Monday Poster Session
Category: GI Bleeding
P3141 - Small Bowel Varix: An Elusive Source of Upper GI Bleed in an Elderly Patient
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Joanna Yuen, DO, MA (she/her/hers)
Ochsner Health Clinic Foundation
Presenting Author(s)
Joanna Yuen, DO, MA1, Andrew Stoddard, MD1, Patt Panuncillon, DO2, Ricardo David Espinosa, MD1, Jaya Bommireddipally, MD1, Reinaldo Quevedo, MD3
1Ochsner Health Clinic Foundation, New Orleans, LA; 2Ochsner Health Clinic Foundation, Pearland, TX; 3Ochsner Medical Center, New Orleans, LA
Introduction: Small bowel varices (SBV) account for 5-10% of all gastrointestinal (GI) bleeds. They can cause life-threatening hemorrhage with a mortality rate of up to 40%. SBV are most commonly seen in patients with cirrhosis and do not often form due to other etiologies. This case describes the rare discovery of a duodenal variceal bleed in a non-cirrhotic patient.
Case Description/
Methods: An 83-year-old woman presented with generalized weakness, presyncope, and melena. She has a remote history of breast cancer, melanoma, and renal cell carcinoma (RCC) with metastasis to the pancreas and spleen. She underwent distal pancreatectomy and splenectomy in 2006. Labs were notable for a low hemoglobin 5.1, normal platelets 292, and high blood urea nitrogen 47. Esophagogastroduodenoscopy (EGD) revealed a normal esophagus, large hiatal hernia with Cameron ulcers, and a duodenal varix actively spurting blood. Hemostatic clips were placed to control the bleeding, though unsuccessful. Case was discussed with Interventional Radiology (IR) and the patient was urgently sent for computed tomography angiogram (CTA). CTA was negative for active bleeding but demonstrated a tumor thrombus and increased pancreatic body mass with direct invasion into the adjacent duodenum. Successful embolization of the gastroepiploic and inferior pancreaticoduodenal arteries supplying the tumor was performed by IR, resulting in cessation of bleeding.
Discussion: Most SBV are caused by portal hypertension as a sequela of cirrhosis. SBV caused by mesenteric venous obstruction are exceedingly rare. The patient’s RCC with worsening metastases to the pancreas resulted in a tumor thrombus with formation of tortuous, dilated collateral veins that invaded into the duodenum, causing GI bleed. The best treatments for SBV have yet to be established given its rarity. Treatment with endoscopy are commonly used for acute bleeds before more invasive approaches like surgery or radiologic intervention are considered. Studies have looked into enteroscopic injection sclerotherapy, hemostatic clip placement, and band ligation to achieve hemostasis, but rebleeding is common. Procedures such as transjugular intrahepatic portosystemic shunt or balloon-occluded retrograde transvenous obliteration are eventually considered to reduce the portal pressure gradient and achieve long-term hemostasis. Multidisciplinary discussion in medicine is therefore crucial to achieving the best outcomes for patients presenting with GI bleeds from SBV.
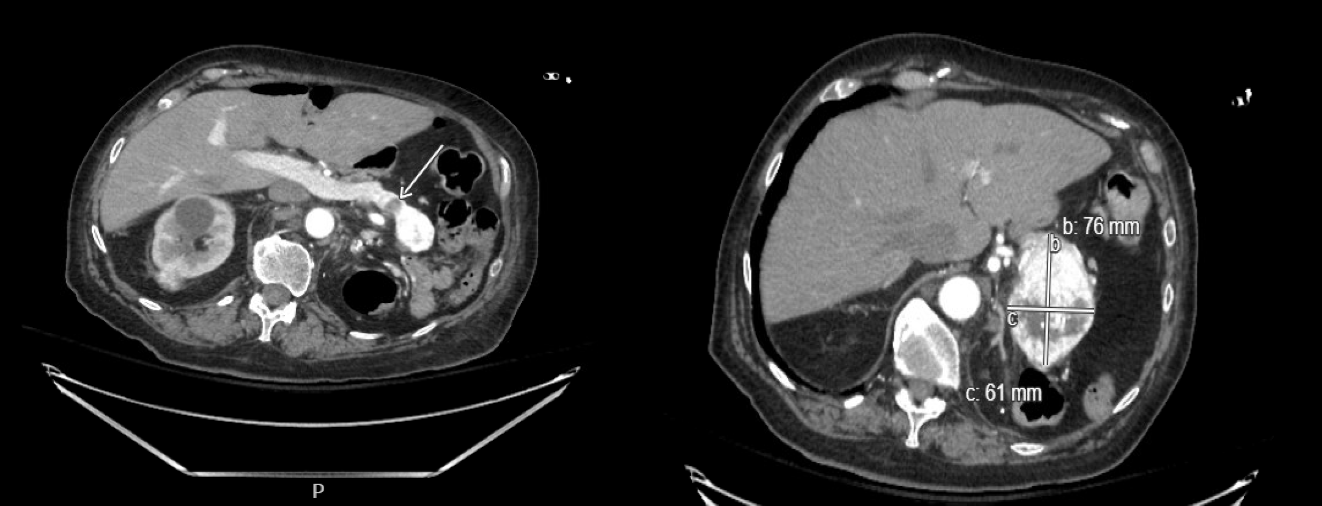
Figure: Figure 1. Varix with suspected fibrin clot on left (yellow arrow). Boston Scientific clip placed at duodenal varix on right.
