Monday Poster Session
Category: GI Bleeding
P3146 - A Case of Recurrent Duodenal Varices
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Makul Sharma, MS (he/him/his)
Wright State University Boonshoft School of Medicine
Fairborn, OH
Presenting Author(s)
Makul Sharma, MS1, Urmimala Chaudhuri, DO2, Hassan Zreik, MD3, Mauricio Carballo, MD4
1Wright State University Boonshoft School of Medicine, Fairborn, OH; 2Wright State University, Centerville, OH; 3Wright State University Boonshoft School of Medicine, Dayton, OH; 4Dayton Gastroenterology, Beavercreek, OH
Introduction: Ectopic varices such as duodenal varices (DV) are characterized by enlarged portosystemic collateral veins in locations outside the gastroesophageal area. DVs are capable of causing significant gastrointestinal bleeding and are associated with a high mortality rate. Treatment consists of endoscopic intervention, radiological intervention, or surgery. We present a case of recurring duodenal varices successfully managed by interventional radiology (IR)-guided sclerotherapy.
Case Description/
Methods: 76-year-old female with pancreatic cystadenoma status post pylorus preserving pancreaticoduodenectomy was found to be anemic to 7.9 g/dL (baseline Hb 12 g/dL) with melenotic bowel movements. The patient had a previous a esophagogastroduodenoscopy (EGD) which noted small esophageal varices, a large small bowel varix immediately distal to the pylorus with presence of multiple red wales which was managed by IR-guided sclerosis at that time.
The patient underwent a repeat EGD which noted small esophageal varices, multiple duodenal varices in the duodenal bulb and large duodenal varices with red wale sign noted at the anastomosis site. IR was consulted for sclerosis. The patient underwent gastroduodenal variceal embolization with surgifoam slurry and sclerotherapy. The patient’s Hb improved to 13 g/dL. Given high likelihood of recurring duodenal varices, general surgery was consulted who recommended against surgical intervention and recommended repeat IR intervention if needed.
Discussion: The patient developed duodenal varices secondary to prior whipple/total pancreatectomy due to ligation of the left gastric vein. Duodenal varices typically arise due to the development of collateral veins between either the portal vein or the superior mesenteric vein and the inferior vena cava. Duodenal varices can be more challenging to treat endoscopically due to their location in the outer layers of the duodenal wall, and if located in the ascending part of the duodenum. Current treatment modalities for bleeding duodenal varices include but are not limited to endoscopic treatments, radiological interventions, and surgical procedures. In our patient, multiple duodenal varices were noted in the duodenal bulb, which required an IR approach. Interventional radiology can be consulted in these cases; they can perform various procedures, including percutaneous trans-paraumbilical sclerotherapy. Ongoing research about the detection of duodenal varices and treatment modalities is critical to patient management.
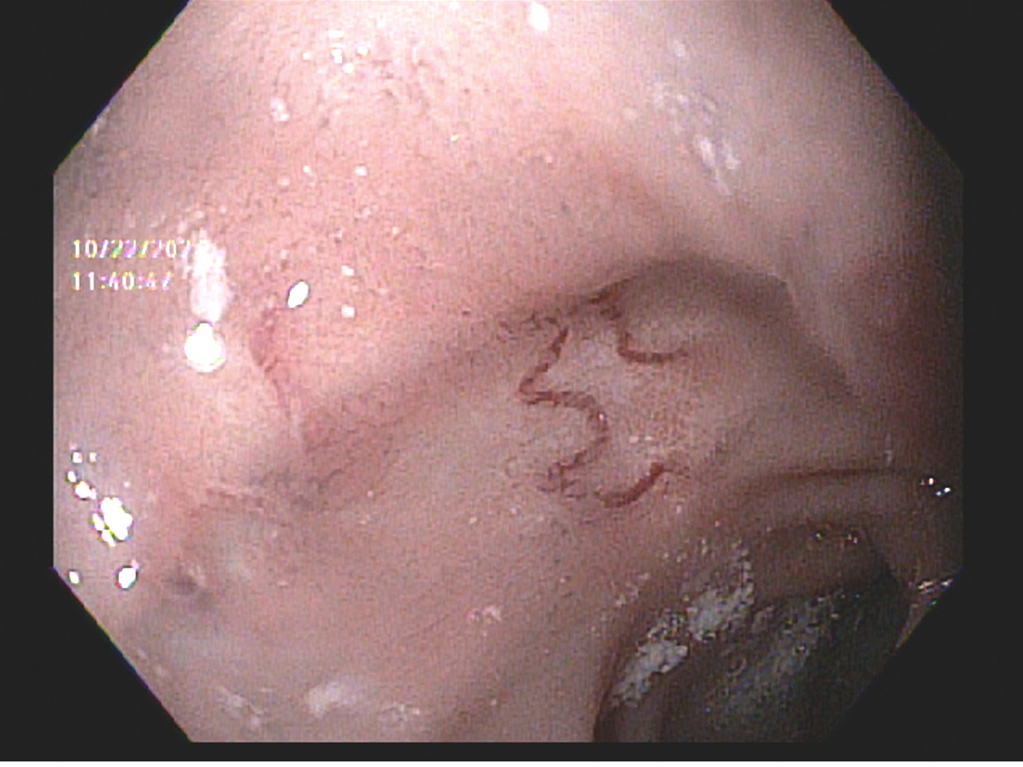
Figure: Figure 1. Linear bluish hue indicative of duodenal varices seen in the duodenal bulb, with red wale sign seen at the anastomosis site.
