Monday Poster Session
Category: GI Bleeding
P3050 - Intermittent vs Continuous Proton Pump Inhibitor Therapy for Bleeding Peptic Ulcer: An Updated Systematic Review and Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- OA
Omar Abdelhalim, MD (he/him/his)
Icahn School of Medicine at Mount Sinai
Queens, NY
Presenting Author(s)
Hazem Abosheaishaa, MD1, Abdallfatah Abdallfatah, 2, Omar Abdelhalim, MD3, Mohamed Eldesouki, MD4, Salma Allam, 5, Gomathy Nageswaran, MBBS6, Fnu Hakim, MD7, Mohamad Elgozair, MD8, Huber Padilla. Zombrano, MD9, Mahassen Akram. Elshaer, MD10, Ahmed Shady, MD11, Saphwat Eskaros, MD12, Negar Niknam, MD12
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY; 2Faculty of Medicine, October 6 University, Giza, Al Jizah, Egypt; 3Icahn School of Medicine at Mount Sinai, Queens, NY; 4Saint Michael's Medical Center, New York Medical College, Newark, NJ; 5Galala University, Suez, As Suways, Egypt; 6University of Arkansas for Medical Sciences, Little Rock, AR; 7Al Jazeerah Health Center, Emirates Health Service – Ministry of Health and Prevention, Jamaica, NY; 8Danbury / Yale New Haven Hospital, Danbury, CT; 9Advanced GI Endoscopy, EmuraCenter Latinoamerica, Bogotá, Colombia, Cartagena, Bolivar, Colombia; 10King Fahad Military Hospital, jeddah, Jeddah, Makkah, Saudi Arabia; 11University of Michigan health-Sparrow, Lansing, MI; 12Icahn school of Medicine at Mount Sinai NYC Health + Hospitals Queens, Gastroenterology Department, Queens, NY
Introduction: Gastrointestinal bleeding from peptic ulcers remains a significant clinical challenge, with high rebleeding rates even after endoscopic intervention. Proton pump inhibitors (PPIs) are commonly used to maintain hemostasis by maintaining gastric pH, but the optimal administration method—continuous infusion versus intermittent therapy—remains debated. This meta-analysis compares the efficacy of intermittent versus continuous PPI therapy in preventing rebleeding and other clinical outcomes in patients with bleeding peptic ulcers.
Methods: We systematically searched databases including Embase, Scopus, Web of Science, Medline/PubMed, and Cochrane. Primary outcomes were rebleeding rates, mortality, hospital stay duration, and ICU admissions. Quality assessment was conducted using the Newcastle-Ottawa Scale for cohort studies and the Cochrane Risk of Bias Tool (ROB2) for RCTs. Meta-analyses were performed using a random-effects model, and heterogeneity was assessed with the I² statistic.
Results: Eighteen studies (n=3664) were included, spanning multiple countries. Meta-analysis showed no significant difference between intermittent and continuous PPI therapy in terms of rebleeding rates (OR=1.02; 95% CI=0.80–1.29; P=0.88, I²=20%), mortality (OR=0.93; 95% CI=0.56–1.55; P=0.79, I²=21%), or the need for surgery (OR=1.09; 95% CI=0.71–1.70; P=0.69, I²=0%). However, intermittent therapy was associated with significantly lower ICU admissions (OR=0.29; 95% CI=0.22–0.40; P< 0.00001, I²=7%).
Discussion: Intermittent PPI therapy is as effective as continuous infusion in managing bleeding peptic ulcers, with comparable rebleeding, surgery, and mortality outcomes. Intermittent therapy also reduces ICU admission rates, suggesting a viable, cost-effective alternative to continuous infusion. Further research with larger, multi-center trials is needed to confirm these findings across diverse populations and healthcare settings.
