Monday Poster Session
Category: GI Bleeding
P3064 - Invisible Risk: Gastrointestinal Bleeding Linked to SSRI Use - A Literature Review
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AM
Amy Mackenzie, MD (she/her/hers)
HCA Florida Orange Park Hospital
Orange Park, FL
Presenting Author(s)
Mushfiqur Siddique, MD1, Mohannad Bitar, MD1, Hayder Alamily, MD2, Hina Wazir, MD1, Sukhbir Ghuman, MD1, Hasan Al-Obaidi, MD3, Amy Mackenzie, MD4
1Jamaica Hospital Medical Center, Jamaica, NY; 2University of Colorado Anschutz Medical Campus, Denver, CO; 3University of Toledo College of Medicine and Life Sciences, Toledo, OH; 4HCA Florida Orange Park Hospital, Orange Park, FL
Introduction: Selective Serotonin Reuptake Inhibitors (SSRIs) are commonly prescribed for depression
and anxiety, but growing evidence suggests a potential risk of gastrointestinal (GI) bleeding
associated with their use. Serotonin is a key mediator in platelet aggregation, and SSRIs may
impair hemostasis by depleting platelet serotonin. This review explores current findings on
the relationship between SSRI use and GI bleeding to guide safer prescribing practices.
Methods: A systematic literature search was conducted across medical databases and curated
sources. Of 192 initially identified articles, 13 met inclusion criteria for qualitative review.
Studies were selected based on relevance, inclusion of human subjects, focus on SSRI-
related bleeding risk, and availability of clinical or quantitative outcomes. Exclusion criteria
included non-English language, animal studies, and lack of bleeding-related endpoints.
Results: The 13 included studies consistently identified an increased risk of upper GI bleeding with
SSRI use. Several found a dose-response relationship, while others highlighted amplified
risk when SSRIs were taken concurrently with NSAIDs or anticoagulants. One study
demonstrated that the risk was specific to SSRIs and not shared by SNRIs. A few reports
showed that co-administration of proton pump inhibitors (PPIs) reduced the incidence of GI
bleeding. Notably, SSRIs independently increased bleeding risk even without other
contributing medications, reinforcing serotonin’s role in platelet dysfunction.
Discussion: This review supports a clinically significant association between SSRIs and GI bleeding. The
effect is biologically plausible and appears dose-related, with additive risk from common
medications such as NSAIDs. Co-prescribing gastroprotective agents like PPIs may mitigate
harm. Clinicians should weigh benefits against bleeding risks, especially in high-risk
populations, and consider the lowest effective SSRI dose when possible. More prospective