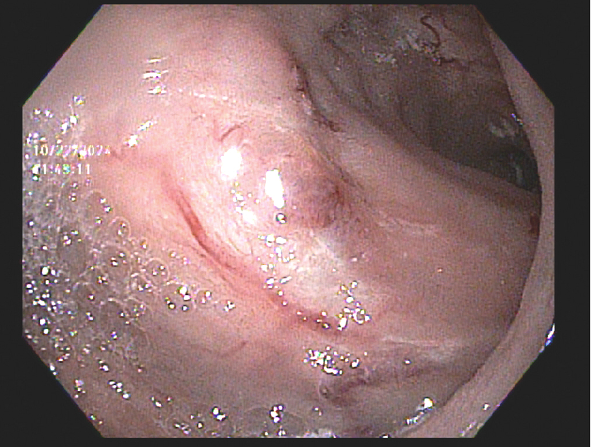
Figure: Figure 2. Linear bluish hue of duodenal varices with erythema seen in the duodenal bulb.
Disclosures:
Makul Sharma indicated no relevant financial relationships.
Urmimala Chaudhuri indicated no relevant financial relationships.
Hassan Zreik indicated no relevant financial relationships.
Mauricio Carballo indicated no relevant financial relationships.
Makul Sharma, MS1, Urmimala Chaudhuri, DO2, Hassan Zreik, MD3, Mauricio Carballo, MD4. P3146 - A Case of Recurrent Duodenal Varices, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wright State University Boonshoft School of Medicine, Fairborn, OH; 2Wright State University, Centerville, OH; 3Wright State University Boonshoft School of Medicine, Dayton, OH; 4Dayton Gastroenterology, Beavercreek, OH
Introduction: Ectopic varices such as duodenal varices (DV) are characterized by enlarged portosystemic collateral veins in locations outside the gastroesophageal area. DVs are capable of causing significant gastrointestinal bleeding and are associated with a high mortality rate. Treatment consists of endoscopic intervention, radiological intervention, or surgery. We present a case of recurring duodenal varices successfully managed by interventional radiology (IR)-guided sclerotherapy.
Case Description/
Methods: 76-year-old female with pancreatic cystadenoma status post pylorus preserving pancreaticoduodenectomy was found to be anemic to 7.9 g/dL (baseline Hb 12 g/dL) with melenotic bowel movements. The patient had a previous a esophagogastroduodenoscopy (EGD) which noted small esophageal varices, a large small bowel varix immediately distal to the pylorus with presence of multiple red wales which was managed by IR-guided sclerosis at that time.
The patient underwent a repeat EGD which noted small esophageal varices, multiple duodenal varices in the duodenal bulb and large duodenal varices with red wale sign noted at the anastomosis site. IR was consulted for sclerosis. The patient underwent gastroduodenal variceal embolization with surgifoam slurry and sclerotherapy. The patient’s Hb improved to 13 g/dL. Given high likelihood of recurring duodenal varices, general surgery was consulted who recommended against surgical intervention and recommended repeat IR intervention if needed.
Discussion: The patient developed duodenal varices secondary to prior whipple/total pancreatectomy due to ligation of the left gastric vein. Duodenal varices typically arise due to the development of collateral veins between either the portal vein or the superior mesenteric vein and the inferior vena cava. Duodenal varices can be more challenging to treat endoscopically due to their location in the outer layers of the duodenal wall, and if located in the ascending part of the duodenum. Current treatment modalities for bleeding duodenal varices include but are not limited to endoscopic treatments, radiological interventions, and surgical procedures. In our patient, multiple duodenal varices were noted in the duodenal bulb, which required an IR approach. Interventional radiology can be consulted in these cases; they can perform various procedures, including percutaneous trans-paraumbilical sclerotherapy. Ongoing research about the detection of duodenal varices and treatment modalities is critical to patient management.