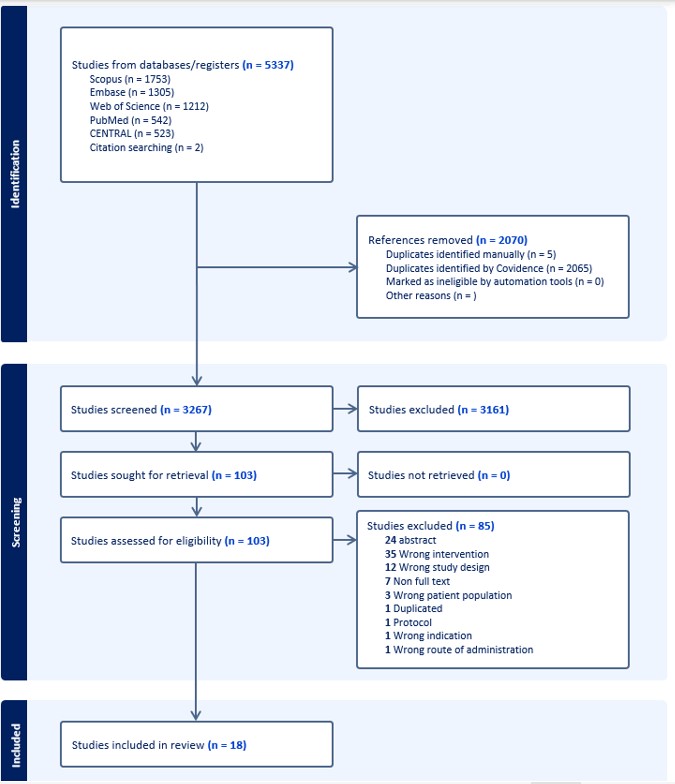
Figure: Figure 1. PRISMA flow chart showing different stages of screening and number of studies included
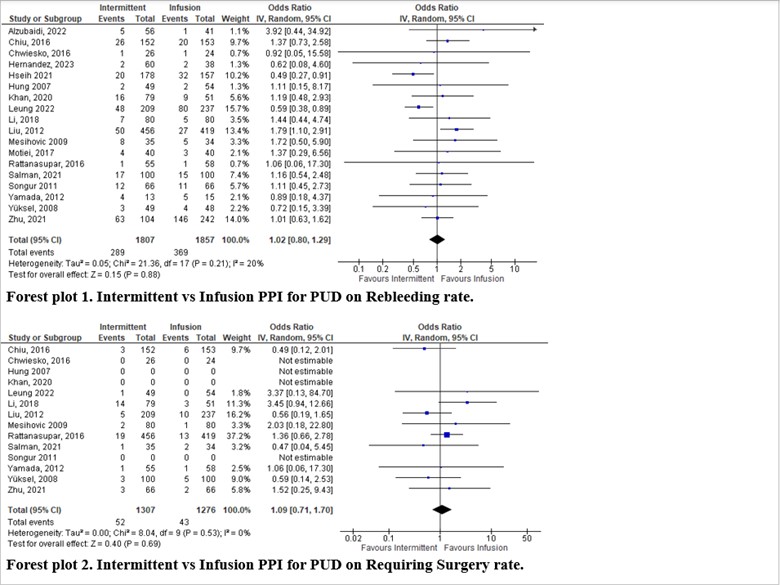
Figure: Figure 2, Forest plot 1. Intermittent vs Infusion PPI for PUD on Rebleeding rate, Forest plot 2. Intermittent vs Infusion PPI for PUD on Requiring Surgery rate.
Disclosures:
Hazem Abosheaishaa indicated no relevant financial relationships.
Abdallfatah Abdallfatah indicated no relevant financial relationships.
Omar Abdelhalim indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Salma Allam indicated no relevant financial relationships.
Gomathy Nageswaran indicated no relevant financial relationships.
Fnu Hakim indicated no relevant financial relationships.
Mohamad Elgozair indicated no relevant financial relationships.
Huber Zombrano indicated no relevant financial relationships.
Mahassen Elshaer indicated no relevant financial relationships.
Ahmed Shady indicated no relevant financial relationships.
Saphwat Eskaros indicated no relevant financial relationships.
Negar Niknam indicated no relevant financial relationships.
