Monday Poster Session
Category: GI Bleeding
P3156 - Hemorrhagic Shock Secondary to Buried Bumper Syndrome
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
John M. Sullivan, III, MD
Henry Ford Health Genesys Hospital
Grand Blanc, MI
Presenting Author(s)
Brandon Wiggins, DO, MPH, John M. Sullivan, MD, Mark Rigby, DO, Nathan Landesman, DO
Henry Ford Health Genesys Hospital, Grand Blanc, MI
Introduction: Buried bumper syndrome (BBS) occurs as a result of exaggerated tensile forces on the intervening tissue between the gastric wall and the superficial dermal layers that results in migration of the gastrostomy tube through the tract. The incidence rate of BBS is considered rare. Here we would like to present a case of a patient who presented with hemorrhagic shock secondary to BBS following percutaneous endoscopic gastrostomy (PEG) placement. As this case presentation is not only rare but provides additional data on the diagnosis and management of BBS related hemorrhagic shock that is not otherwise well described in the current literature.
Case Description/
Methods: A 54-year-old with history of cerebrovascular accident status post PEG placement and atrial fibrillation on Apixaban presented for anemia. The patient was sent to the hospital from her nursing facility due to a hemoglobin of 5.7 g/dL with unknown baseline and began having large volume melena in the emergency department. Vital signs on arrival were significant for mean arterial pressures (MAP) in the low 60’s that did not respond to fluid boluses and she was started on Norepinephrine to maintain MAP > 65. The patient received blood and was started on IV Pantoprazole twice daily and esophagogastroduodenoscopy was performed, revealing a buried PEG tube bumper with associated large, deep gastric ulcer. The PEG tube was removed to allow the site to heal and an IR guided gastrostomy tube was placed. The patient stopped bleeding and had vasopressors weaned off while holding anticoagulation and with administration of high dose proton pump inhibitor for several days and was eventually discharged in stable condition.
Discussion: This case highlights the importance of proper PEG tube management to prevent complications from arising. Additionally, a high index of suspicion for potential BBS should arise when any patient presents with decreased output/function of the PEG, erythema and pain surrounding the stoma site. Further consideration to risk stratify patients based on their preexisting risk factors may be of benefit to modify the maintenance and follow-up schedules for such patients to prevent BBS from occurring. Early intervention such as a risk stratifying tool and formal education of medical practitioners and caretakers would aid in preventing mortality associated with BBS related hemorrhagic shock. Lastly, a multidisciplinary approach is of greatest benefit to expedite evaluation and management.
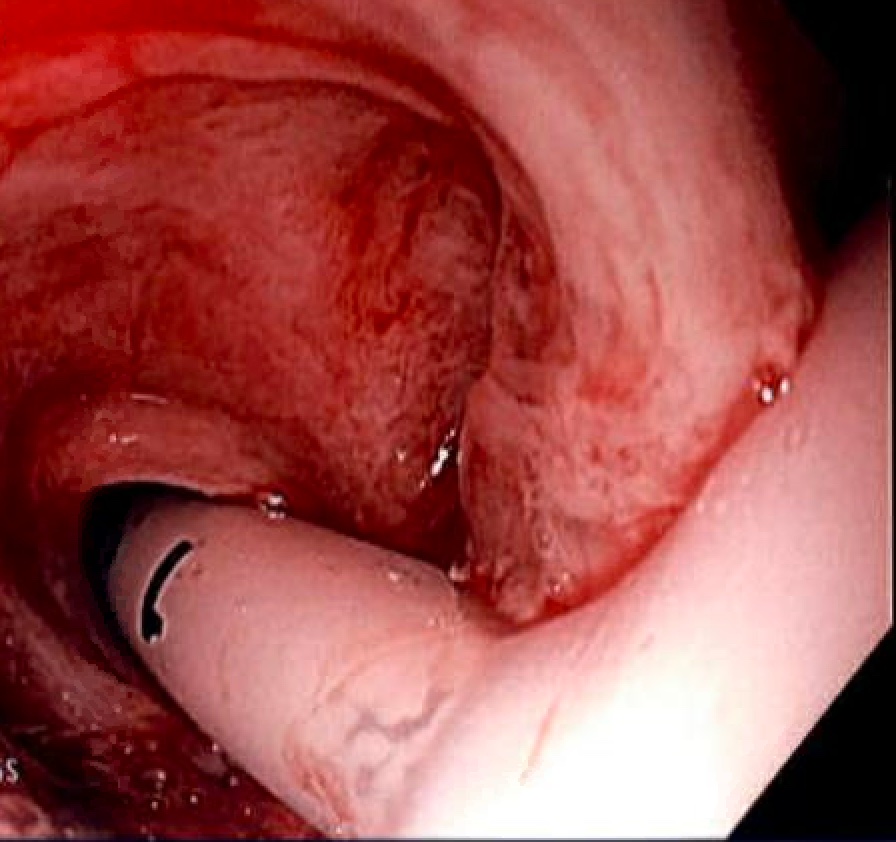
Figure: Endoscopic view of gastrostomy tube in place with suspected buried bumper syndrome related hemorrhage.
