Monday Poster Session
Category: Esophagus
P2905 - Lymphocytic Esophagitis Masquerading as Eosinophilic Esophagitis: Diagnostic Challenges in an 85-Year-Old Patient
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Manasa S. Pavuloori, BSc (she/her/hers)
Oakland University William Beaumont School of Medicine
Royal Oak, MI
Presenting Author(s)
Manasa S. Pavuloori, BSc1, Nathanial Bartosek, MD2, Melina Brown, DO3, Inayat Gill, MD4, Fadi Odish, MD4
1Oakland University William Beaumont School of Medicine, Royal Oak, MI; 2Corewell Health East William Beaumont University Hospital, Royal Oak, MI; 3William Beaumont Hospital, Royal Oak, MI; 4Corewell Health, Royal Oak, MI
Introduction: Lymphocytic esophagitis (LE) is detected in 0.1-0.3% of esophageal biopsies in America, characterized by intraepithelial lymphocyte infiltration (≥20 per high-power field) and absence of significant eosinophilia (< 15 eosinophils/hpf). While sharing symptoms with eosinophilic esophagitis (EoE), LE primarily affects females (median age 51-63 years) and exhibits nonspecific endoscopic findings, including mucosal edema, erythema, rings, or normal tissue. The etiology remains unclear, though associations with autoimmune conditions, medications, and gastroesophageal reflux have been proposed. This case describes an 85-year-old woman ultimately diagnosed with LE, highlighting the importance of considering LE outside typical demographics and the diagnostic value of histopathologic evaluation.
Case Description/
Methods: An 85-year-old woman with hypertension, microscopic collagenous colitis, and 3-pack-year smoking history presented with progressive solid-food dysphagia and chronic nonproductive cough. Pantoprazole 40mg daily provided minimal symptomatic relief. She denied odynophagia, heartburn, regurgitation, weight loss, melena, NSAID use, alcohol consumption, or relevant family history.
Esophagogastroduodenoscopy revealed linear furrows, rings, and mucosal friability—classic endoscopic features of EoE. However, biopsies demonstrated dense lymphocytic infiltration ( >30 lymphocytes/hpf) with minimal eosinophilia (< 5 eosinophils/hpf), consistent with LE. Initial high-dose PPI therapy (pantoprazole 40mg twice daily) for 8 weeks failed to achieve clinical or histologic improvement. Subsequent treatment with viscous budesonide 1mg twice daily achieved complete symptom resolution and histologic remission within 12 weeks. Disease recurrence occurred within 4 weeks of medication discontinuation, necessitating maintenance budesonide therapy. Sustained clinical and endoscopic remission was maintained at 6-month follow-up.
Discussion: This case emphasizes systematic biopsy evaluation in elderly patients with dysphagia, regardless of endoscopic findings. Only ~5% of LE patients exceed 80 years, making this case diagnostically significant. Diagnostic delays in older adults may result from symptom attribution to GERD, medication effects, or age-related esophageal motility changes. Like EoE, LE appears to require maintenance therapy for sustained remission, suggesting chronic inflammatory pathophysiology. Future research should elucidate LE's natural history, optimal treatment duration, and disease associations.
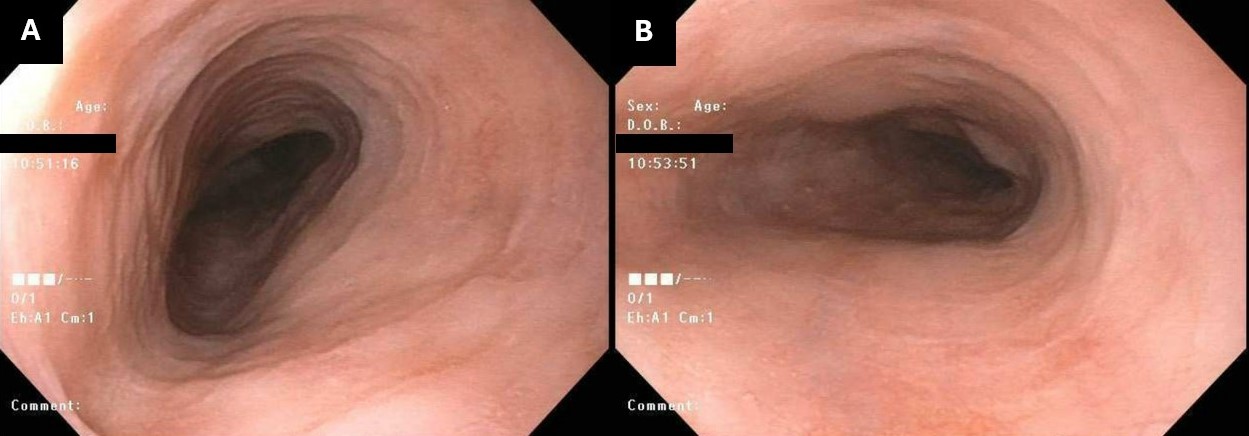
Figure: Figure 1. Mild abnormal mucosa with concentric rings in the mid (A) and distal (B) esophagus, providing initial concern for esophagitis.
Disclosures:
Manasa Pavuloori indicated no relevant financial relationships.
Nathanial Bartosek indicated no relevant financial relationships.
Melina Brown indicated no relevant financial relationships.
Inayat Gill indicated no relevant financial relationships.
Fadi Odish indicated no relevant financial relationships.
