Monday Poster Session
Category: GI Bleeding
P3061 - Evaluating the Influence of Systemic Hypertension on Mortality and Complications in Gastrointestinal Bleeding Patients: A Propensity-Matched Retrospective Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Abdelaziz Mohamed, MBBS (he/him/his)
One Brooklyn Health-Interfaith Medical Center
Brooklyn, NY
Presenting Author(s)
Abdelaziz Mohamed, MBBS1, Ali Osman, MD, MSCI Candidate2, Miqdad Dafaallah, MD3, Mohammad Adam, MD, MSc4, Fatima Elmustafa, MBBS5, Mouhand Mohamed, MBBS, MS6
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2Washington University School of Medicine in St. Louis, Ballwin, MO; 3Mercyone Des Moines Medical Center, Iowa, IA; 4University of Missouri - Kansas City School of Medicine, Kansas City, MO; 5Henry Ford Warren, Warren, MI; 6Mayo Clinic, Rochester, MN
Introduction: Gastrointestinal bleeding (GIB) is a common and serious condition associated with substantial morbidity, mortality, and healthcare burden. Hypertension (HTN) frequently coexists in patients with GIB. Although the relationship between HTN and GIB outcomes is not fully understood, some evidence suggests antihypertensive therapy may affect bleeding risk. Since hypertensive patients often receive multiple medications, this study aimed to evaluate the overall impact of HTN on mortality and other outcomes in GIB patients.
Methods: We performed a retrospective cohort study using the TriNetX Global Collaborative Network to assess the effect of HTN on outcomes in GIB patients. Two cohorts were defined: GIB with HTN (n = 233,272) and GIB without HTN (n = 233,272), matched 1:1 by propensity scores based on demographics, comorbidities, and medication use. The index event was the first recorded GIB diagnosis, with outcomes assessed up to 365 days post-index. The primary outcome was all-cause mortality. Secondary outcomes included packed red blood cell (PRBC) transfusion, recurrent GIB, and emergency room (ER) visits. Analyses included risk comparisons, Kaplan-Meier survival, and frequency of clinical events.
Results: After matching, mortality was slightly lower in the HTN+GIB group compared to the No-HTN+GIB group (5.2% vs 6.3%; risk difference -0.011 [95% CI: -0.012, -0.010]; RR 0.827; p< 0.001). One-year Kaplan-Meier survival was higher in the HTN group (93.62% vs 91.53%; HR 0.735 [95% CI: 0.717, 0.753]; p< 0.001). However, the HTN cohort had slightly higher rates of PRBC transfusion (2.6% vs 2.3%; p< 0.001), recurrent GIB (24.8% vs 26.9%; p< 0.001), and ER visits (12.0% vs 8.7%; p< 0.001). The average number of transfusions and GIB episodes was also greater in hypertensive patients(Table 1).
Discussion: This large cohort study found no increase in mortality risk in GIB patients with HTN when compared to GIB patients wihtout HTN. Nonetheless, higher rates of transfusions, recurrent bleeding, and ER visits suggest increased complication risks. Further studies are needed to better understand the effect of systemic HTN in GIB patients.