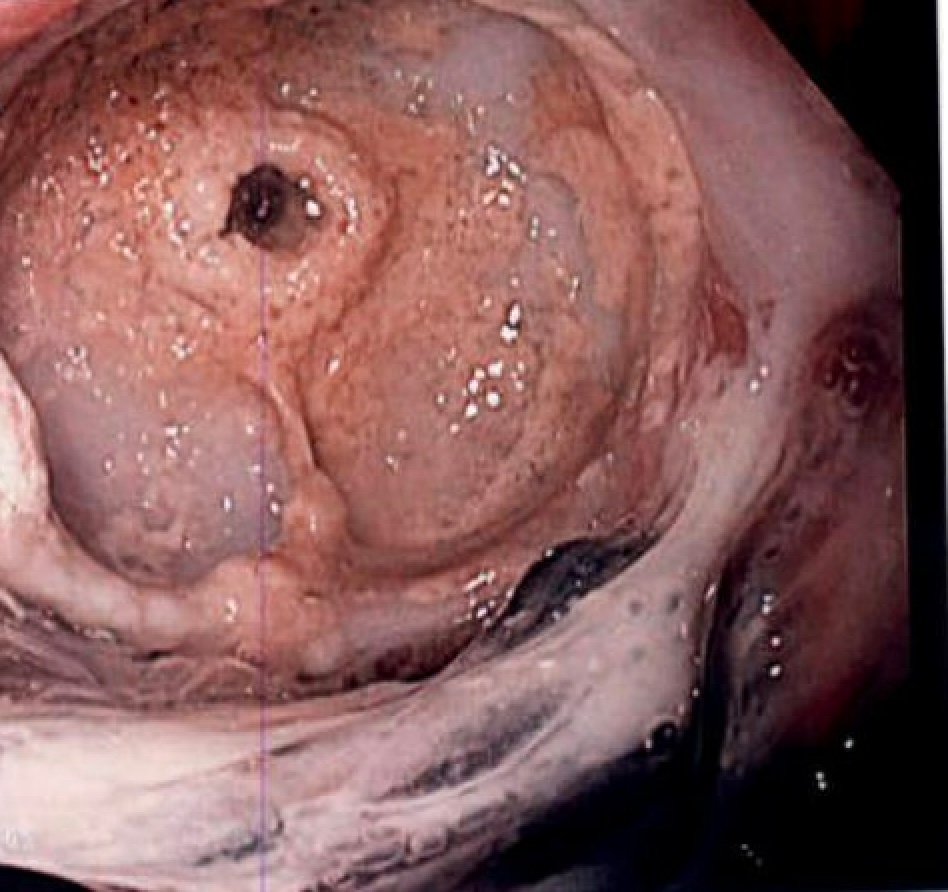
Figure: Endoscopic view of suspected buried bumper syndrome following gastrostomy tube removal and hemostasis achieved.
Disclosures:
Brandon Wiggins indicated no relevant financial relationships.
John Sullivan indicated no relevant financial relationships.
Mark Rigby indicated no relevant financial relationships.
Nathan Landesman indicated no relevant financial relationships.