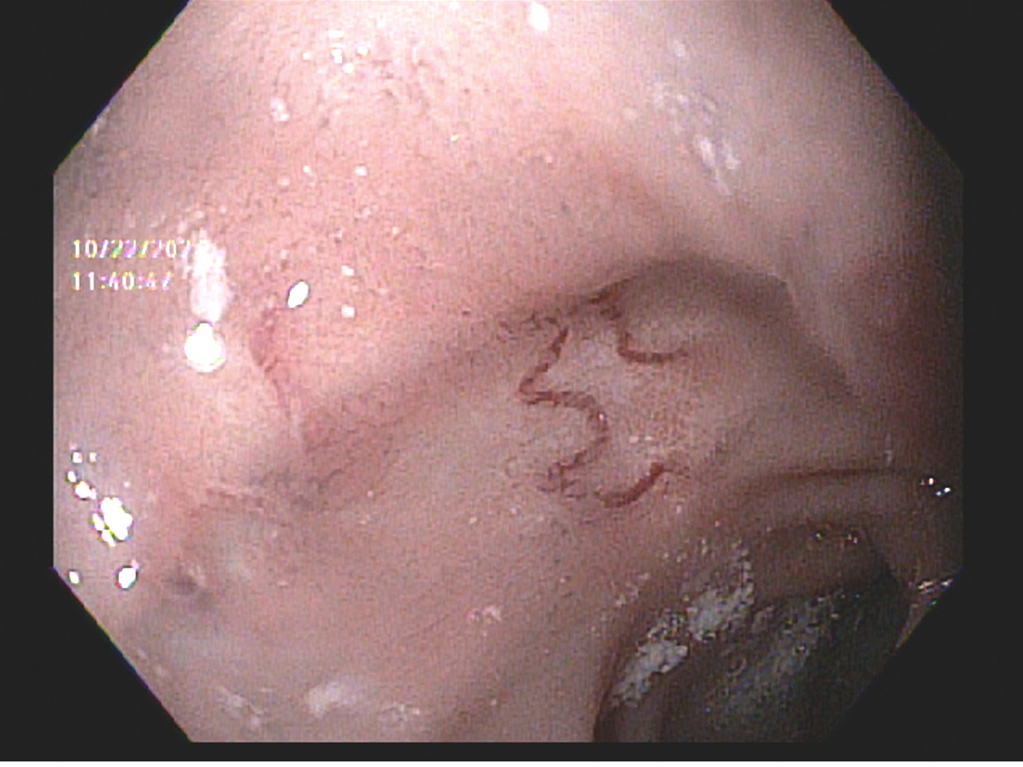
Figure: Figure 1. Linear bluish hue indicative of duodenal varices seen in the duodenal bulb, with red wale sign seen at the anastomosis site.
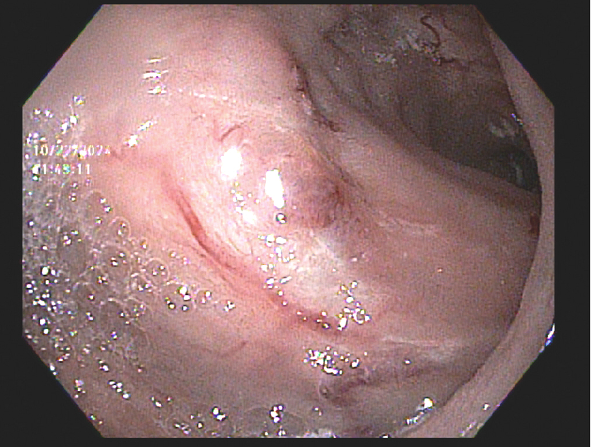
Figure: Figure 2. Linear bluish hue of duodenal varices with erythema seen in the duodenal bulb.
Disclosures:
Makul Sharma indicated no relevant financial relationships.
Urmimala Chaudhuri indicated no relevant financial relationships.
Hassan Zreik indicated no relevant financial relationships.
Mauricio Carballo indicated no relevant financial relationships.
Makul Sharma, MS1, Urmimala Chaudhuri, DO2, Hassan Zreik, MD3, Mauricio Carballo, MD4. P3146 - A Case of Recurrent Duodenal Varices, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
