Figure 1B). Subsequent esophagogastroduodenoscopy (EGD) revealed a hypertonic lower esophageal sphincter (LES), diminished peristaltic activity, and normal mucosa in the entire esophagus (Figure 2). She was managed with sildenafil, endoscopic balloon dilation of the entire esophagus. Besides, the patient underwent two botulinum toxin injections targeting the lower and distal one-third of esophageal sphincter (LES). During follow-up, the patient reported modest symptom relief and improved tolerance of oral intake.
Discussion: The diagnosis of EGJOO was established based on clinical presentation, esophagram findings, and manometric evidence. Pharmacologic therapies, the first-line treatment of EGJOO, may offer symptomatic relief but do not correct the underlying esophageal motility disorder. Interventions targeting esophageal dysmotility include botulinum toxin injection, Pneumatic balloon dilation, laparoscopic Heller myotomy with Dor fundoplication, and POEM.
This case highlights the complexity and individualized nature of managing EGJOO, underscoring the need for further research to generate evidence-based recommendations for optimal treatment selection. A personalized treatment strategy and shared decision-making play a critical role in guiding the management of this condition.
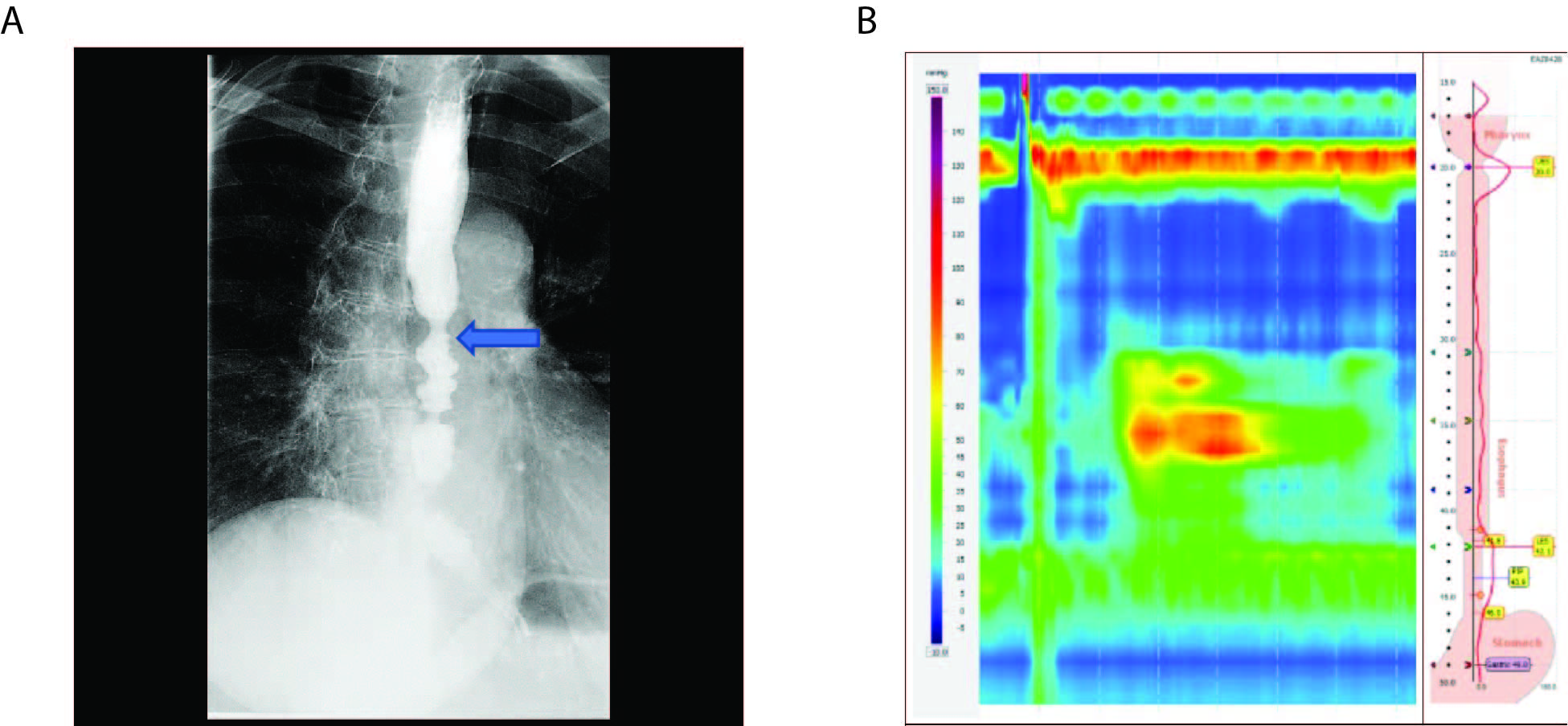
Figure: Figure 1: barium esophagram and esophageal manometry examination. (A) Barium esophagram demonstrated mild to moderate focal narrowing in the midthoracic esophagus. Episodes of esophageal spasm were observed distal to the narrowing marked with the blue arrow. (B) Esophageal manometry revealed a contractile activity in the mid and lower segments of the esophagus, characterized by an uncoordinated peristaltic sequence and pan-esophageal pressurization.