Brandon Wiggins, DO, MPH, John M. Sullivan, MD, Mark Rigby, DO, Nathan Landesman, DO. P3156 - Hemorrhagic Shock Secondary to Buried Bumper Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Henry Ford Health Genesys Hospital, Grand Blanc, MI
Introduction: Buried bumper syndrome (BBS) occurs as a result of exaggerated tensile forces on the intervening tissue between the gastric wall and the superficial dermal layers that results in migration of the gastrostomy tube through the tract. The incidence rate of BBS is considered rare. Here we would like to present a case of a patient who presented with hemorrhagic shock secondary to BBS following percutaneous endoscopic gastrostomy (PEG) placement. As this case presentation is not only rare but provides additional data on the diagnosis and management of BBS related hemorrhagic shock that is not otherwise well described in the current literature.
Case Description/
Methods: A 54-year-old with history of cerebrovascular accident status post PEG placement and atrial fibrillation on Apixaban presented for anemia. The patient was sent to the hospital from her nursing facility due to a hemoglobin of 5.7 g/dL with unknown baseline and began having large volume melena in the emergency department. Vital signs on arrival were significant for mean arterial pressures (MAP) in the low 60’s that did not respond to fluid boluses and she was started on Norepinephrine to maintain MAP > 65. The patient received blood and was started on IV Pantoprazole twice daily and esophagogastroduodenoscopy was performed, revealing a buried PEG tube bumper with associated large, deep gastric ulcer. The PEG tube was removed to allow the site to heal and an IR guided gastrostomy tube was placed. The patient stopped bleeding and had vasopressors weaned off while holding anticoagulation and with administration of high dose proton pump inhibitor for several days and was eventually discharged in stable condition.
Discussion: This case highlights the importance of proper PEG tube management to prevent complications from arising. Additionally, a high index of suspicion for potential BBS should arise when any patient presents with decreased output/function of the PEG, erythema and pain surrounding the stoma site. Further consideration to risk stratify patients based on their preexisting risk factors may be of benefit to modify the maintenance and follow-up schedules for such patients to prevent BBS from occurring. Early intervention such as a risk stratifying tool and formal education of medical practitioners and caretakers would aid in preventing mortality associated with BBS related hemorrhagic shock. Lastly, a multidisciplinary approach is of greatest benefit to expedite evaluation and management.
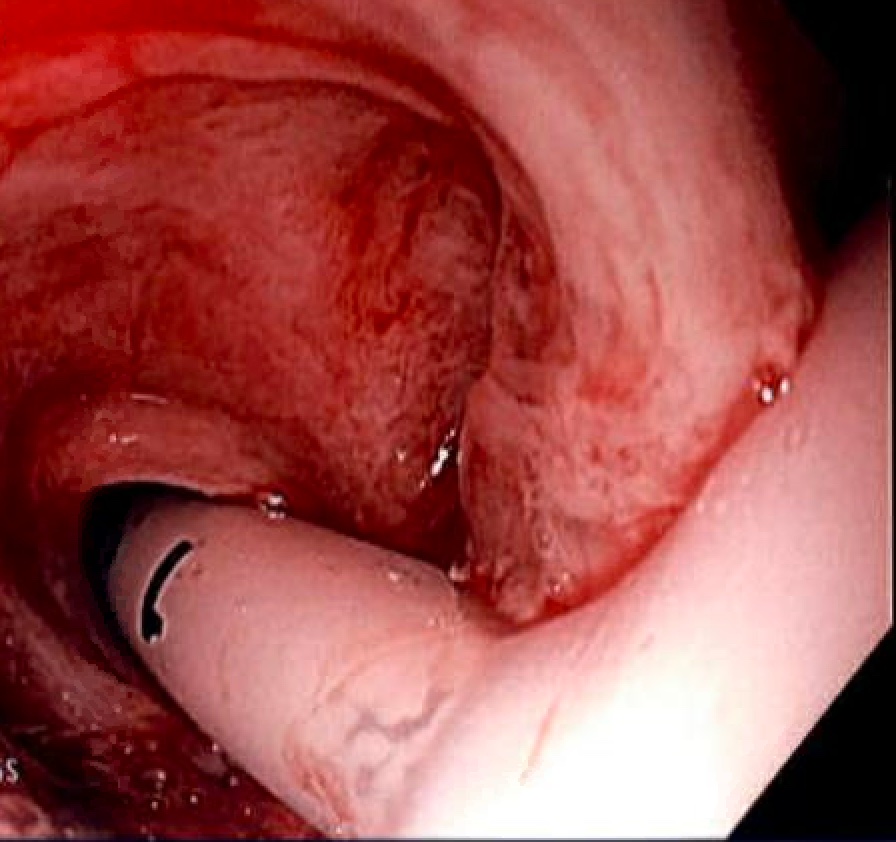
Figure: Endoscopic view of gastrostomy tube in place with suspected buried bumper syndrome related hemorrhage.
