Monday Poster Session
Category: GI Bleeding
P3055 - Upper Gastrointestinal Bleeding After Acute Myocardial Infarction: Incidence, Predictors, and COVID-Era Comparison
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Yilin Song, MD (she/her/hers)
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Thai Hau Koo, MD1, Yilin Song, MD2, Stephen Firkins, MD3, Roberto Simons-Linares, MD3
1University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 2University of Maryland Medical Center, Baltimore, MD; 3Gastroenterology and Hepatology, Cleveland Clinic, Cleveland, OH
Introduction: Upper gastrointestinal bleeding (UGIB) is one of the complications of acute myocardial infarction (AMI) associated with poor outcomes. We aimed to evaluate the incidence and risk factors of UGIB within the first 30-day following AMI across the US nation for the past 15 years since FDA approval of direct oral anticoagulants (DOAC) in October 2010, and a subgroup of pre- and post-COVID era.
Methods: This retrospective cohort study analyzed data from the TriNetX database, encompassing over 275 million de-identified patient records. All inpatients from the US aged ≥ 18 years diagnosed with AMI were identified between October 2010 and May 2025. We defined UGIB events as all clinical and endoscopic diagnoses of UGIB occurring within a 30-day follow-up period after the AMI hospitalization. Patients with UGIB diagnosis that occurred before or during the AMI hospitalization were excluded. Patients who went through AMI without developing UGIB were classified into the control group. Propensity score matching was applied based on demographics and risk factors related to UGIB. The Cox proportional hazards model was applied to evaluate the risk factors of UGIB. A subgroup analysis was performed to evaluate the trends pre- and post-COVID. