Monday Poster Session
Category: GI Bleeding
P3057 - Proton Pump Inhibitors Reduce GI Bleeding Risk in Patients Receiving Clopidogrel Therapy Post-Percutaneous Coronary Intervention
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RT
Rahul Tripathi, MD
Stony Brook Medicine
Stony Brook, NY
Presenting Author(s)
Rahul Tripathi, MD1, James Lee, MD2, Shivani Gupta, MD1, Nezar Zeidan, DO1, Alexander Kaiteris, DO1, Alan Abboud, MD1, Michael Tao, MD3, Daniel Jamorabo, MD4
1Stony Brook Medicine, Stony Brook, NY; 2Stony Brook University Hospital, Stony Brook, NY; 3Hartford HealthCare, Middletown, CT; 4Northwell Health, Forest Hills, NY
Introduction: Concurrent administration of proton pump inhibitors (PPIs) and Clopidogrel in patients undergoing percutaneous coronary intervention (PCI) has potential drug-drug interactions undermining clopidogrel’s efficacy. Although there is abundant literature on the pharmacokinetics of taking a PPI simultaneously with clopidogrel, the clinical outcomes are unclear. This meta-analysis aims to investigate potential clinical outcomes associated with the post-PCI utilization of PPI with clopidogrel on clinical outcomes.
Methods: A literature search was performed using the databases Pubmed, Embase, and the Web of Science, identifying studies that evaluated the association of post-PCI outcomes with concomitant administration of a PPI and clopidogrel. Large database and observational studies were excluded. The endpoints of interest included major adverse cardiac events (MACE), mortality, myocardial infarction (MI), and gastrointestinal bleeding (GIB).
Results: Nine randomized controlled trials with 6359 patients met the inclusion criteria. There were 2858 patients who were treated with PPI and clopidogrel, compared to 3501 treated with only clopidogrel after PCI.
There was no significant difference between the two groups regarding mortality (OR 1.56 95% CI 0.98-2.49, P=0.06), MI (OR 1.22 95% CI 0.85-1.76, P=0.28), or MACE (OR 1.23 95% CI 0.95-1.60, P=0.11), as shown in Figures 1a, 1b, and 1c. We found a significant reduction in the risk for GIB, however, when clopidogrel was given with a PPI compared to those patients who were only on clopidogrel post-PCI (OR 0.30 CI 95% 0.17-0.55, P< 0.0001), as highlighted in Figure 1d.
Discussion: Our study identified a statistically significant protective effect of concurrent PPI use against gastrointestinal bleeding in patients who were given clopidogrel post-PCI. We found no mortality benefit or significant reduction in MACE or MI risk with dual PPI-clopidogrel therapy, so we could not corroborate pharmacokinetic evidence indicating potential interference between PPIs and clopidogrel. The reduction in GIB risk, however, underscores the healing effects that PPIs have in the upper GI tract, which is particularly important in patient populations who are at higher risk of developing GI bleeding. Further studies are nonetheless warranted to clarify any drug-drug interactions between PPIs and clopidogrel in a real-world setting.