studies are needed to refine risk stratification and preventive strategies.
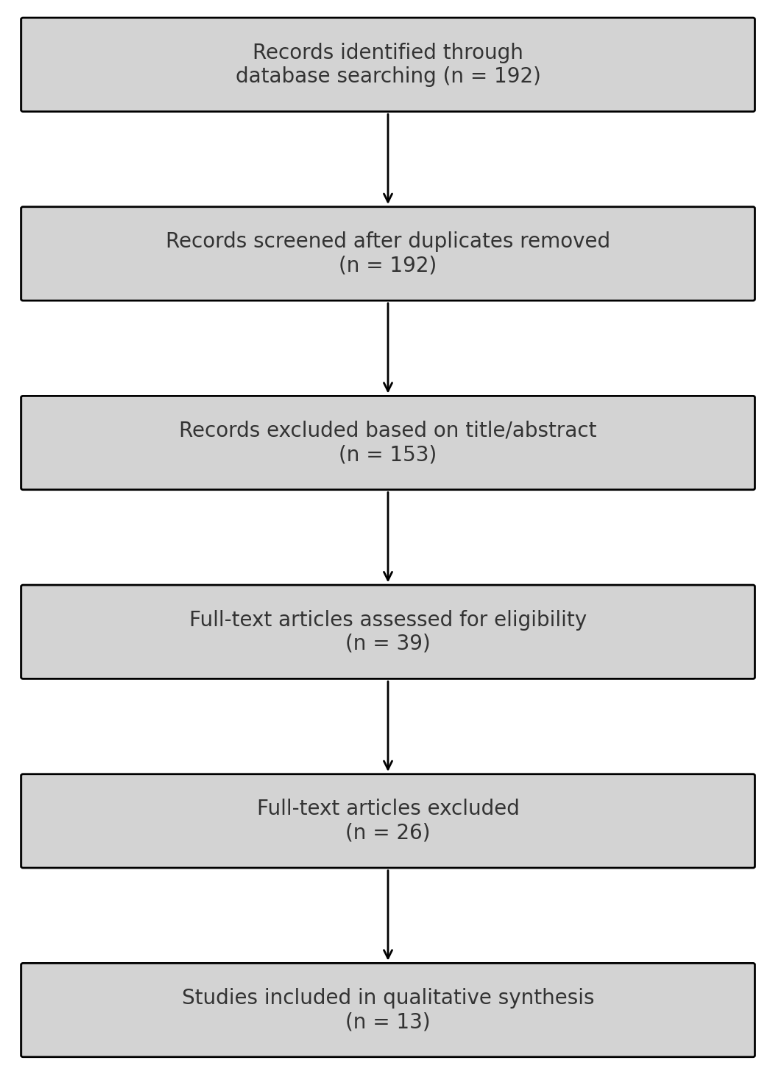
Figure: PRISMA Flowchart for Systematic Review
Disclosures:
Mushfiqur Siddique indicated no relevant financial relationships.
Mohannad Bitar indicated no relevant financial relationships.
Hayder Alamily indicated no relevant financial relationships.
Hina Wazir indicated no relevant financial relationships.
Sukhbir Ghuman indicated no relevant financial relationships.
Hasan Al-Obaidi indicated no relevant financial relationships.
Amy Mackenzie indicated no relevant financial relationships.
Mushfiqur Siddique, MD1, Mohannad Bitar, MD1, Hayder Alamily, MD2, Hina Wazir, MD1, Sukhbir Ghuman, MD1, Hasan Al-Obaidi, MD3, Amy Mackenzie, MD4. P3064 - Invisible Risk: Gastrointestinal Bleeding Linked to SSRI Use - A Literature Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Jamaica Hospital Medical Center, Jamaica, NY; 2University of Colorado Anschutz Medical Campus, Denver, CO; 3University of Toledo College of Medicine and Life Sciences, Toledo, OH; 4HCA Florida Orange Park Hospital, Orange Park, FL
Introduction: Selective Serotonin Reuptake Inhibitors (SSRIs) are commonly prescribed for depression
and anxiety, but growing evidence suggests a potential risk of gastrointestinal (GI) bleeding
associated with their use. Serotonin is a key mediator in platelet aggregation, and SSRIs may
impair hemostasis by depleting platelet serotonin. This review explores current findings on
the relationship between SSRI use and GI bleeding to guide safer prescribing practices.
Methods: A systematic literature search was conducted across medical databases and curated
sources. Of 192 initially identified articles, 13 met inclusion criteria for qualitative review.
Studies were selected based on relevance, inclusion of human subjects, focus on SSRI-
related bleeding risk, and availability of clinical or quantitative outcomes. Exclusion criteria
included non-English language, animal studies, and lack of bleeding-related endpoints.
Results: The 13 included studies consistently identified an increased risk of upper GI bleeding with
SSRI use. Several found a dose-response relationship, while others highlighted amplified
risk when SSRIs were taken concurrently with NSAIDs or anticoagulants. One study
demonstrated that the risk was specific to SSRIs and not shared by SNRIs. A few reports
showed that co-administration of proton pump inhibitors (PPIs) reduced the incidence of GI
bleeding. Notably, SSRIs independently increased bleeding risk even without other
contributing medications, reinforcing serotonin’s role in platelet dysfunction.