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Results: Among the 116,287 patients with AMI, 1,310 developed UGIB within 30 days (1.13%). After matching, 1,300 patients were included in each group. The overall incidence of UGIB was 5.75%, which was higher post-COVID (3.97%) and pre-COVID (2.43%). The incidence increased with age, peaking at 7.89% in patients aged ≥ 85 years (Table 1). Independent risk factors included hemoglobin < 10 g/dL, BUN ≥ 40 mg/dL, heart failure, chronic kidney disease, diabetes, steroid use, and blood transfusion (Table 3). Aspirin (HR 0.78) and ticagrelor (HR, 0.63) were associated with a lower risk of UGIB. The UGIB risk was higher in the post-COVID period (HR 2.19) than in the pre-COVID period (HR 2.03).
Discussion: The incidence of UGIB following AMI increased in older adults and in those with anemia, renal dysfunction, or cardiovascular comorbidities. Risk increased significantly after the COVID-19 pandemic. Early recognition and risk mitigation, including cautious use of anticoagulants and appropriate gastroprotection, may reduce the post-AMI UGIB burden.
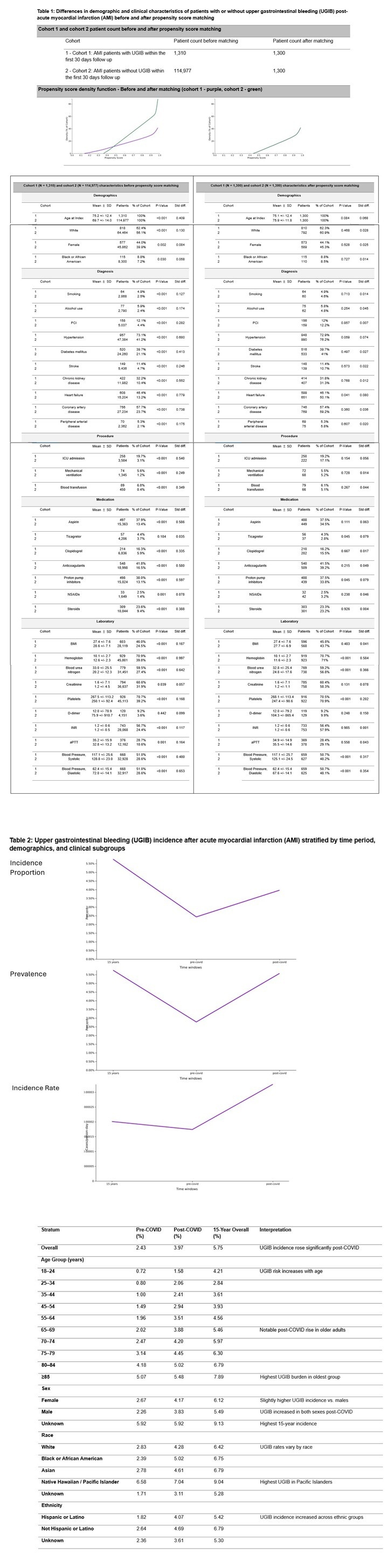
Figure: Table 1: Differences in demographic and clinical characteristics of patients with or without upper gastrointestinal bleeding (UGIB) post-acute myocardial infarction (AMI) before and after propensity score matching
Table 2: Upper gastrointestinal bleeding (UGIB) incidence after acute myocardial infarction (AMI) stratified by time period, demographics, and clinical subgroups
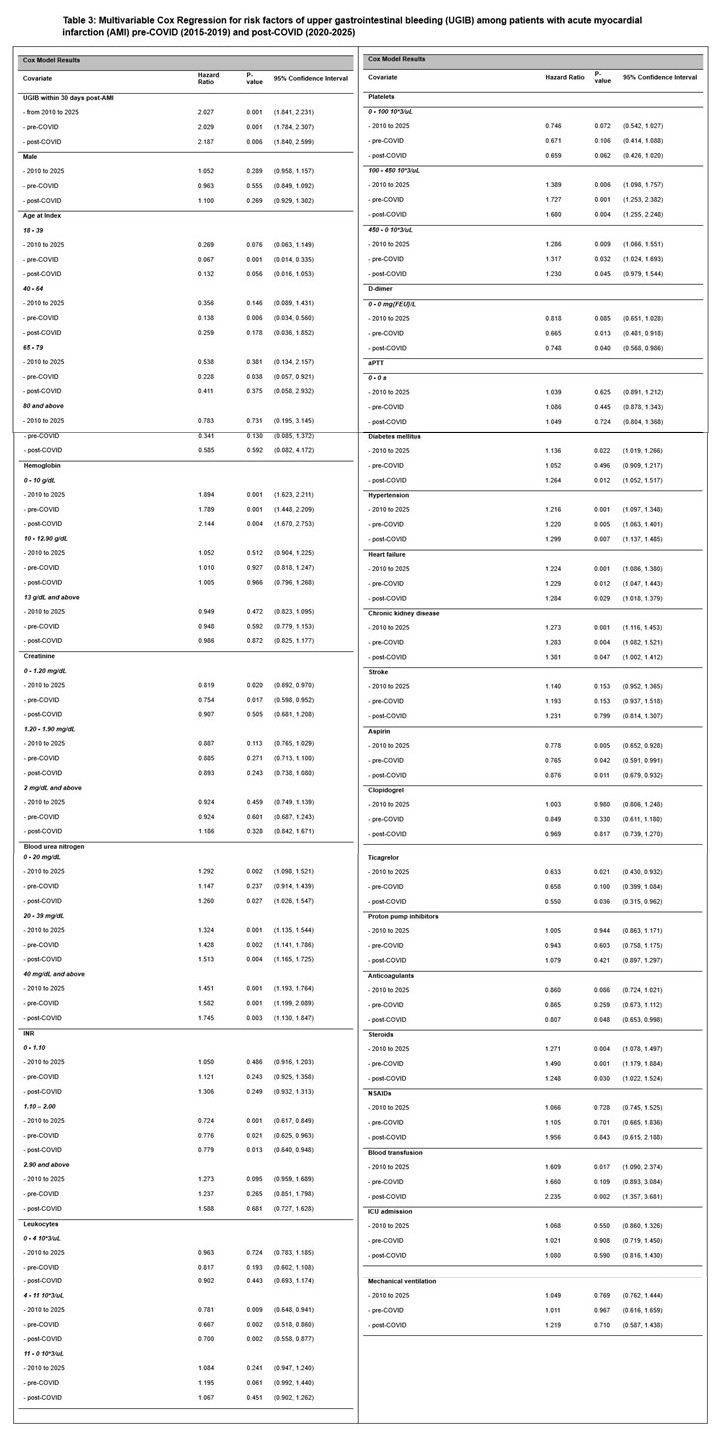
Figure: Table 3: Multivariable Cox Regression for risk factors of upper gastrointestinal bleeding (UGIB) among patients with acute myocardial infarction (AMI) pre-COVID (2015-2019) and post-COVID (2020-2025)
Disclosures:
Thai Hau Koo indicated no relevant financial relationships.
Yilin Song indicated no relevant financial relationships.
Stephen Firkins indicated no relevant financial relationships.
Roberto Simons-Linares indicated no relevant financial relationships.
