Monday Poster Session
Category: Esophagus
P2825 - When Swallowing Stops: A Rare Case of Achalasia Presenting With Pulmonary Abscesses in an Elderly Patient
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ali Rida, MD (he/him/his)
McLaren Greater Lansing Hospital
Dearborn Heights, MI
Presenting Author(s)
Ali Rida, MD1, Claire C. Russell, DO2, Thomas Barker, MD3, Caleb Glover, DO2, Tyler Cooper, DO2, Derrick Schultz, DO2, Eric Nguyen, MD2, Edward Cay, DO4, Dorian Jones, MD3
1McLaren Greater Lansing Hospital, Dearborn Heights, MI; 2McLaren Greater Lansing Hospital, Lansing, MI; 3Michigan State University, East Lansing, MI; 4McLaren Greater Lansing, Lansing, MI
Introduction: Achalasia is a rare esophageal motility disorder defined by impaired lower esophageal sphincter (LES) relaxation and loss of peristalsis, leading to dysphagia, regurgitation, and weight loss. Though typically diagnosed between ages 25–60, achalasia can present in elderly patients, where symptoms may be misattributed to more common conditions like GERD, delaying diagnosis and increasing risk for complications such as aspiration or malnutrition [1]. Long-standing disease may result in esophageal dilation and stasis, which predispose to aspiration pneumonia and, in rare cases, pulmonary abscesses [2]. Diagnosis is confirmed with manometry, while CT and endoscopy help evaluate structural and infectious complications [3].
Case Description/
Methods: An 80-year-old male with known achalasia and spondylitis presented with progressive dysphagia, vomiting of saliva, and weakness over two weeks. He reported complete intolerance to solids and liquids. Physical exam showed signs of dehydration and malnutrition. A contrast-enhanced CT of the chest, abdomen, and pelvis revealed a markedly dilated esophagus filled with food debris and multiple right middle lobe fluid collections concerning for pulmonary abscesses (Figures 1 and 2).
Empiric IV antibiotics were initiated. Esophagogastroduodenoscopy (EGD) demonstrated a severely dilated esophagus with retained food and a fibrotic but traversable stricture at the LES. Balloon dilation was performed. Post-procedure imaging confirmed improvement in esophageal decompression.
The patient gradually improved clinically and biochemically, with resolution of fever and decreasing leukocytosis. Upon stabilization, he was referred to a tertiary center for peroral endoscopic myotomy (POEM) evaluation.
Discussion: This case highlights the severe complications of untreated achalasia, particularly in elderly patients. Esophageal dilation with retained contents can lead to chronic aspiration, which predisposes to pneumonia, and in rare cases, pulmonary abscess formation [2,4]. In one review, up to 37% of achalasia patients had pulmonary complications, though pulmonary abscesses specifically remain rare (< 2%) and are primarily reported in isolated case series [2]. The multidisciplinary approach in this case—combining endoscopic dilation, antibiotic therapy, thoracentesis, and nutritional support—was key to recovery and stabilization.

Figure: Coronal CT Image demonstrating Markedly Distended Esophagus with Debris
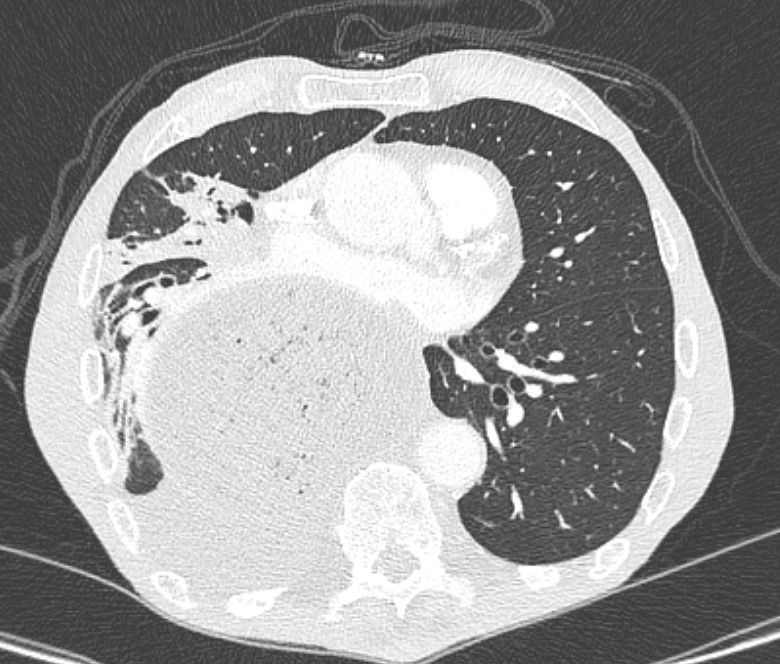
Figure: Cross-Sectional CT image again demonstrating markedly distended esophagus as well as multiple fluid collections concerning for Pulmonary Abscesses.
Disclosures:
Ali Rida indicated no relevant financial relationships.
Claire Russell indicated no relevant financial relationships.
Thomas Barker indicated no relevant financial relationships.
Caleb Glover indicated no relevant financial relationships.
Tyler Cooper indicated no relevant financial relationships.
Derrick Schultz indicated no relevant financial relationships.
Eric Nguyen indicated no relevant financial relationships.
Edward Cay indicated no relevant financial relationships.
Dorian Jones indicated no relevant financial relationships.