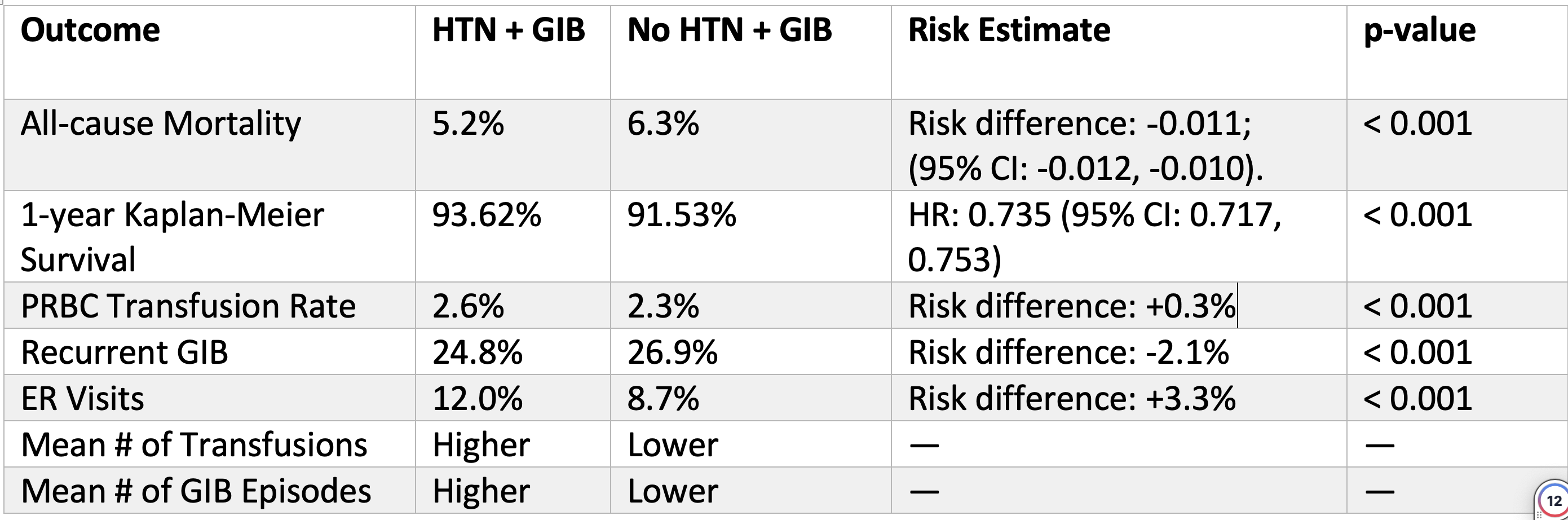
Figure: Table 1. Summary of the results and a comparison of outcomes between the two groups.
Disclosures:
Abdelaziz Mohamed indicated no relevant financial relationships.
Ali Osman indicated no relevant financial relationships.
Miqdad Dafaallah indicated no relevant financial relationships.
Mohammad Adam indicated no relevant financial relationships.
Fatima Elmustafa indicated no relevant financial relationships.
Mouhand Mohamed indicated no relevant financial relationships.
Abdelaziz Mohamed, MBBS1, Ali Osman, MD, MSCI Candidate2, Miqdad Dafaallah, MD3, Mohammad Adam, MD, MSc4, Fatima Elmustafa, MBBS5, Mouhand Mohamed, MBBS, MS6. P3061 - Evaluating the Influence of Systemic Hypertension on Mortality and Complications in Gastrointestinal Bleeding Patients: A Propensity-Matched Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2Washington University School of Medicine in St. Louis, Ballwin, MO; 3Mercyone Des Moines Medical Center, Iowa, IA; 4University of Missouri - Kansas City School of Medicine, Kansas City, MO; 5Henry Ford Warren, Warren, MI; 6Mayo Clinic, Rochester, MN
Introduction: Gastrointestinal bleeding (GIB) is a common and serious condition associated with substantial morbidity, mortality, and healthcare burden. Hypertension (HTN) frequently coexists in patients with GIB. Although the relationship between HTN and GIB outcomes is not fully understood, some evidence suggests antihypertensive therapy may affect bleeding risk. Since hypertensive patients often receive multiple medications, this study aimed to evaluate the overall impact of HTN on mortality and other outcomes in GIB patients.
Methods: We performed a retrospective cohort study using the TriNetX Global Collaborative Network to assess the effect of HTN on outcomes in GIB patients. Two cohorts were defined: GIB with HTN (n = 233,272) and GIB without HTN (n = 233,272), matched 1:1 by propensity scores based on demographics, comorbidities, and medication use. The index event was the first recorded GIB diagnosis, with outcomes assessed up to 365 days post-index. The primary outcome was all-cause mortality. Secondary outcomes included packed red blood cell (PRBC) transfusion, recurrent GIB, and emergency room (ER) visits. Analyses included risk comparisons, Kaplan-Meier survival, and frequency of clinical events.
Results: After matching, mortality was slightly lower in the HTN+GIB group compared to the No-HTN+GIB group (5.2% vs 6.3%; risk difference -0.011 [95% CI: -0.012, -0.010]; RR 0.827; p< 0.001). One-year Kaplan-Meier survival was higher in the HTN group (93.62% vs 91.53%; HR 0.735 [95% CI: 0.717, 0.753]; p< 0.001). However, the HTN cohort had slightly higher rates of PRBC transfusion (2.6% vs 2.3%; p< 0.001), recurrent GIB (24.8% vs 26.9%; p< 0.001), and ER visits (12.0% vs 8.7%; p< 0.001). The average number of transfusions and GIB episodes was also greater in hypertensive patients(Table 1).
