Monday Poster Session
Category: Esophagus
P2909 - Type II Achalasia in an Adult With Sjögren’s Syndrome and Multiple Autoimmune Comorbidities: A Rare Case Report
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Abdelrhman Refaey, MD
Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences
Teaneck, NJ
Presenting Author(s)
Abdelrhman Refaey, MD, Samuel A. Schueler, MD, Marie L. Borum, MD, EdD, MPH, FACG
Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC
Introduction: Achalasia is a rare esophageal motility disorder characterized by impaired lower esophageal sphincter relaxation and loss of peristalsis. Sjögren’s syndrome, a chronic autoimmune disease affecting exocrine glands, commonly causes xerostomia and oropharyngeal dysphagia, but is rarely associated with achalasia. While the association between achalasia and juvenile Sjögren’s syndrome has been described in several cases, only a single adult case has been reported. We present a case of type II achalasia in a woman with Sjögren’s and multiple autoimmune comorbidities.
Case Description/
Methods: A 66- year-old woman with Sjögren’s syndrome, multiple sclerosis, myasthenia gravis, prediabetes, hyperthyroidism, gastroesophageal reflux disease, and history of colonic adenomas presented with one month of progressive dysphagia to solids, liquids, and pills associated with cough, daily regurgitation, and a 13-pound weight loss requiring her to modify her diet to soft foods and nutritional supplements. Her exam and labs were unremarkable.
Initial chest radiography showed a markedly dilated esophagus with an air-fluid level with no evidence of pneumonia. CT scan confirmed marked dilation of the thoracic esophagus with tapering at the gastroesophageal junction, without mass or lymphadenopathy. Barium esophagram revealed a dilated esophagus, absent peristalsis, and a narrowed gastroesophageal junction, raising suspicion for achalasia. Upper endoscopy demonstrated diffuse esophageal dilation, congestion, friability, and sloughing, and atrophic gastric mucosa and erosions (biopsies negative for H. pylori.). Despite dietary modifications, she continued to lose weight.
High-resolution esophageal manometry revealed panesophageal pressurization in all swallows and median integrated relaxation pressure (IRP) of 15.1 mm Hg, consistent with type II achalasia and corresponding with her symptoms and findings on esophagram and endoscopy. Due to suboptimal manometry catheter placement likely resulting in an underestimate of the IRP, the patient will undergo EndoFLIP for further confirmation of Type II Achalasia prior to definitive intervention.
Discussion: Although dysphagia is common in adult Sjögren’s syndrome, the association with achalasia is rare. This case highlights the importance of considering achalasia in adult Sjögren’s patients with unexplained or progressive dysphagia. Comprehensive evaluation is essential for accurate diagnosis and management strategy.

Figure: Figure 1.
(A) Axial chest CT showing a markedly dilated, air-filled esophagus without obstructing mass.
(B) Sagittal chest CT demonstrates a markedly dilated esophagus throughout its course with air-fluid levels tapering at the esophagogastric junction without discernible mass.
(C) Barium esophagram reveals a dilated esophagus with smooth tapering and delayed contrast passage at the gastroesophageal junction, consistent with achalasia.
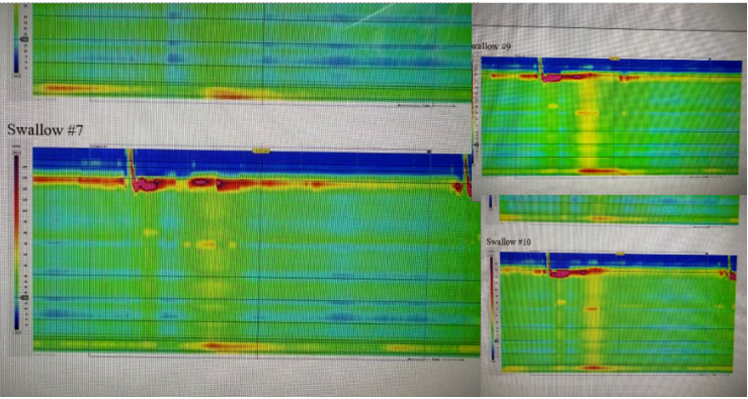
Figure: Figure 2. High resolution manometry tracings from three swallows showing pan esophageal pressurization (yellow columns) and absence of peristalsis with elevated integrated relaxation pressure, consistent with type II achalasia.
Disclosures:
Abdelrhman Refaey indicated no relevant financial relationships.
Samuel Schueler indicated no relevant financial relationships.
Marie Borum indicated no relevant financial relationships.