Thai Hau Koo, MD1, Yilin Song, MD2, Stephen Firkins, MD3, Roberto Simons-Linares, MD3. P3055 - Upper Gastrointestinal Bleeding After Acute Myocardial Infarction: Incidence, Predictors, and COVID-Era Comparison, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 2University of Maryland Medical Center, Baltimore, MD; 3Gastroenterology and Hepatology, Cleveland Clinic, Cleveland, OH
Introduction: Upper gastrointestinal bleeding (UGIB) is one of the complications of acute myocardial infarction (AMI) associated with poor outcomes. We aimed to evaluate the incidence and risk factors of UGIB within the first 30-day following AMI across the US nation for the past 15 years since FDA approval of direct oral anticoagulants (DOAC) in October 2010, and a subgroup of pre- and post-COVID era.
Methods: This retrospective cohort study analyzed data from the TriNetX database, encompassing over 275 million de-identified patient records. All inpatients from the US aged ≥ 18 years diagnosed with AMI were identified between October 2010 and May 2025. We defined UGIB events as all clinical and endoscopic diagnoses of UGIB occurring within a 30-day follow-up period after the AMI hospitalization. Patients with UGIB diagnosis that occurred before or during the AMI hospitalization were excluded. Patients who went through AMI without developing UGIB were classified into the control group. Propensity score matching was applied based on demographics and risk factors related to UGIB. The Cox proportional hazards model was applied to evaluate the risk factors of UGIB. A subgroup analysis was performed to evaluate the trends pre- and post-COVID. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Results: Among the 116,287 patients with AMI, 1,310 developed UGIB within 30 days (1.13%). After matching, 1,300 patients were included in each group. The overall incidence of UGIB was 5.75%, which was higher post-COVID (3.97%) and pre-COVID (2.43%). The incidence increased with