Hazem Abosheaishaa, MD1, Abdallfatah Abdallfatah, 2, Omar Abdelhalim, MD3, Mohamed Eldesouki, MD4, Salma Allam, 5, Gomathy Nageswaran, MBBS6, Fnu Hakim, MD7, Mohamad Elgozair, MD8, Huber Padilla. Zombrano, MD9, Mahassen Akram. Elshaer, MD10, Ahmed Shady, MD11, Saphwat Eskaros, MD12, Negar Niknam, MD12. P3050 - Intermittent vs Continuous Proton Pump Inhibitor Therapy for Bleeding Peptic Ulcer: An Updated Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY; 2Faculty of Medicine, October 6 University, Giza, Al Jizah, Egypt; 3Icahn School of Medicine at Mount Sinai, Queens, NY; 4Saint Michael's Medical Center, New York Medical College, Newark, NJ; 5Galala University, Suez, As Suways, Egypt; 6University of Arkansas for Medical Sciences, Little Rock, AR; 7Al Jazeerah Health Center, Emirates Health Service – Ministry of Health and Prevention, Jamaica, NY; 8Danbury / Yale New Haven Hospital, Danbury, CT; 9Advanced GI Endoscopy, EmuraCenter Latinoamerica, Bogotá, Colombia, Cartagena, Bolivar, Colombia; 10King Fahad Military Hospital, jeddah, Jeddah, Makkah, Saudi Arabia; 11University of Michigan health-Sparrow, Lansing, MI; 12Icahn school of Medicine at Mount Sinai NYC Health + Hospitals Queens, Gastroenterology Department, Queens, NY
Introduction: Gastrointestinal bleeding from peptic ulcers remains a significant clinical challenge, with high rebleeding rates even after endoscopic intervention. Proton pump inhibitors (PPIs) are commonly used to maintain hemostasis by maintaining gastric pH, but the optimal administration method—continuous infusion versus intermittent therapy—remains debated. This meta-analysis compares the efficacy of intermittent versus continuous PPI therapy in preventing rebleeding and other clinical outcomes in patients with bleeding peptic ulcers.
Methods: We systematically searched databases including Embase, Scopus, Web of Science, Medline/PubMed, and Cochrane. Primary outcomes were rebleeding rates, mortality, hospital stay duration, and ICU admissions. Quality assessment was conducted using the Newcastle-Ottawa Scale for cohort studies and the Cochrane Risk of Bias Tool (ROB2) for RCTs. Meta-analyses were performed using a random-effects model, and heterogeneity was assessed with the I² statistic.
Results: Eighteen studies (n=3664) were included, spanning multiple countries. Meta-analysis showed no significant difference between intermittent and continuous PPI therapy in terms of rebleeding rates (OR=1.02; 95% CI=0.80–1.29; P=0.88, I²=20%), mortality (OR=0.93; 95% CI=0.56–1.55; P=0.79, I²=21%), or the need for surgery (OR=1.09; 95% CI=0.71–1.70; P=0.69, I²=0%). However, intermittent therapy was associated with significantly lower ICU admissions (OR=0.29; 95% CI=0.22–0.40; P< 0.00001, I²=7%).
Discussion: Intermittent PPI therapy is as effective as continuous infusion in managing bleeding peptic ulcers, with comparable rebleeding, surgery, and mortality outcomes. Intermittent therapy also reduces ICU admission rates, suggesting a viable, cost-effective alternative to continuous infusion. Further research with larger, multi-center trials is needed to confirm these findings across diverse populations and healthcare settings.