Abdelrhman Refaey, MD, Samuel A. Schueler, MD, Marie L. Borum, MD, EdD, MPH, FACG. P2909 - Type II Achalasia in an Adult With Sjögren’s Syndrome and Multiple Autoimmune Comorbidities: A Rare Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC
Introduction: Achalasia is a rare esophageal motility disorder characterized by impaired lower esophageal sphincter relaxation and loss of peristalsis. Sjögren’s syndrome, a chronic autoimmune disease affecting exocrine glands, commonly causes xerostomia and oropharyngeal dysphagia, but is rarely associated with achalasia. While the association between achalasia and juvenile Sjögren’s syndrome has been described in several cases, only a single adult case has been reported. We present a case of type II achalasia in a woman with Sjögren’s and multiple autoimmune comorbidities.
Case Description/
Methods: A 66- year-old woman with Sjögren’s syndrome, multiple sclerosis, myasthenia gravis, prediabetes, hyperthyroidism, gastroesophageal reflux disease, and history of colonic adenomas presented with one month of progressive dysphagia to solids, liquids, and pills associated with cough, daily regurgitation, and a 13-pound weight loss requiring her to modify her diet to soft foods and nutritional supplements. Her exam and labs were unremarkable.
Initial chest radiography showed a markedly dilated esophagus with an air-fluid level with no evidence of pneumonia. CT scan confirmed marked dilation of the thoracic esophagus with tapering at the gastroesophageal junction, without mass or lymphadenopathy. Barium esophagram revealed a dilated esophagus, absent peristalsis, and a narrowed gastroesophageal junction, raising suspicion for achalasia. Upper endoscopy demonstrated diffuse esophageal dilation, congestion, friability, and sloughing, and atrophic gastric mucosa and erosions (biopsies negative for H. pylori.). Despite dietary modifications, she continued to lose weight.
High-resolution esophageal manometry revealed panesophageal pressurization in all swallows and median integrated relaxation pressure (IRP) of 15.1 mm Hg, consistent with type II achalasia and corresponding with her symptoms and findings on esophagram and endoscopy. Due to suboptimal manometry catheter placement likely resulting in an underestimate of the IRP, the patient will undergo EndoFLIP for further confirmation of Type II Achalasia prior to definitive intervention.
Discussion: Although dysphagia is common in adult Sjögren’s syndrome, the association with achalasia is rare. This case highlights the importance of considering achalasia in adult Sjögren’s patients with unexplained or progressive dysphagia. Comprehensive evaluation is essential for accurate diagnosis and management strategy.

Figure: Figure 1.
(A) Axial chest CT showing a markedly dilated, air-filled esophagus without obstructing mass.
(B) Sagittal chest CT demonstrates a markedly dilated esophagus throughout its course with air-fluid levels tapering at the esophagogastric junction without discernible mass.
(C) Barium esophagram reveals a dilated esophagus with smooth tapering and delayed contrast passage at the gastroesophageal junction, consistent with achalasia.
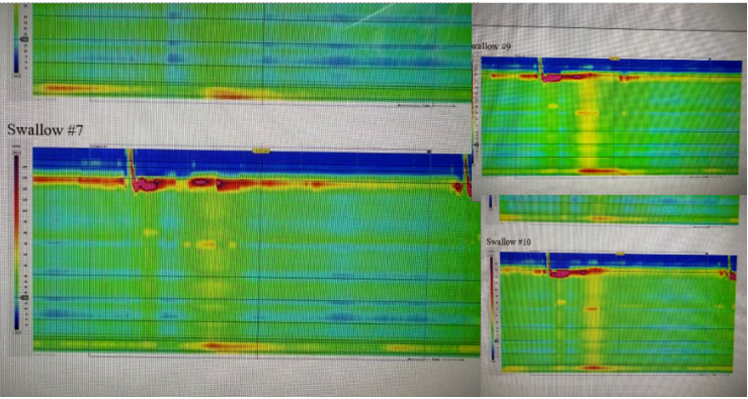
Figure: Figure 2. High resolution manometry tracings from three swallows showing pan esophageal pressurization (yellow columns) and absence of peristalsis with elevated integrated relaxation pressure, consistent with type II achalasia.
Disclosures:
Abdelrhman Refaey indicated no relevant financial relationships.
Samuel Schueler indicated no relevant financial relationships.
Marie Borum indicated no relevant financial relationships.
Abdelrhman Refaey, MD, Samuel A. Schueler, MD, Marie L. Borum, MD, EdD, MPH, FACG. P2909 - Type II Achalasia in an Adult With Sjögren’s Syndrome and Multiple Autoimmune Comorbidities: A Rare Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