Discussion: This large cohort study found no increase in mortality risk in GIB patients with HTN when compared to GIB patients wihtout HTN. Nonetheless, higher rates of transfusions, recurrent bleeding, and ER visits suggest increased complication risks. Further studies are needed to better understand the effect of systemic HTN in GIB patients.
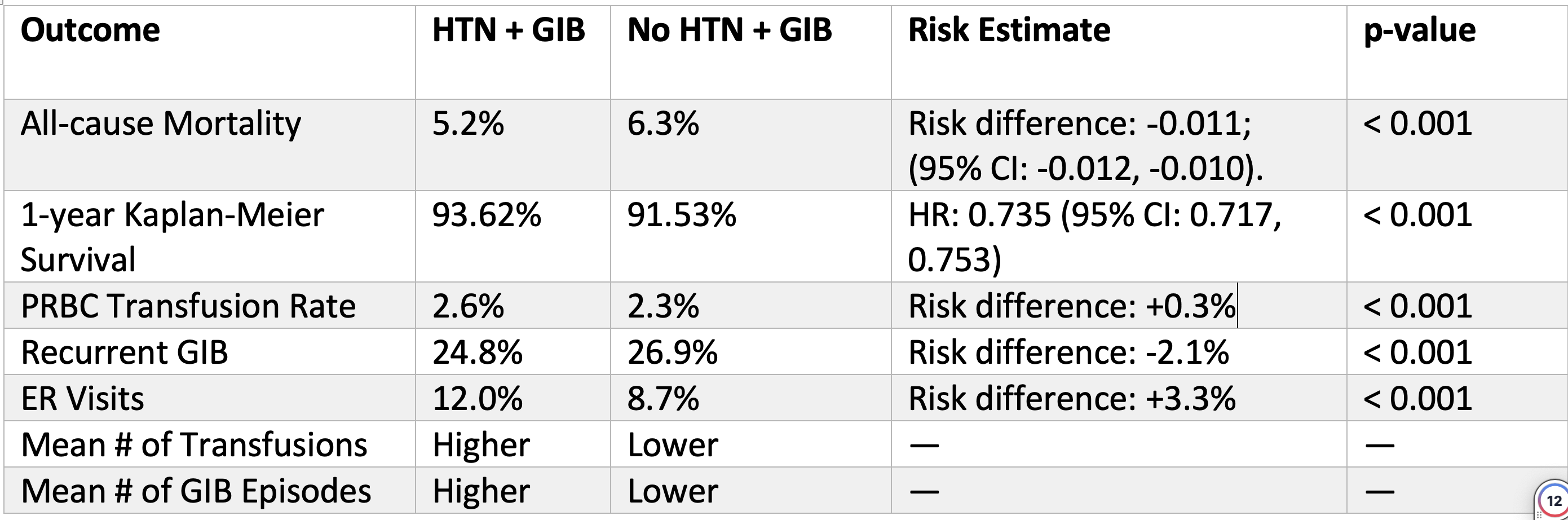
Figure: Table 1. Summary of the results and a comparison of outcomes between the two groups.
Disclosures:
Abdelaziz Mohamed indicated no relevant financial relationships.
Ali Osman indicated no relevant financial relationships.
Miqdad Dafaallah indicated no relevant financial relationships.
Mohammad Adam indicated no relevant financial relationships.
Fatima Elmustafa indicated no relevant financial relationships.
Mouhand Mohamed indicated no relevant financial relationships.
Abdelaziz Mohamed, MBBS1, Ali Osman, MD, MSCI Candidate2, Miqdad Dafaallah, MD3, Mohammad Adam, MD, MSc4, Fatima Elmustafa, MBBS5, Mouhand Mohamed, MBBS, MS6. P3061 - Evaluating the Influence of Systemic Hypertension on Mortality and Complications in Gastrointestinal Bleeding Patients: A Propensity-Matched Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