Ali Rida, MD1, Claire C. Russell, DO2, Thomas Barker, MD3, Caleb Glover, DO2, Tyler Cooper, DO2, Derrick Schultz, DO2, Eric Nguyen, MD2, Edward Cay, DO4, Dorian Jones, MD3. P2825 - When Swallowing Stops: A Rare Case of Achalasia Presenting With Pulmonary Abscesses in an Elderly Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1McLaren Greater Lansing Hospital, Dearborn Heights, MI; 2McLaren Greater Lansing Hospital, Lansing, MI; 3Michigan State University, East Lansing, MI; 4McLaren Greater Lansing, Lansing, MI
Introduction: Achalasia is a rare esophageal motility disorder defined by impaired lower esophageal sphincter (LES) relaxation and loss of peristalsis, leading to dysphagia, regurgitation, and weight loss. Though typically diagnosed between ages 25–60, achalasia can present in elderly patients, where symptoms may be misattributed to more common conditions like GERD, delaying diagnosis and increasing risk for complications such as aspiration or malnutrition [1]. Long-standing disease may result in esophageal dilation and stasis, which predispose to aspiration pneumonia and, in rare cases, pulmonary abscesses [2]. Diagnosis is confirmed with manometry, while CT and endoscopy help evaluate structural and infectious complications [3].
Case Description/
Methods: An 80-year-old male with known achalasia and spondylitis presented with progressive dysphagia, vomiting of saliva, and weakness over two weeks. He reported complete intolerance to solids and liquids. Physical exam showed signs of dehydration and malnutrition. A contrast-enhanced CT of the chest, abdomen, and pelvis revealed a markedly dilated esophagus filled with food debris and multiple right middle lobe fluid collections concerning for pulmonary abscesses (Figures 1 and 2).
Empiric IV antibiotics were initiated. Esophagogastroduodenoscopy (EGD) demonstrated a severely dilated esophagus with retained food and a fibrotic but traversable stricture at the LES. Balloon dilation was performed. Post-procedure imaging confirmed improvement in esophageal decompression.
The patient gradually improved clinically and biochemically, with resolution of fever and decreasing leukocytosis. Upon stabilization, he was referred to a tertiary center for peroral endoscopic myotomy (POEM) evaluation.
Discussion: This case highlights the severe complications of untreated achalasia, particularly in elderly patients. Esophageal dilation with retained contents can lead to chronic aspiration, which predisposes to pneumonia, and in rare cases, pulmonary abscess formation [2,4]. In one review, up to 37% of achalasia patients had pulmonary complications, though pulmonary abscesses specifically remain rare (< 2%) and are primarily reported in isolated case series [2]. The multidisciplinary approach in this case—combining endoscopic dilation, antibiotic therapy, thoracentesis, and nutritional support—was key to recovery and stabilization.

Figure: Coronal CT Image demonstrating Markedly Distended Esophagus with Debris
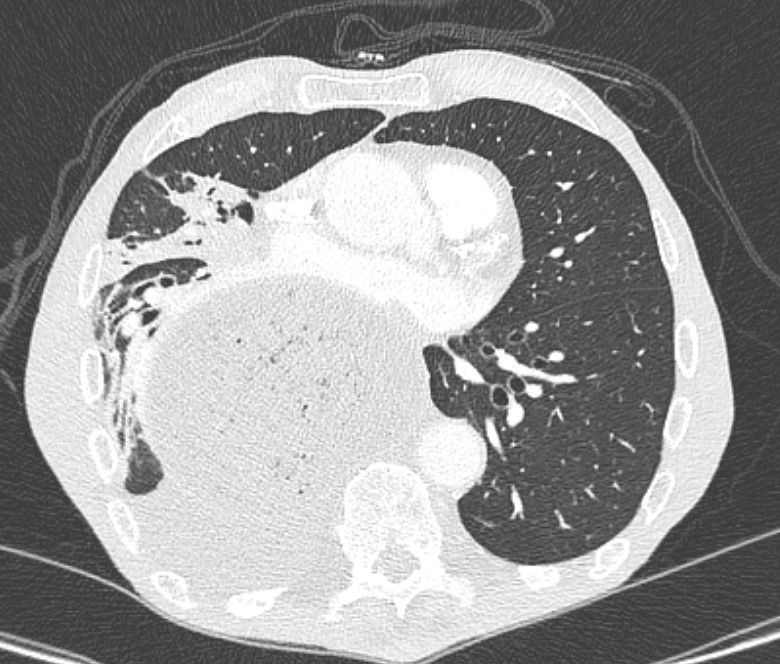
Figure: Cross-Sectional CT image again demonstrating markedly distended esophagus as well as multiple fluid collections concerning for Pulmonary Abscesses.
Disclosures:
Ali Rida indicated no relevant financial relationships.
Claire Russell indicated no relevant financial relationships.
Thomas Barker indicated no relevant financial relationships.
Caleb Glover indicated no relevant financial relationships.
Tyler Cooper indicated no relevant financial relationships.
Derrick Schultz indicated no relevant financial relationships.
Eric Nguyen indicated no relevant financial relationships.
Edward Cay indicated no relevant financial relationships.
Dorian Jones indicated no relevant financial relationships.
Ali Rida, MD1, Claire C. Russell, DO2, Thomas Barker, MD3, Caleb Glover, DO2, Tyler Cooper, DO2, Derrick Schultz, DO2, Eric Nguyen, MD2, Edward Cay, DO4, Dorian Jones, MD3. P2825 - When Swallowing Stops: A Rare Case of Achalasia Presenting With Pulmonary Abscesses in an Elderly Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