Manasa S. Pavuloori, BSc1, Nathanial Bartosek, MD2, Melina Brown, DO3, Inayat Gill, MD4, Fadi Odish, MD4. P2905 - Lymphocytic Esophagitis Masquerading as Eosinophilic Esophagitis: Diagnostic Challenges in an 85-Year-Old Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Oakland University William Beaumont School of Medicine, Royal Oak, MI; 2Corewell Health East William Beaumont University Hospital, Royal Oak, MI; 3William Beaumont Hospital, Royal Oak, MI; 4Corewell Health, Royal Oak, MI
Introduction: Lymphocytic esophagitis (LE) is detected in 0.1-0.3% of esophageal biopsies in America, characterized by intraepithelial lymphocyte infiltration (≥20 per high-power field) and absence of significant eosinophilia (< 15 eosinophils/hpf). While sharing symptoms with eosinophilic esophagitis (EoE), LE primarily affects females (median age 51-63 years) and exhibits nonspecific endoscopic findings, including mucosal edema, erythema, rings, or normal tissue. The etiology remains unclear, though associations with autoimmune conditions, medications, and gastroesophageal reflux have been proposed. This case describes an 85-year-old woman ultimately diagnosed with LE, highlighting the importance of considering LE outside typical demographics and the diagnostic value of histopathologic evaluation.
Case Description/
Methods: An 85-year-old woman with hypertension, microscopic collagenous colitis, and 3-pack-year smoking history presented with progressive solid-food dysphagia and chronic nonproductive cough. Pantoprazole 40mg daily provided minimal symptomatic relief. She denied odynophagia, heartburn, regurgitation, weight loss, melena, NSAID use, alcohol consumption, or relevant family history.
Esophagogastroduodenoscopy revealed linear furrows, rings, and mucosal friability—classic endoscopic features of EoE. However, biopsies demonstrated dense lymphocytic infiltration ( >30 lymphocytes/hpf) with minimal eosinophilia (< 5 eosinophils/hpf), consistent with LE. Initial high-dose PPI therapy (pantoprazole 40mg twice daily) for 8 weeks failed to achieve clinical or histologic improvement. Subsequent treatment with viscous budesonide 1mg twice daily achieved complete symptom resolution and histologic remission within 12 weeks. Disease recurrence occurred within 4 weeks of medication discontinuation, necessitating maintenance budesonide therapy. Sustained clinical and endoscopic remission was maintained at 6-month follow-up.
Discussion: This case emphasizes systematic biopsy evaluation in elderly patients with dysphagia, regardless of endoscopic findings. Only ~5% of LE patients exceed 80 years, making this case diagnostically significant. Diagnostic delays in older adults may result from symptom attribution to GERD, medication effects, or age-related esophageal motility changes. Like EoE, LE appears to require maintenance therapy for sustained remission, suggesting chronic inflammatory pathophysiology. Future research should elucidate LE's natural history, optimal treatment duration, and disease associations.
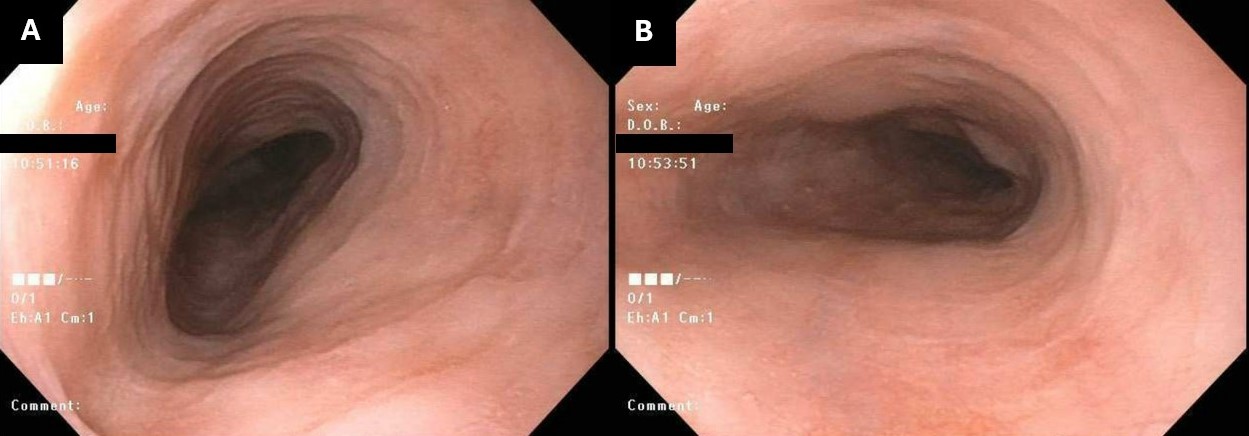
Figure: Figure 1. Mild abnormal mucosa with concentric rings in the mid (A) and distal (B) esophagus, providing initial concern for esophagitis.
Disclosures:
Manasa Pavuloori indicated no relevant financial relationships.
Nathanial Bartosek indicated no relevant financial relationships.
Melina Brown indicated no relevant financial relationships.
Inayat Gill indicated no relevant financial relationships.
Fadi Odish indicated no relevant financial relationships.
Manasa S. Pavuloori, BSc1, Nathanial Bartosek, MD2, Melina Brown, DO3, Inayat Gill, MD4, Fadi Odish, MD4. P2905 - Lymphocytic Esophagitis Masquerading as Eosinophilic Esophagitis: Diagnostic Challenges in an 85-Year-Old Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.