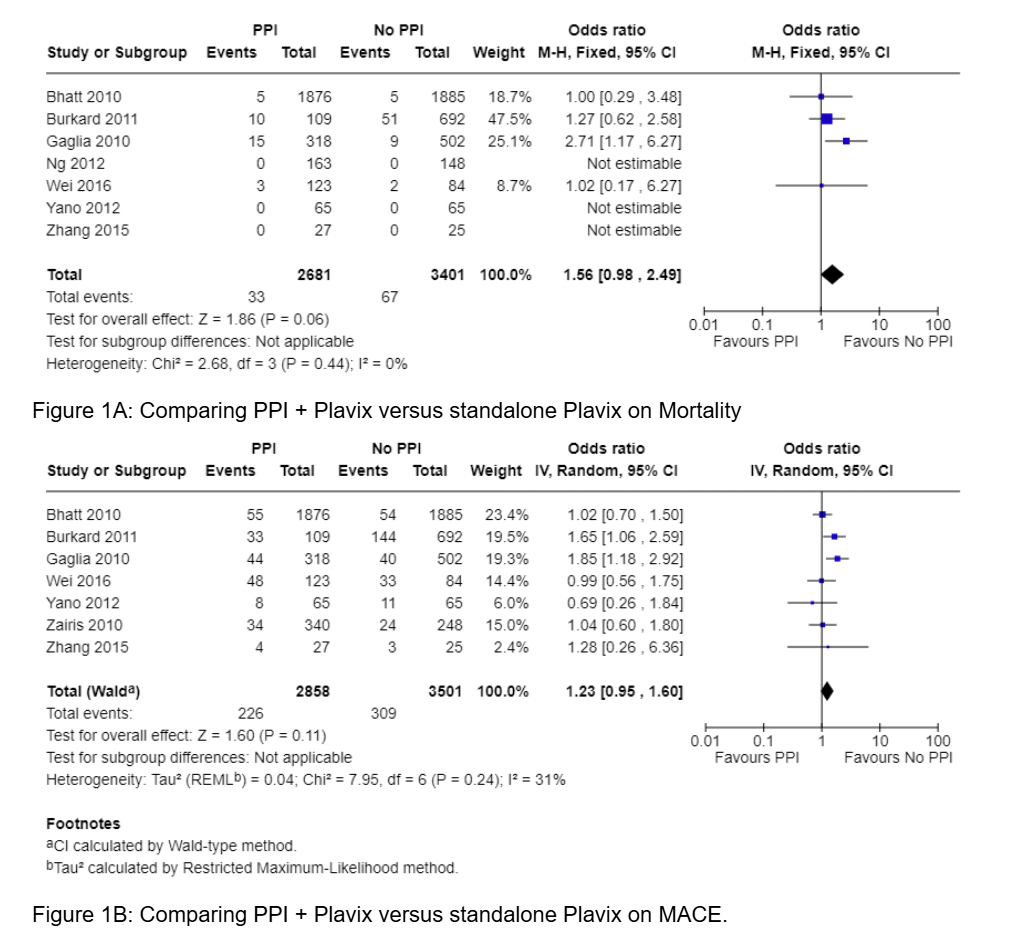
Figure: Figure 1A: Comparing PPI + Plavix versus standalone Plavix on Mortality
Figure 1B: Comparing PPI + Plavix versus standalone Plavix on MACE.
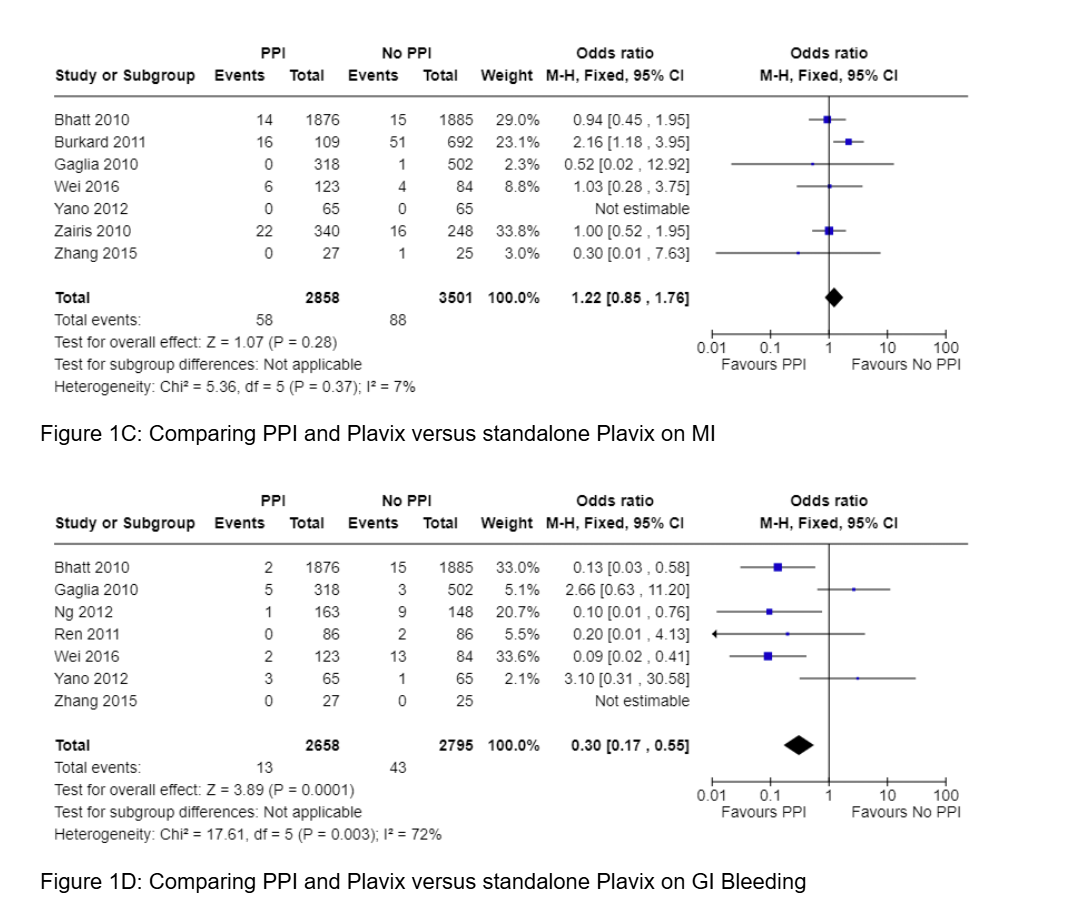
Figure: Figure 1C: Comparing PPI and Plavix versus standalone Plavix on MI
Figure 1D: Comparing PPI and Plavix versus standalone Plavix on GI Bleeding
Disclosures:
Rahul Tripathi indicated no relevant financial relationships.
James Lee indicated no relevant financial relationships.
Shivani Gupta indicated no relevant financial relationships.
Nezar Zeidan indicated no relevant financial relationships.
Alexander Kaiteris indicated no relevant financial relationships.
Alan Abboud indicated no relevant financial relationships.
Michael Tao indicated no relevant financial relationships.
Daniel Jamorabo indicated no relevant financial relationships.
Rahul Tripathi, MD1, James Lee, MD2, Shivani Gupta, MD1, Nezar Zeidan, DO1, Alexander Kaiteris, DO1, Alan Abboud, MD1, Michael Tao, MD3, Daniel Jamorabo, MD4. P3057 - Proton Pump Inhibitors Reduce GI Bleeding Risk in Patients Receiving Clopidogrel Therapy Post-Percutaneous Coronary Intervention, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Stony Brook Medicine, Stony Brook, NY; 2Stony Brook University Hospital, Stony Brook, NY; 3Hartford HealthCare, Middletown, CT; 4Northwell Health, Forest Hills, NY
