Monday Poster Session
Category: GI Bleeding
P3056 - Role of Bridging Anticoagulation in High-Risk Atrial Fibrillation Patients During EGD and Colonoscopy: A Nationwide Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nisar Amin, MD
Charleston Area Medical Center
Charleston, WV
Presenting Author(s)
Nisar Amin, MD1, Harleen Chela, MD1, Julton Tomanguillo, MD1, Veysel Tahan, MD, FACG2, Ebubekir Daglilar, MD1
1Charleston Area Medical Center, Charleston, WV; 2Northeast Ohio Medical University & CAMC, Charleston, WV
Introduction: The role of perioperative bridging anticoagulation in patients with atrial fibrillation (AF) on warfarin remains controversial. The BRIDGE trial demonstrated that foregoing bridging is non-inferior to bridging in stroke prevention; however, it included few patients with high thromboembolic risk. Current guidelines lack specific recommendations for patients with elevated CHA₂DS₂-VASc scores. This retrospective study investigates the risks and benefits of bridging anticoagulation in patients with a CHA₂DS₂-VASc score >5 undergoing EGD and colonoscopy.
Methods: We conducted a retrospective cohort study using the TriNetX de-identified database. Patients with AF and CHA₂DS₂-VASc >5 undergoing EGD or colonoscopy were grouped based on whether they received perioperative bridging with low molecular weight heparin (LMWH). Patients with mechanical mitral or aortic valves, antiphospholipid syndrome, deep vein thrombosis or pulmonary embolism, platelet count < 100,000/µL, or creatinine clearance < 30 mL/min were excluded. Propensity score matching was used to adjust for baseline differences. The primary outcome was 90-day risk of stroke or TIA. Secondary outcomes included major bleeding, clinically relevant non-major bleeding, thrombosis, and all-cause mortality within 90 days post-procedure.
Results: Among 13,126 patients with (AF) on warfarin undergoing EGD or colonoscopy, 841 (6.4%) received bridging anticoagulation with LMWH, while 12,285 (93.6%) did not. After 1:1 propensity score matching, 816 patients were included in each group with balanced baseline characteristics.
The 90-day incidence of stroke or TIA was comparable between the bridged and non-bridged groups (2.7% vs. 2.6%, p = 0.95), showing no significant thromboembolic benefit from bridging. There was no significant difference in the 90-day incidence of gastrointestinal bleeding (5.9% vs. 4.9%, p = 0.48), intracranial hemorrhage (1.27% vs. 1.27%, p = 0.99), or systemic thrombosis (1.2% vs. 1.4%, p = 0.81). All-cause mortality at 90 days was similar between groups (5.8% vs. 6.1%, p = 0.75). (Figure1)
Discussion: In high-risk AF patients (CHA₂DS₂-VASc >5) undergoing EGD or colonoscopy, perioperative bridging with LMWH did not reduce the risk of stroke or TIA and was associated with a non-significant increase in bleeding and no difference in mortality. Consistent with prior studies showing elevated bleeding risk with bridging, our findings do not support routine use of bridging anticoagulation in this high-risk population.
