Monday Poster Session
Category: GI Bleeding
P3053 - Bleeding Differently: Variceal vs Non-Variceal GI Bleeds in Sarcoidosis – Who Fares Better?
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Aashay Dharia, MD
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Chaula Desai, MD, Manasa Ginjupalli, MD, Sweta Lohani, MD, Aashay Dharia, MD
Brooklyn Hospital Center, Brooklyn, NY
Introduction: Sarcoidosis is a chronic systemic inflammatory disease affecting multiple organs, including the gastrointestinal (GI) system. Luminal involvement of the GI tract is rare but potentially life-threatening. Variceal bleeding in sarcoidosis is likely due to liver involvement progressing to cirrhosis. Nonvariceal bleeding could be due to chronic non-steroidal anti-inflammatory drugs (NSAIDs) use, steroids, and vascular involvement. Data comparing variceal and non-variceal bleeding outcomes in sarcoidosis is limited. This study compares patient characteristics, clinical outcomes, and the need for interventions in sarcoidosis patients with variceal and non-variceal GI bleeds.
Methods: We queried the National Inpatient Sample (NIS) from 2016 to 2020 to identify adult hospitalizations with sarcoidosis using appropriate ICD-10 codes. They were divided into two groups based on variceal and non-variceal gastrointestinal (GI) bleeding and the chi-square test and independent sample t-test were used to compare outcomes in variceal and non-variceal bleeding. Logistic regression models were used to adjust for potential confounders. A p-value less than 0.05 was set to determine statistical significance.
Results: 384,375 adult hospitalizations with sarcoidosis were identified. Among patients with GI bleeding, 12.2% had variceal and 87.8% had non-variceal bleeding. The variceal cohort was younger (mean age 57 vs 62) and predominantly male. Hospitalizations with sarcoidosis and variceal bleeding had significantly lower odds of mortality (adjusted Odds ratio [aOR] 0.37, p-value 0.02). However, they were more likely to receive endoscopic intervention (aOR 3.98, p< 0.001). There was no significant difference in the risk of shock, acute kidney injury (AKI), need for blood transfusions, vasopressor requirement, or ventilator support.
Discussion: Our study highlights key differences in outcomes between variceal and non-variceal GI bleeding in sarcoidosis patients. Despite being younger and having lower mortality rates, the variceal group had a higher need for endoscopic intervention. Variceal bleeding has well-established protocols for management and is more amenable to interventions like variceal banding and sclerotherapy. Non-variceal bleeding can be more heterogeneous and is often due to superficial mucosal bleeding which is unsuitable for endoscopic intervention. Further studies are warranted to explore these differences and optimize the management of GI bleeding in sarcoidosis patients.
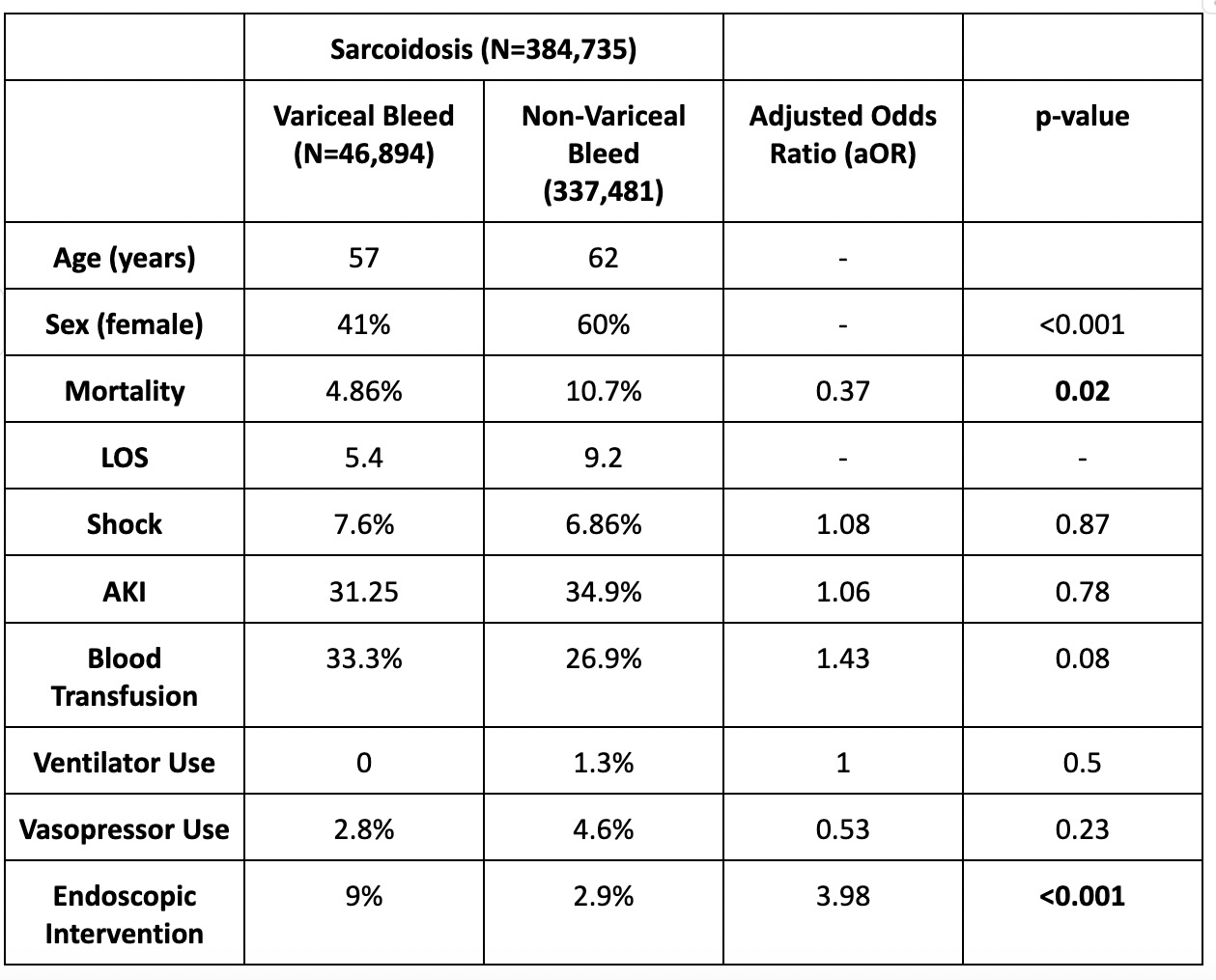
Figure: Results
Disclosures:
Chaula Desai indicated no relevant financial relationships.
Manasa Ginjupalli indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Aashay Dharia indicated no relevant financial relationships.
Chaula Desai, MD, Manasa Ginjupalli, MD, Sweta Lohani, MD, Aashay Dharia, MD. P3053 - Bleeding Differently: Variceal vs Non-Variceal GI Bleeds in Sarcoidosis – Who Fares Better?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Brooklyn Hospital Center, Brooklyn, NY
Introduction: Sarcoidosis is a chronic systemic inflammatory disease affecting multiple organs, including the gastrointestinal (GI) system. Luminal involvement of the GI tract is rare but potentially life-threatening. Variceal bleeding in sarcoidosis is likely due to liver involvement progressing to cirrhosis. Nonvariceal bleeding could be due to chronic non-steroidal anti-inflammatory drugs (NSAIDs) use, steroids, and vascular involvement. Data comparing variceal and non-variceal bleeding outcomes in sarcoidosis is limited. This study compares patient characteristics, clinical outcomes, and the need for interventions in sarcoidosis patients with variceal and non-variceal GI bleeds.
Methods: We queried the National Inpatient Sample (NIS) from 2016 to 2020 to identify adult hospitalizations with sarcoidosis using appropriate ICD-10 codes. They were divided into two groups based on variceal and non-variceal gastrointestinal (GI) bleeding and the chi-square test and independent sample t-test were used to compare outcomes in variceal and non-variceal bleeding. Logistic regression models were used to adjust for potential confounders. A p-value less than 0.05 was set to determine statistical significance.
Results: 384,375 adult hospitalizations with sarcoidosis were identified. Among patients with GI bleeding, 12.2% had variceal and 87.8% had non-variceal bleeding. The variceal cohort was younger (mean age 57 vs 62) and predominantly male. Hospitalizations with sarcoidosis and variceal bleeding had significantly lower odds of mortality (adjusted Odds ratio [aOR] 0.37, p-value 0.02). However, they were more likely to receive endoscopic intervention (aOR 3.98, p< 0.001). There was no significant difference in the risk of shock, acute kidney injury (AKI), need for blood transfusions, vasopressor requirement, or ventilator support.
Discussion: Our study highlights key differences in outcomes between variceal and non-variceal GI bleeding in sarcoidosis patients. Despite being younger and having lower mortality rates, the variceal group had a higher need for endoscopic intervention. Variceal bleeding has well-established protocols for management and is more amenable to interventions like variceal banding and sclerotherapy. Non-variceal bleeding can be more heterogeneous and is often due to superficial mucosal bleeding which is unsuitable for endoscopic intervention. Further studies are warranted to explore these differences and optimize the management of GI bleeding in sarcoidosis patients.