Introduction: Concurrent administration of proton pump inhibitors (PPIs) and Clopidogrel in patients undergoing percutaneous coronary intervention (PCI) has potential drug-drug interactions undermining clopidogrel’s efficacy. Although there is abundant literature on the pharmacokinetics of taking a PPI simultaneously with clopidogrel, the clinical outcomes are unclear. This meta-analysis aims to investigate potential clinical outcomes associated with the post-PCI utilization of PPI with clopidogrel on clinical outcomes.
Methods: A literature search was performed using the databases Pubmed, Embase, and the Web of Science, identifying studies that evaluated the association of post-PCI outcomes with concomitant administration of a PPI and clopidogrel. Large database and observational studies were excluded. The endpoints of interest included major adverse cardiac events (MACE), mortality, myocardial infarction (MI), and gastrointestinal bleeding (GIB).
Results: Nine randomized controlled trials with 6359 patients met the inclusion criteria. There were 2858 patients who were treated with PPI and clopidogrel, compared to 3501 treated with only clopidogrel after PCI.
There was no significant difference between the two groups regarding mortality (OR 1.56 95% CI 0.98-2.49, P=0.06), MI (OR 1.22 95% CI 0.85-1.76, P=0.28), or MACE (OR 1.23 95% CI 0.95-1.60, P=0.11), as shown in Figures 1a, 1b, and 1c. We found a significant reduction in the risk for GIB, however, when clopidogrel was given with a PPI compared to those patients who were only on clopidogrel post-PCI (OR 0.30 CI 95% 0.17-0.55, P< 0.0001), as highlighted in Figure 1d.