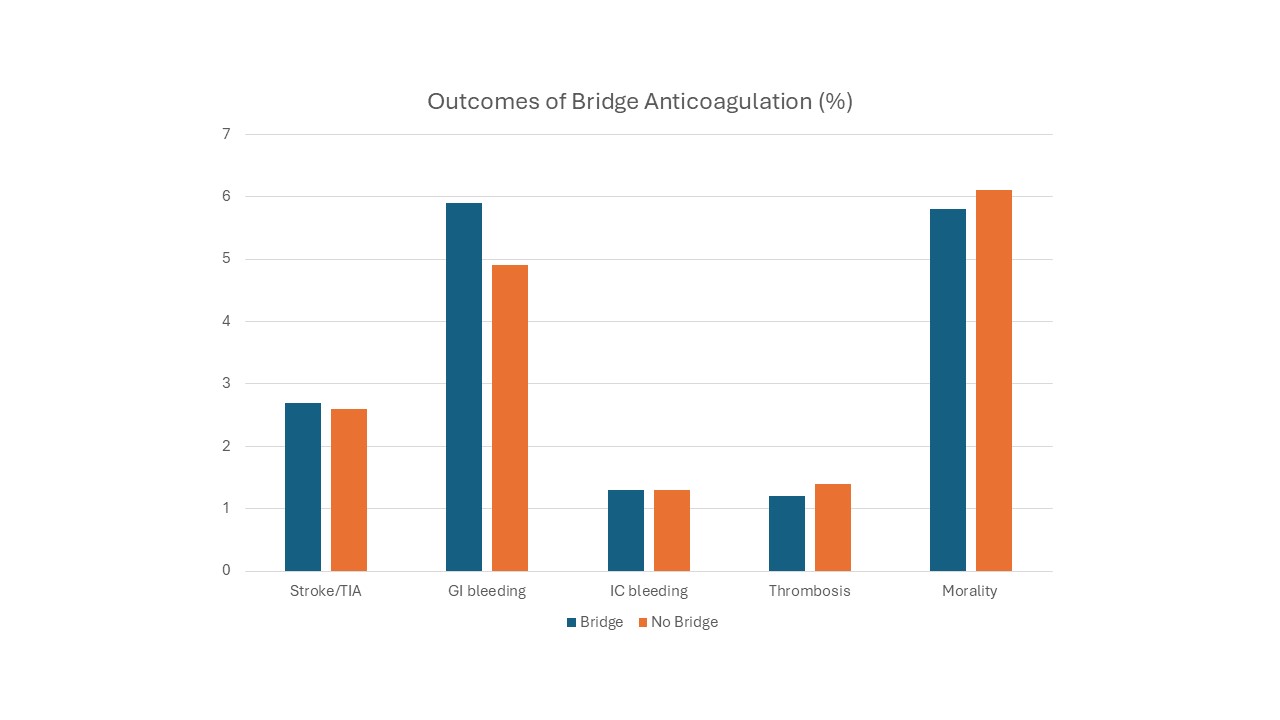
Figure: Figure-1. Outcomes of bridge anticoagulation in patients with atrial fibrillation on Warfarin who underwent EGD/Colonoscopy.
Disclosures:
Nisar Amin indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Julton Tomanguillo indicated no relevant financial relationships.
Veysel Tahan indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Nisar Amin, MD1, Harleen Chela, MD1, Julton Tomanguillo, MD1, Veysel Tahan, MD, FACG2, Ebubekir Daglilar, MD1. P3056 - Role of Bridging Anticoagulation in High-Risk Atrial Fibrillation Patients During EGD and Colonoscopy: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Charleston Area Medical Center, Charleston, WV; 2Northeast Ohio Medical University & CAMC, Charleston, WV
Introduction: The role of perioperative bridging anticoagulation in patients with atrial fibrillation (AF) on warfarin remains controversial. The BRIDGE trial demonstrated that foregoing bridging is non-inferior to bridging in stroke prevention; however, it included few patients with high thromboembolic risk. Current guidelines lack specific recommendations for patients with elevated CHA₂DS₂-VASc scores. This retrospective study investigates the risks and benefits of bridging anticoagulation in patients with a CHA₂DS₂-VASc score >5 undergoing EGD and colonoscopy.
Methods: We conducted a retrospective cohort study using the TriNetX de-identified database. Patients with AF and CHA₂DS₂-VASc >5 undergoing EGD or colonoscopy were grouped based on whether they received perioperative bridging with low molecular weight heparin (LMWH). Patients with mechanical mitral or aortic valves, antiphospholipid syndrome, deep vein thrombosis or pulmonary embolism, platelet count < 100,000/µL, or creatinine clearance < 30 mL/min were excluded. Propensity score matching was used to adjust for baseline differences. The primary outcome was 90-day risk of stroke or TIA. Secondary outcomes included major bleeding, clinically relevant non-major bleeding, thrombosis, and all-cause mortality within 90 days post-procedure.
Results: Among 13,126 patients with (AF) on warfarin undergoing EGD or colonoscopy, 841 (6.4%) received bridging anticoagulation with LMWH, while 12,285 (93.6%) did not. After 1:1 propensity score matching, 816 patients were included in each group with balanced baseline characteristics.