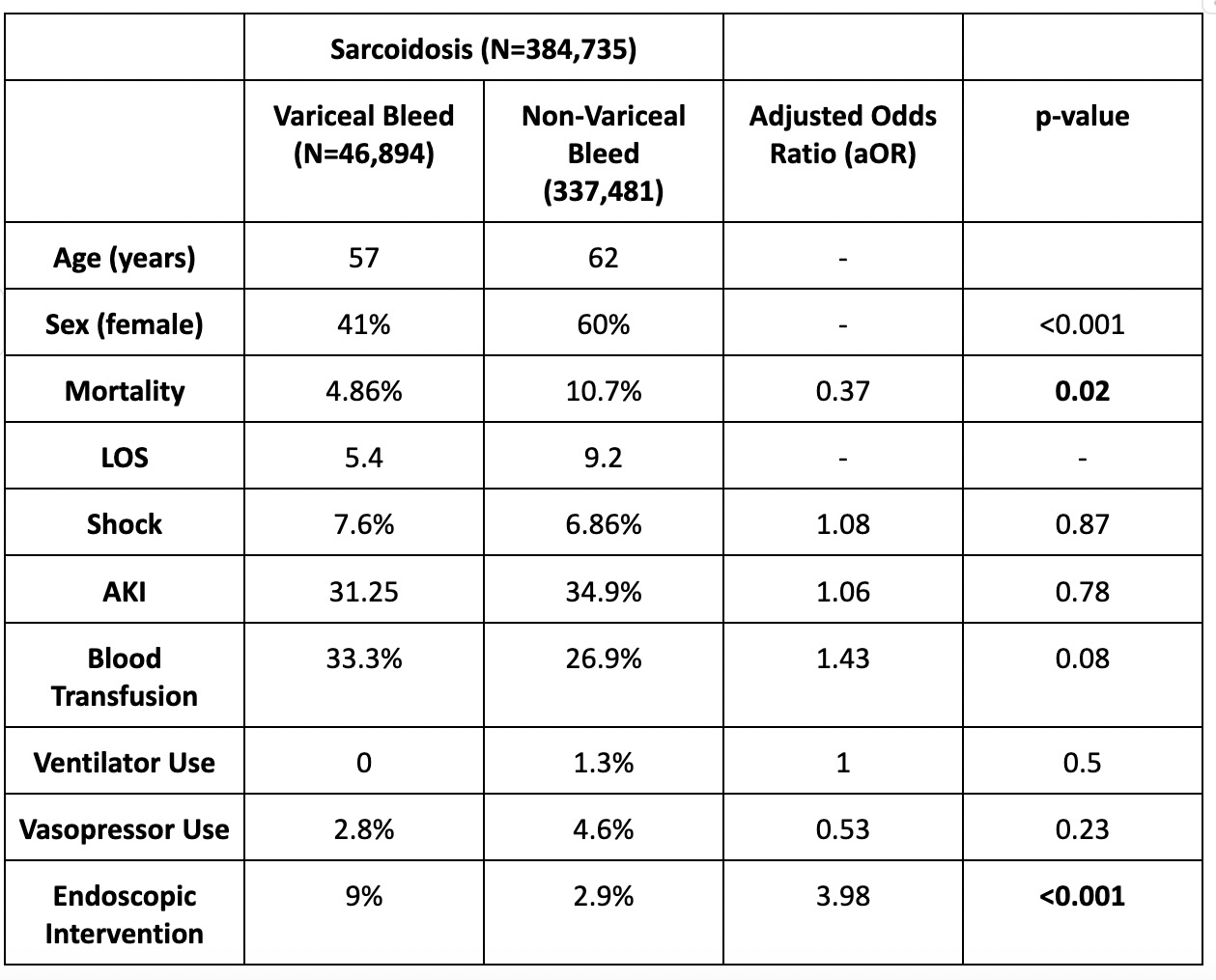
Figure: Results
Disclosures:
Chaula Desai indicated no relevant financial relationships.
Manasa Ginjupalli indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Aashay Dharia indicated no relevant financial relationships.
Chaula Desai, MD, Manasa Ginjupalli, MD, Sweta Lohani, MD, Aashay Dharia, MD. P3053 - Bleeding Differently: Variceal vs Non-Variceal GI Bleeds in Sarcoidosis – Who Fares Better?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