age, peaking at 7.89% in patients aged ≥ 85 years (Table 1). Independent risk factors included hemoglobin < 10 g/dL, BUN ≥ 40 mg/dL, heart failure, chronic kidney disease, diabetes, steroid use, and blood transfusion (Table 3). Aspirin (HR 0.78) and ticagrelor (HR, 0.63) were associated with a lower risk of UGIB. The UGIB risk was higher in the post-COVID period (HR 2.19) than in the pre-COVID period (HR 2.03).
Discussion: The incidence of UGIB following AMI increased in older adults and in those with anemia, renal dysfunction, or cardiovascular comorbidities. Risk increased significantly after the COVID-19 pandemic. Early recognition and risk mitigation, including cautious use of anticoagulants and appropriate gastroprotection, may reduce the post-AMI UGIB burden.
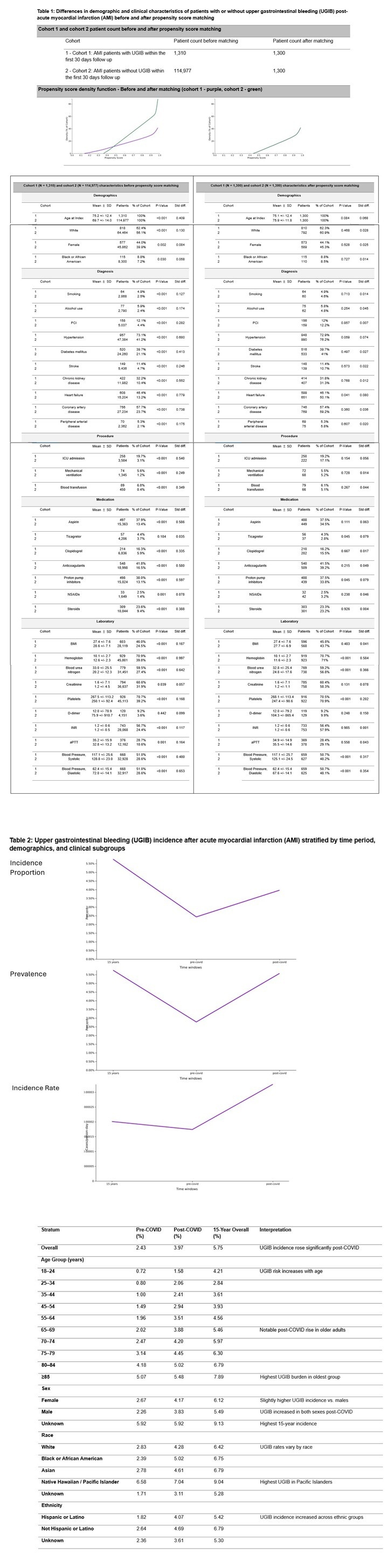
Figure: Table 1: Differences in demographic and clinical characteristics of patients with or without upper gastrointestinal bleeding (UGIB) post-acute myocardial infarction (AMI) before and after propensity score matching
Table 2: Upper gastrointestinal bleeding (UGIB) incidence after acute myocardial infarction (AMI) stratified by time period, demographics, and clinical subgroups
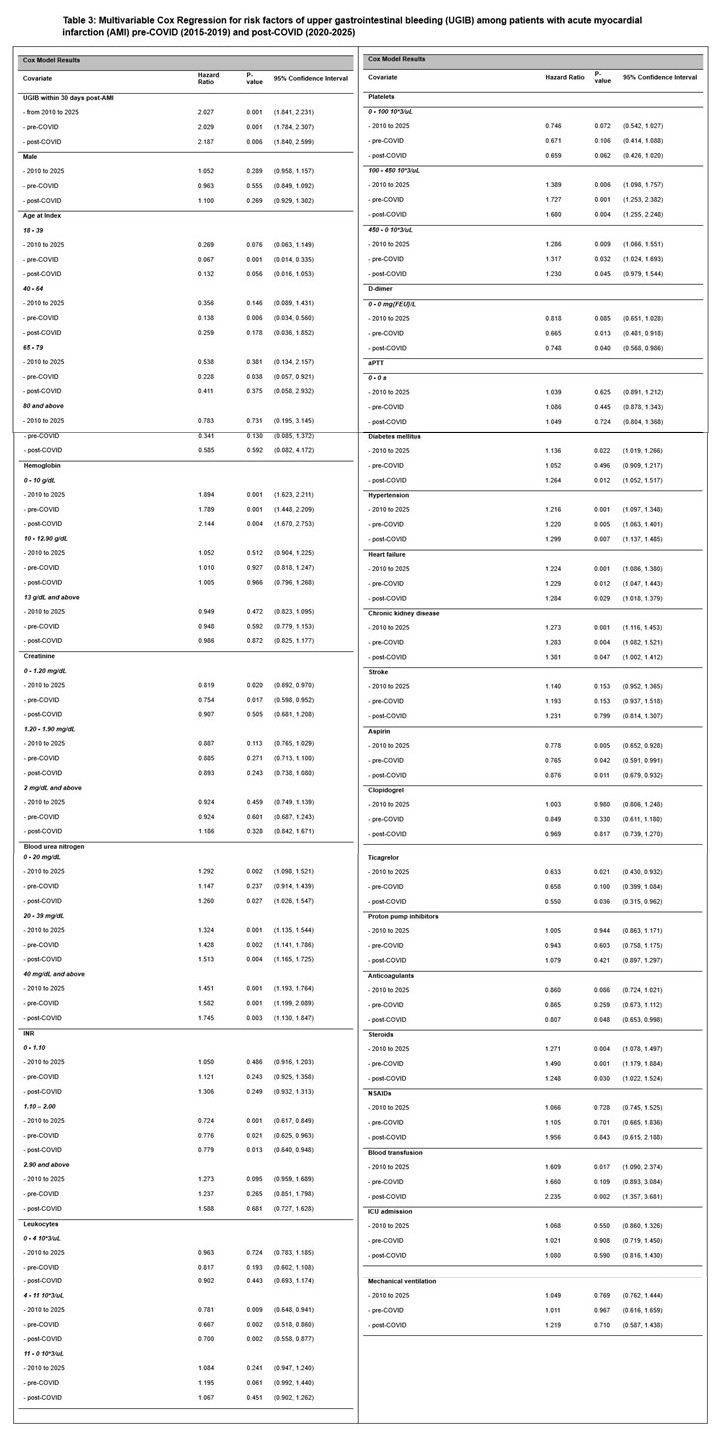
Figure: Table 3: Multivariable Cox Regression for risk factors of upper gastrointestinal bleeding (UGIB) among patients with acute myocardial infarction (AMI) pre-COVID (2015-2019) and post-COVID (2020-2025)
Disclosures:
Thai Hau Koo indicated no relevant financial relationships.
Yilin Song indicated no relevant financial relationships.
Stephen Firkins indicated no relevant financial relationships.
Roberto Simons-Linares indicated no relevant financial relationships.
Thai Hau Koo, MD1, Yilin Song, MD2, Stephen Firkins, MD3, Roberto Simons-Linares, MD3. P3055 - Upper Gastrointestinal Bleeding After Acute Myocardial Infarction: Incidence, Predictors, and COVID-Era Comparison, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