The 90-day incidence of stroke or TIA was comparable between the bridged and non-bridged groups (2.7% vs. 2.6%, p = 0.95), showing no significant thromboembolic benefit from bridging. There was no significant difference in the 90-day incidence of gastrointestinal bleeding (5.9% vs. 4.9%, p = 0.48), intracranial hemorrhage (1.27% vs. 1.27%, p = 0.99), or systemic thrombosis (1.2% vs. 1.4%, p = 0.81). All-cause mortality at 90 days was similar between groups (5.8% vs. 6.1%, p = 0.75). (Figure1)
Discussion: In high-risk AF patients (CHA₂DS₂-VASc >5) undergoing EGD or colonoscopy, perioperative bridging with LMWH did not reduce the risk of stroke or TIA and was associated with a non-significant increase in bleeding and no difference in mortality. Consistent with prior studies showing elevated bleeding risk with bridging, our findings do not support routine use of bridging anticoagulation in this high-risk population.
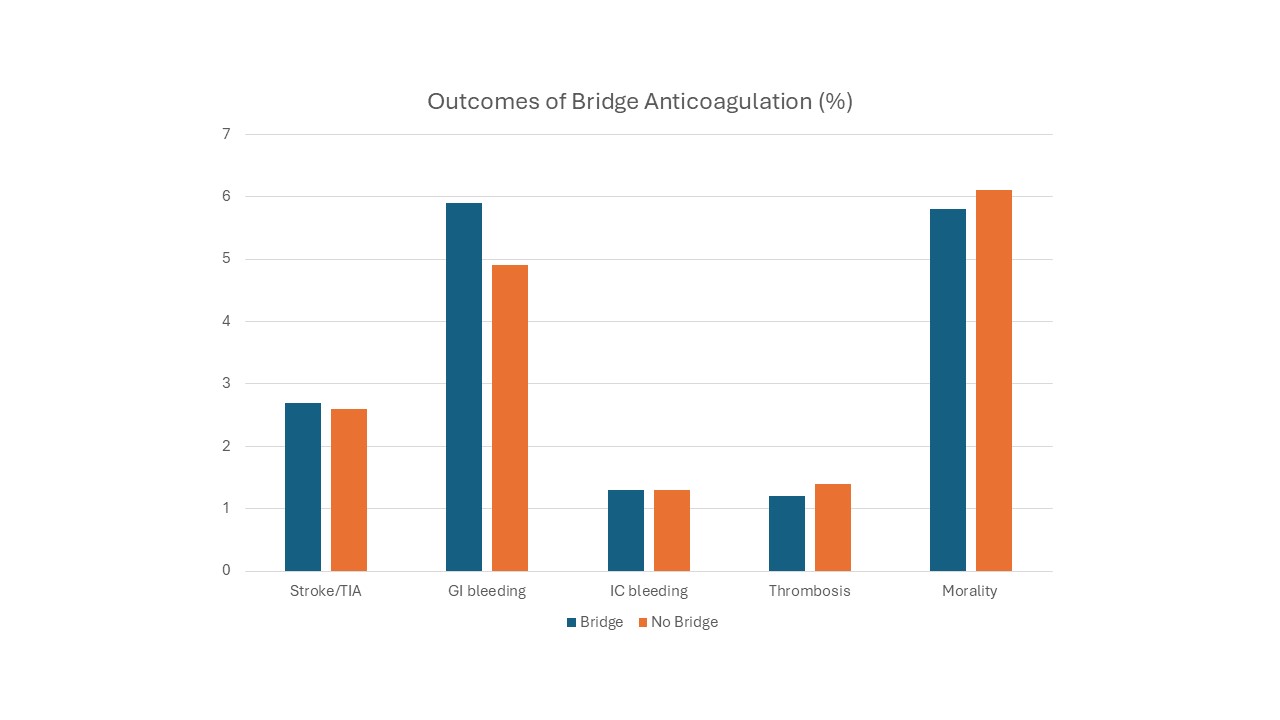
Figure: Figure-1. Outcomes of bridge anticoagulation in patients with atrial fibrillation on Warfarin who underwent EGD/Colonoscopy.
Disclosures:
Nisar Amin indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Julton Tomanguillo indicated no relevant financial relationships.
Veysel Tahan indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Nisar Amin, MD1, Harleen Chela, MD1, Julton Tomanguillo, MD1, Veysel Tahan, MD, FACG2, Ebubekir Daglilar, MD1. P3056 - Role of Bridging Anticoagulation in High-Risk Atrial Fibrillation Patients During EGD and Colonoscopy: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