Discussion: Our study identified a statistically significant protective effect of concurrent PPI use against gastrointestinal bleeding in patients who were given clopidogrel post-PCI. We found no mortality benefit or significant reduction in MACE or MI risk with dual PPI-clopidogrel therapy, so we could not corroborate pharmacokinetic evidence indicating potential interference between PPIs and clopidogrel. The reduction in GIB risk, however, underscores the healing effects that PPIs have in the upper GI tract, which is particularly important in patient populations who are at higher risk of developing GI bleeding. Further studies are nonetheless warranted to clarify any drug-drug interactions between PPIs and clopidogrel in a real-world setting.
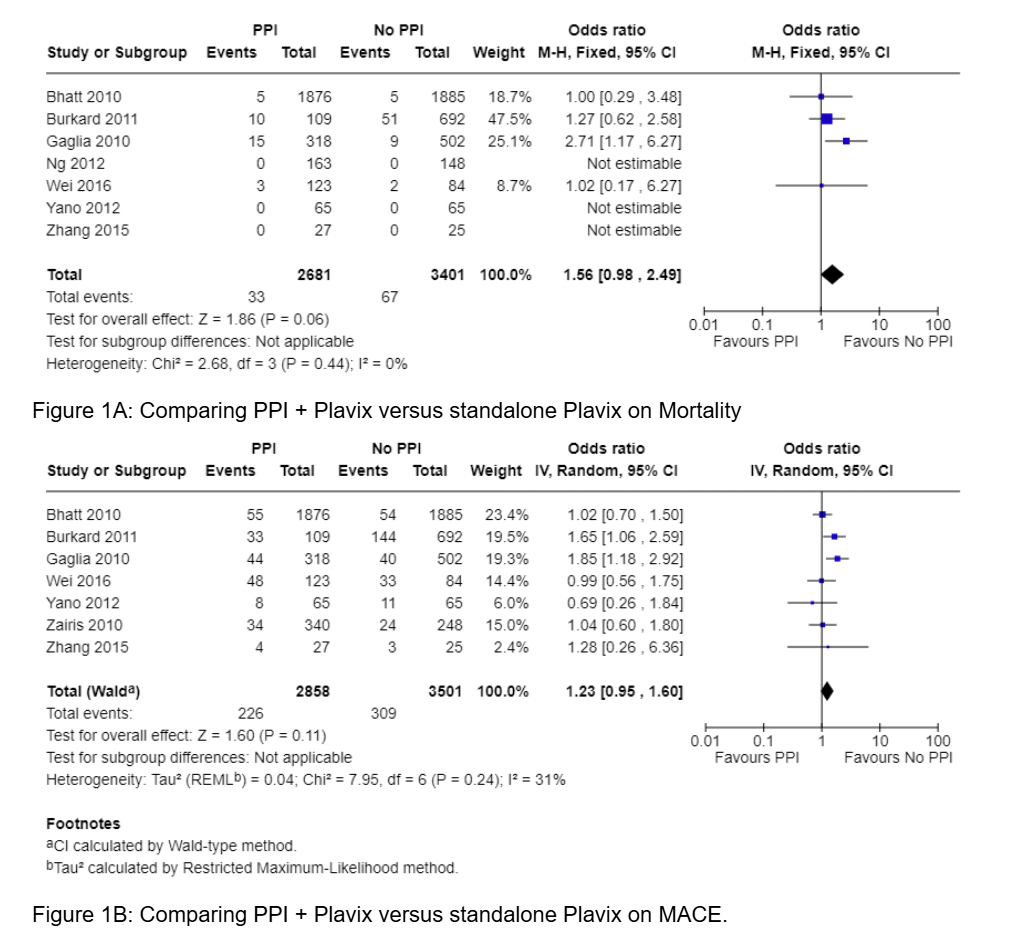
Figure: Figure 1A: Comparing PPI + Plavix versus standalone Plavix on Mortality
Figure 1B: Comparing PPI + Plavix versus standalone Plavix on MACE.