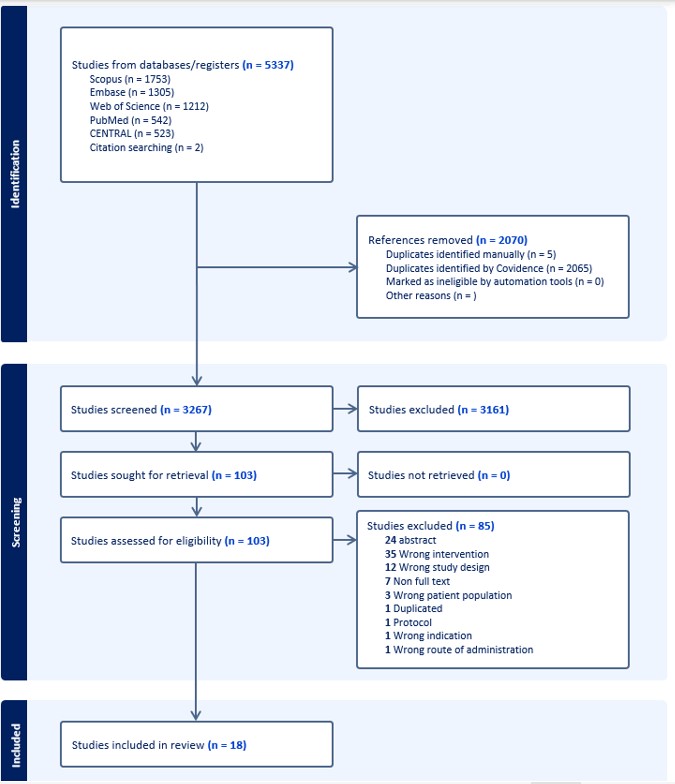
Figure: Figure 1. PRISMA flow chart showing different stages of screening and number of studies included
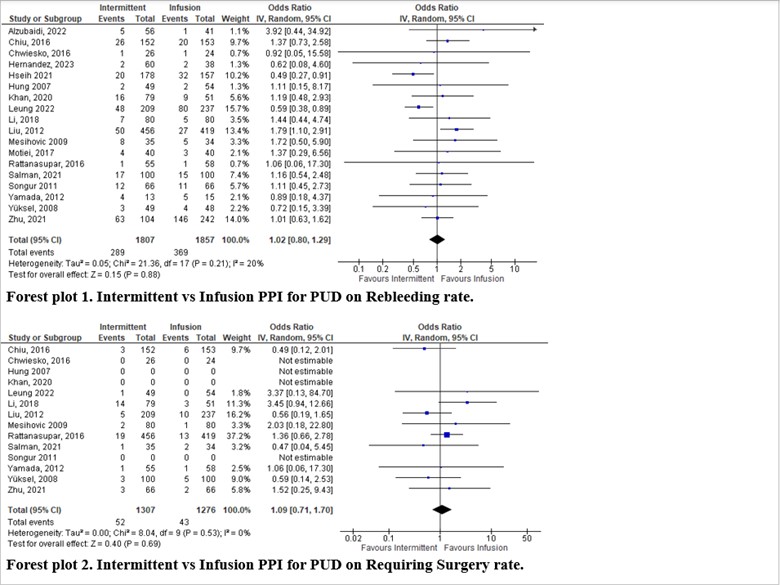
Figure: Figure 2, Forest plot 1. Intermittent vs Infusion PPI for PUD on Rebleeding rate, Forest plot 2. Intermittent vs Infusion PPI for PUD on Requiring Surgery rate.
Disclosures:
Hazem Abosheaishaa indicated no relevant financial relationships.
Abdallfatah Abdallfatah indicated no relevant financial relationships.
Omar Abdelhalim indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Salma Allam indicated no relevant financial relationships.
Gomathy Nageswaran indicated no relevant financial relationships.
Fnu Hakim indicated no relevant financial relationships.
Mohamad Elgozair indicated no relevant financial relationships.
Huber Zombrano indicated no relevant financial relationships.
Mahassen Elshaer indicated no relevant financial relationships.
Ahmed Shady indicated no relevant financial relationships.
Saphwat Eskaros indicated no relevant financial relationships.
Negar Niknam indicated no relevant financial relationships.
Hazem Abosheaishaa, MD1, Abdallfatah Abdallfatah, 2, Omar Abdelhalim, MD3, Mohamed Eldesouki, MD4, Salma Allam, 5, Gomathy Nageswaran, MBBS6, Fnu Hakim, MD7, Mohamad Elgozair, MD8, Huber Padilla. Zombrano, MD9, Mahassen Akram. Elshaer, MD10, Ahmed Shady, MD11, Saphwat Eskaros, MD12, Negar Niknam, MD12. P3050 - Intermittent vs Continuous Proton Pump Inhibitor Therapy for Bleeding Peptic Ulcer: An Updated Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