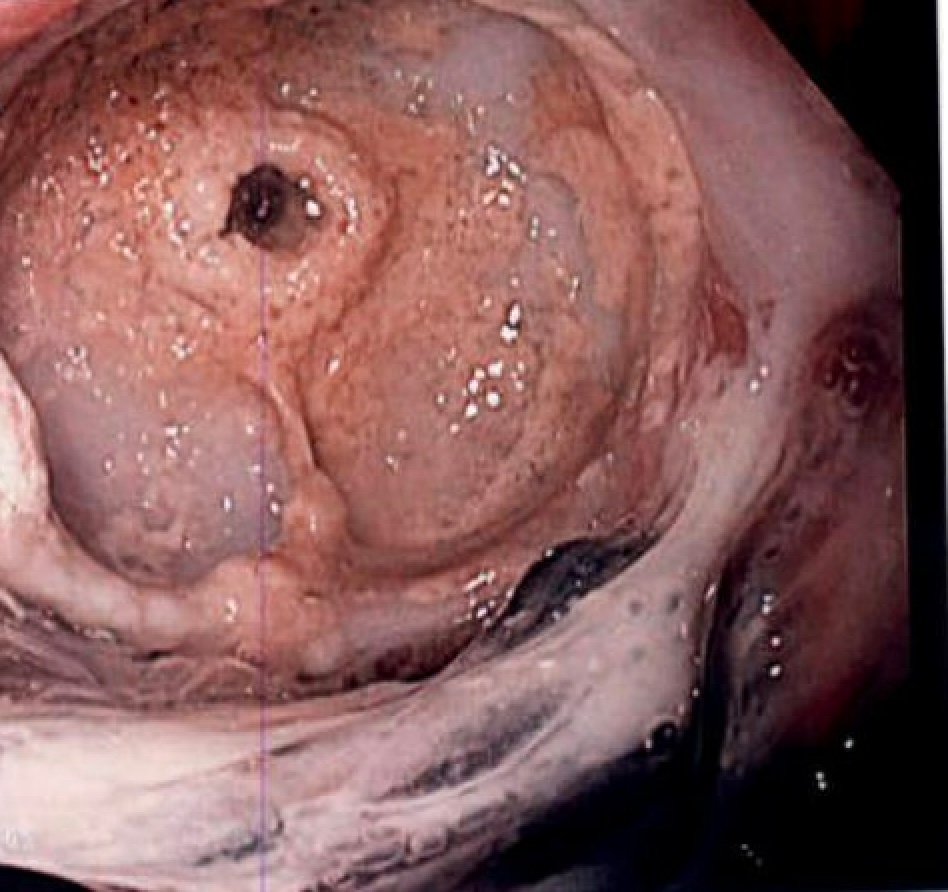
Figure: Endoscopic view of suspected buried bumper syndrome following gastrostomy tube removal and hemostasis achieved.
Disclosures:
Brandon Wiggins indicated no relevant financial relationships.
John Sullivan indicated no relevant financial relationships.
Mark Rigby indicated no relevant financial relationships.
Nathan Landesman indicated no relevant financial relationships.
Brandon Wiggins, DO, MPH, John M. Sullivan, MD, Mark Rigby, DO, Nathan Landesman, DO. P3156 - Hemorrhagic Shock Secondary to Buried Bumper Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
