Monday Poster Session
Category: GI Bleeding
Severe Iron Deficiency Anemia Due to a <i>Strongyloides</i>-Induced Duodenal Ulcer in the Setting of Warfarin Therapy
P3152 - Severe Iron Deficiency Anemia Due to a Strongyloides-Induced Duodenal Ulcer in the Setting of Warfarin Therapy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sevag Hamamah, DO
Scripps Mercy Hospital
San Diego, CA
Presenting Author(s)
Sevag Hamamah, DO, Nupur Savalia, MD, Faizi Hai, MD
Scripps Mercy Hospital, San Diego, CA
Introduction: Strongyloidiasis, caused by the parasitic nematode Strongyloides stercoralis, is endemic to tropical and subtropical regions including Southeast Asia, Africa, and Latin America. Infection occurs when filariform larvae penetrate the skin. Inside the host, female parasites reproduce through parthenogenesis, with larvae excreted through feces. Autoinfection can also occur when rhabditiform larvae develop within the gastrointestinal (GI) tract, allowing the parasite to reside for years. In immunocompromised individuals, this may lead to hyperinfection syndrome and disseminated strongyloidiasis, which can be life-threatening. However, the infection is typically asymptomatic in immunocompetent hosts and severe iron deficiency anemia requiring multiple transfusions is an uncommon presentation.
Case Description/
Methods: A 74-year-old immunocompetent man born in Latin America, with a history of paroxysmal atrial fibrillation on warfarin, presented with severe acute-on-chronic anemia. Hemoglobin on admission was 4.5 g/dL with a mean corpuscular volume of 69 fL, decreased from a baseline of 11.3 g/dL recorded one year earlier. Laboratory evaluation revealed iron deficiency with serum iron 14 µg/dL, ferritin 6.2 ng/mL, iron saturation 4%, and total iron-binding capacity 333 µg/dL. Reticulocyte count was elevated to 3%, with an immature reticulocyte fraction of 30%, indicating appropriate bone marrow response to the anemia. Further hemolytic work-up was negative. EGD revealed a superficial duodenal ulcer with an erythematous base, which biopsy confirmed as acute duodenitis due to Strongyloides stercoralis infection. Colonoscopy was unremarkable. Eosinophilia and a positive serum Strongyloides Immunoglobulin G antibody were supportive of the diagnosis. The patient received six units of packed red blood cells, three doses of intravenous iron, and a two-day weight-based course of ivermectin. Warfarin was switched to apixaban due to its lower risk of exacerbating GI bleeding. He was discharged on pantoprazole with stabilization of the anemia during follow-up.
Discussion: This case highlights the importance of considering Strongyloides stercoralis infection in unexplained iron deficiency anemia and eosinophilia, particularly when evaluating individuals from endemic regions. It also underlines key interactions between the use of anticoagulation and GI bleeding. Overall, timely diagnosis and treatment with ivermectin helped achieve resolution of the anemia and prevented further complications.

Figure: Figure 1. Strongyloides-induced small superficial ulcer with an erythematous base seen at the duodenal bulb.
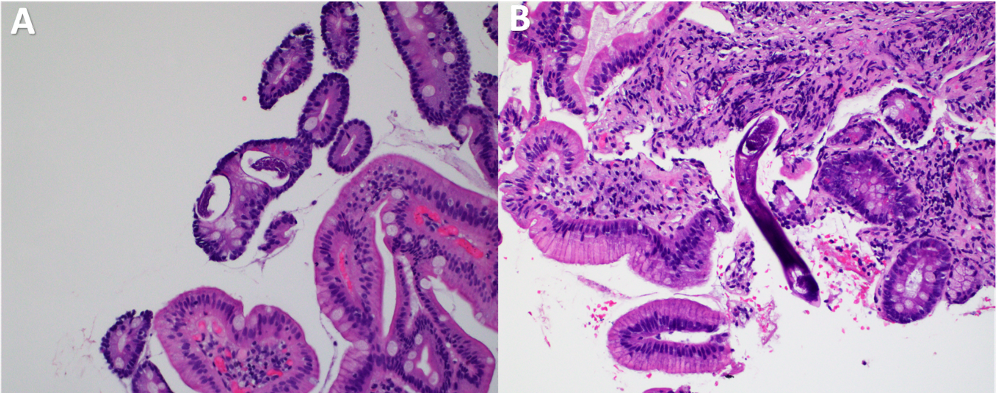
Figure: Figure 2. Histopathology from the duodenal ulcer biopsy. A) High-power Hematoxylin and Eosin (H&E)-stain of duodenal mucosa showing a cross-section of Strongyloides larvae within the crypt epithelium and lamina propria. B) Longitudinal section with filariform larvae seen within the inflamed lamina propria. Villous blunting and mucosal inflammation are present throughout both images.
Disclosures:
Sevag Hamamah indicated no relevant financial relationships.
Nupur Savalia indicated no relevant financial relationships.