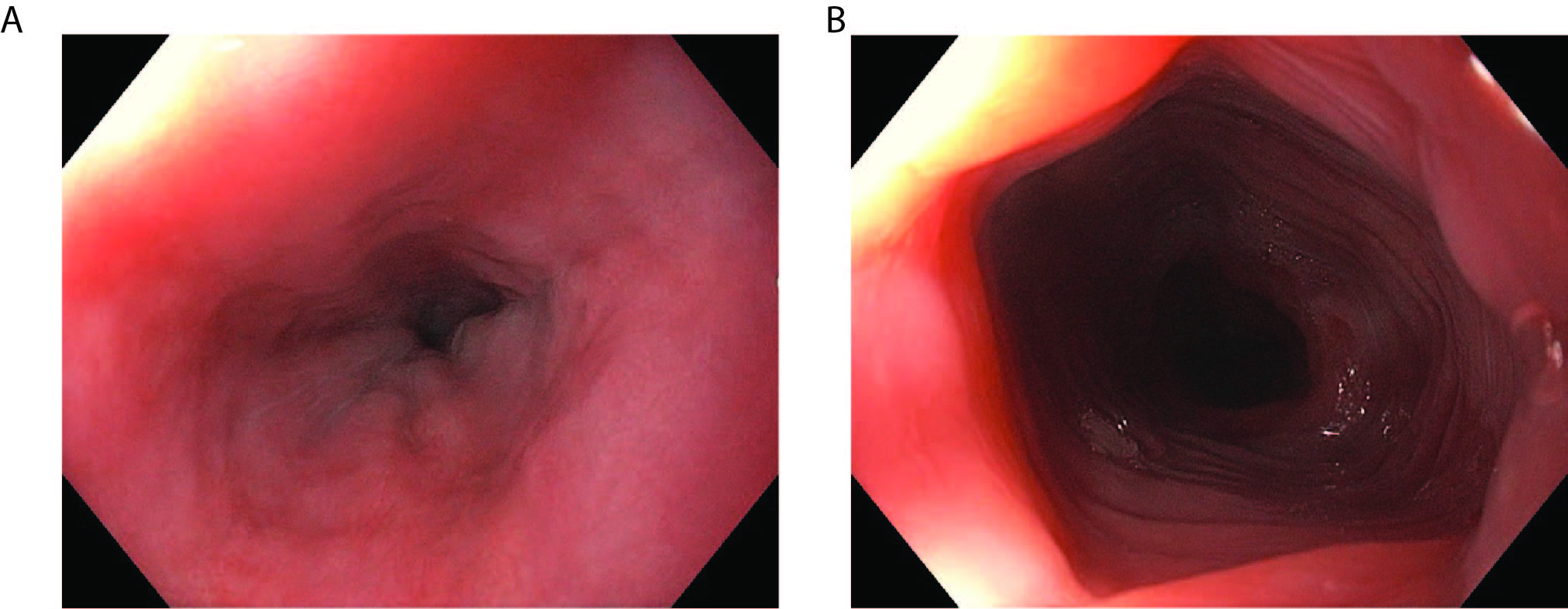
Figure:
Figure 2. Esophagogastroduodenoscopy (EGD) showed a normal mucosa throughout the entire esophagus.
Disclosures:
Yan Yan indicated no relevant financial relationships.
Osayande Osagiede indicated no relevant financial relationships.
Yichen Wang indicated no relevant financial relationships.
Maoyin Pang indicated no relevant financial relationships.
Yuting Huang indicated no relevant financial relationships.
Yan Yan, MD, PhD1, Osayande Osagiede, MBBS, MPH2, Yichen Wang, MD3, Maoyin Pang, MD, PhD1, Yuting Huang, MD, PhD1. P2831 - Dilate, Paralyze, Relieve: Multimodal Management of EGJOO in an Elderly Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