Discussion: This review supports a clinically significant association between SSRIs and GI bleeding. The
effect is biologically plausible and appears dose-related, with additive risk from common
medications such as NSAIDs. Co-prescribing gastroprotective agents like PPIs may mitigate
harm. Clinicians should weigh benefits against bleeding risks, especially in high-risk
populations, and consider the lowest effective SSRI dose when possible. More prospective
studies are needed to refine risk stratification and preventive strategies.
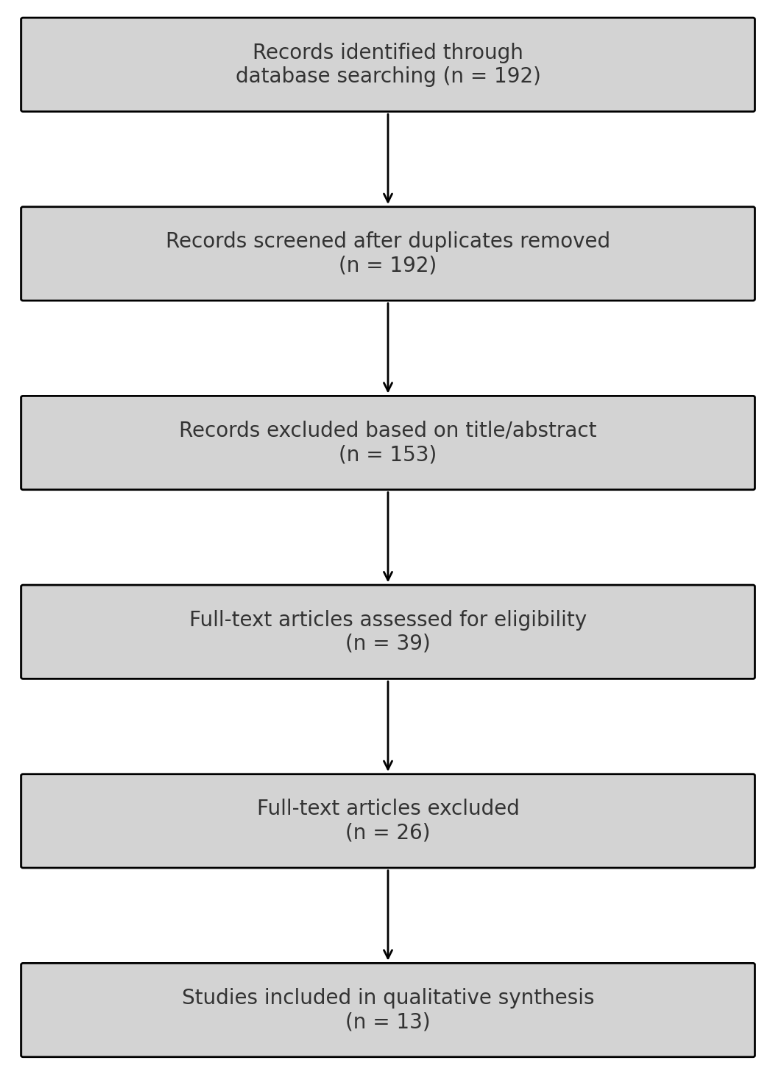
Figure: PRISMA Flowchart for Systematic Review
Disclosures:
Mushfiqur Siddique indicated no relevant financial relationships.
Mohannad Bitar indicated no relevant financial relationships.
Hayder Alamily indicated no relevant financial relationships.
Hina Wazir indicated no relevant financial relationships.
Sukhbir Ghuman indicated no relevant financial relationships.
Hasan Al-Obaidi indicated no relevant financial relationships.
Amy Mackenzie indicated no relevant financial relationships.
Mushfiqur Siddique, MD1, Mohannad Bitar, MD1, Hayder Alamily, MD2, Hina Wazir, MD1, Sukhbir Ghuman, MD1, Hasan Al-Obaidi, MD3, Amy Mackenzie, MD4. P3064 - Invisible Risk: Gastrointestinal Bleeding Linked to SSRI Use - A Literature Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