Faizi Hai indicated no relevant financial relationships.
Sevag Hamamah, DO, Nupur Savalia, MD, Faizi Hai, MD. P3152 - Severe Iron Deficiency Anemia Due to a <i>Strongyloides</i>-Induced Duodenal Ulcer in the Setting of Warfarin Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Scripps Mercy Hospital, San Diego, CA
Introduction: Strongyloidiasis, caused by the parasitic nematode Strongyloides stercoralis, is endemic to tropical and subtropical regions including Southeast Asia, Africa, and Latin America. Infection occurs when filariform larvae penetrate the skin. Inside the host, female parasites reproduce through parthenogenesis, with larvae excreted through feces. Autoinfection can also occur when rhabditiform larvae develop within the gastrointestinal (GI) tract, allowing the parasite to reside for years. In immunocompromised individuals, this may lead to hyperinfection syndrome and disseminated strongyloidiasis, which can be life-threatening. However, the infection is typically asymptomatic in immunocompetent hosts and severe iron deficiency anemia requiring multiple transfusions is an uncommon presentation.
Case Description/
Methods: A 74-year-old immunocompetent man born in Latin America, with a history of paroxysmal atrial fibrillation on warfarin, presented with severe acute-on-chronic anemia. Hemoglobin on admission was 4.5 g/dL with a mean corpuscular volume of 69 fL, decreased from a baseline of 11.3 g/dL recorded one year earlier. Laboratory evaluation revealed iron deficiency with serum iron 14 µg/dL, ferritin 6.2 ng/mL, iron saturation 4%, and total iron-binding capacity 333 µg/dL. Reticulocyte count was elevated to 3%, with an immature reticulocyte fraction of 30%, indicating appropriate bone marrow response to the anemia. Further hemolytic work-up was negative. EGD revealed a superficial duodenal ulcer with an erythematous base, which biopsy confirmed as acute duodenitis due to Strongyloides stercoralis infection. Colonoscopy was unremarkable. Eosinophilia and a positive serum Strongyloides Immunoglobulin G antibody were supportive of the diagnosis. The patient received six units of packed red blood cells, three doses of intravenous iron, and a two-day weight-based course of ivermectin. Warfarin was switched to apixaban due to its lower risk of exacerbating GI bleeding. He was discharged on pantoprazole with stabilization of the anemia during follow-up.
Discussion: This case highlights the importance of considering Strongyloides stercoralis infection in unexplained iron deficiency anemia and eosinophilia, particularly when evaluating individuals from endemic regions. It also underlines key interactions between the use of anticoagulation and GI bleeding. Overall, timely diagnosis and treatment with ivermectin helped achieve resolution of the anemia and prevented further complications.

Figure: Figure 1. Strongyloides-induced small superficial ulcer with an erythematous base seen at the duodenal bulb.
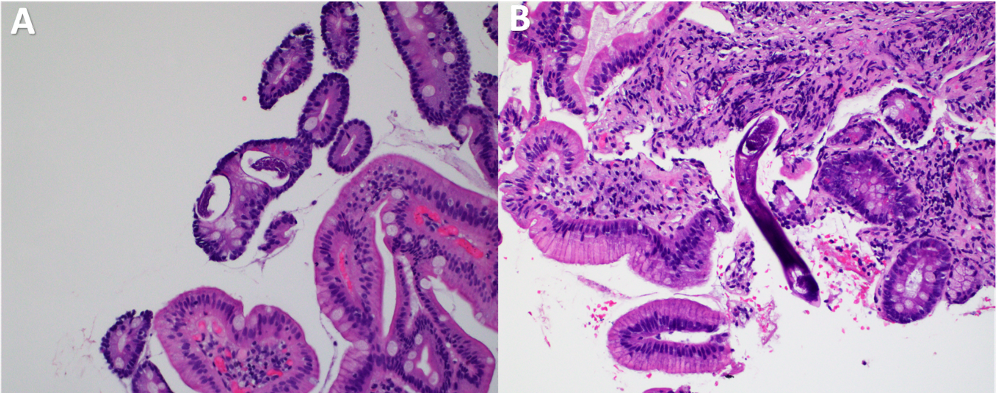
Figure: Figure 2. Histopathology from the duodenal ulcer biopsy. A) High-power Hematoxylin and Eosin (H&E)-stain of duodenal mucosa showing a cross-section of Strongyloides larvae within the crypt epithelium and lamina propria. B) Longitudinal section with filariform larvae seen within the inflamed lamina propria. Villous blunting and mucosal inflammation are present throughout both images.
Disclosures:
Sevag Hamamah indicated no relevant financial relationships.
Nupur Savalia indicated no relevant financial relationships.
Faizi Hai indicated no relevant financial relationships.
Sevag Hamamah, DO, Nupur Savalia, MD, Faizi Hai, MD. P3152 - Severe Iron Deficiency Anemia Due to a <i>Strongyloides</i>-Induced Duodenal Ulcer in the Setting of Warfarin Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