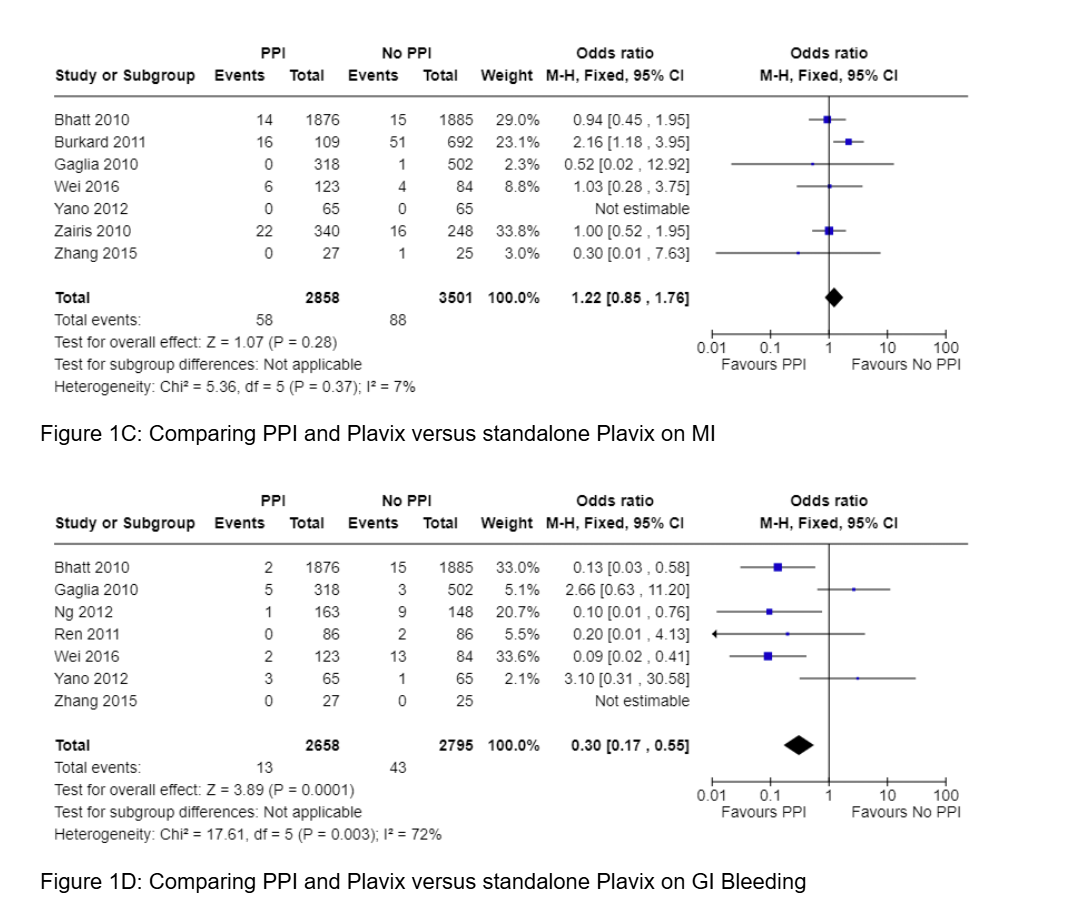
Figure: Figure 1C: Comparing PPI and Plavix versus standalone Plavix on MI
Figure 1D: Comparing PPI and Plavix versus standalone Plavix on GI Bleeding
Disclosures:
Rahul Tripathi indicated no relevant financial relationships.
James Lee indicated no relevant financial relationships.
Shivani Gupta indicated no relevant financial relationships.
Nezar Zeidan indicated no relevant financial relationships.
Alexander Kaiteris indicated no relevant financial relationships.
Alan Abboud indicated no relevant financial relationships.
Michael Tao indicated no relevant financial relationships.
Daniel Jamorabo indicated no relevant financial relationships.
Rahul Tripathi, MD1, James Lee, MD2, Shivani Gupta, MD1, Nezar Zeidan, DO1, Alexander Kaiteris, DO1, Alan Abboud, MD1, Michael Tao, MD3, Daniel Jamorabo, MD4. P3057 - Proton Pump Inhibitors Reduce GI Bleeding Risk in Patients Receiving Clopidogrel Therapy Post-Percutaneous Coronary Intervention, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