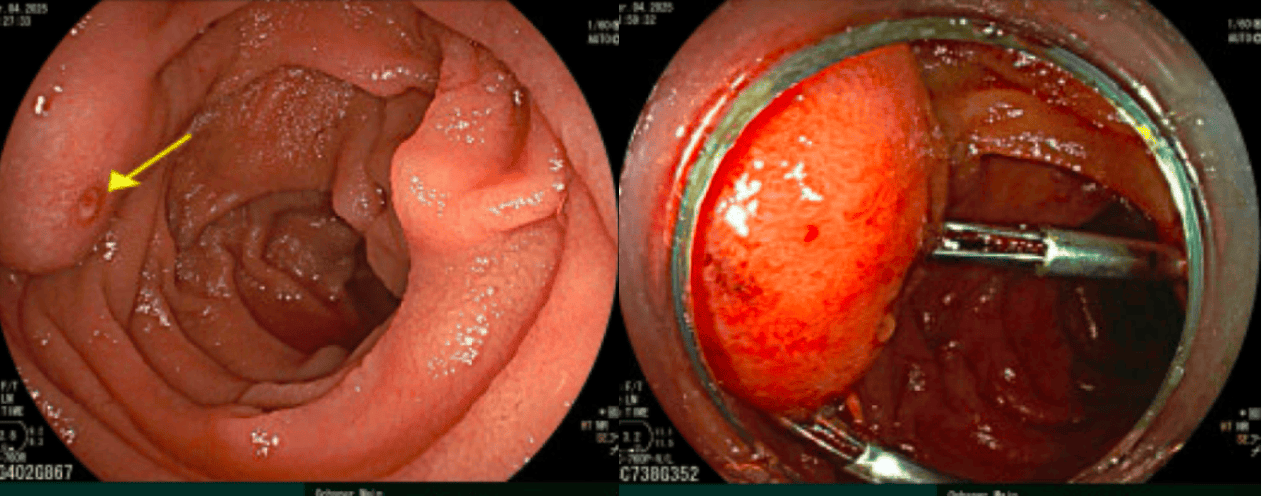
Figure: Figure 2. CTA of the abdomen and pelvis demonstrating venous collateral intraluminal filling defect with mild enhancement, suspicious for tumor thrombus, on the left (white arrow). Pancreatic mass at the body of significant tortuous and dilated collaterals, increased in size from before (6.9 x 6.4 x 5.0 cm, previously 5.3 x 5.6 x 3.9 cm), with direct invasion of adjacent distal duodenum on the right.
Disclosures:
Joanna Yuen indicated no relevant financial relationships.
Andrew Stoddard indicated no relevant financial relationships.
Patt Panuncillon indicated no relevant financial relationships.
Ricardo David Espinosa indicated no relevant financial relationships.
Jaya Bommireddipally indicated no relevant financial relationships.
Reinaldo Quevedo indicated no relevant financial relationships.
Joanna Yuen, DO, MA1, Andrew Stoddard, MD1, Patt Panuncillon, DO2, Ricardo David Espinosa, MD1, Jaya Bommireddipally, MD1, Reinaldo Quevedo, MD3. P3141 - Small Bowel Varix: An Elusive Source of Upper GI Bleed in an Elderly Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ochsner Health Clinic Foundation, New Orleans, LA; 2Ochsner Health Clinic Foundation, Pearland, TX; 3Ochsner Medical Center, New Orleans, LA
Introduction: Small bowel varices (SBV) account for 5-10% of all gastrointestinal (GI) bleeds. They can cause life-threatening hemorrhage with a mortality rate of up to 40%. SBV are most commonly seen in patients with cirrhosis and do not often form due to other etiologies. This case describes the rare discovery of a duodenal variceal bleed in a non-cirrhotic patient.
Case Description/
Methods: An 83-year-old woman presented with generalized weakness, presyncope, and melena. She has a remote history of breast cancer, melanoma, and renal cell carcinoma (RCC) with metastasis to the pancreas and spleen. She underwent distal pancreatectomy and splenectomy in 2006. Labs were notable for a low hemoglobin 5.1, normal platelets 292, and high blood urea nitrogen 47. Esophagogastroduodenoscopy (EGD) revealed a normal esophagus, large hiatal hernia with Cameron ulcers, and a duodenal varix actively spurting blood. Hemostatic clips were placed to control the bleeding, though unsuccessful. Case was discussed with Interventional Radiology (IR) and the patient was urgently sent for computed tomography angiogram (CTA). CTA was negative for active bleeding but demonstrated a tumor thrombus and increased pancreatic body mass with direct invasion into the adjacent duodenum. Successful embolization of the gastroepiploic and inferior pancreaticoduodenal arteries supplying the tumor was performed by IR, resulting in cessation of bleeding.
Discussion: Most SBV are caused by portal hypertension as a sequela of cirrhosis. SBV caused by mesenteric venous obstruction are exceedingly rare. The patient’s RCC with worsening metastases to the pancreas resulted in a tumor thrombus with formation of tortuous, dilated collateral veins that invaded into the duodenum, causing GI bleed. The best treatments for SBV have yet to be established given its rarity. Treatment with endoscopy are commonly used for acute bleeds before more invasive approaches like surgery or radiologic intervention are considered. Studies have looked into enteroscopic injection sclerotherapy, hemostatic clip placement, and band ligation to achieve hemostasis, but rebleeding is common. Procedures such as transjugular intrahepatic portosystemic shunt or balloon-occluded retrograde transvenous obliteration are eventually considered to reduce the portal pressure gradient and achieve long-term hemostasis. Multidisciplinary discussion in medicine is therefore crucial to achieving the best outcomes for patients presenting with GI bleeds from SBV.
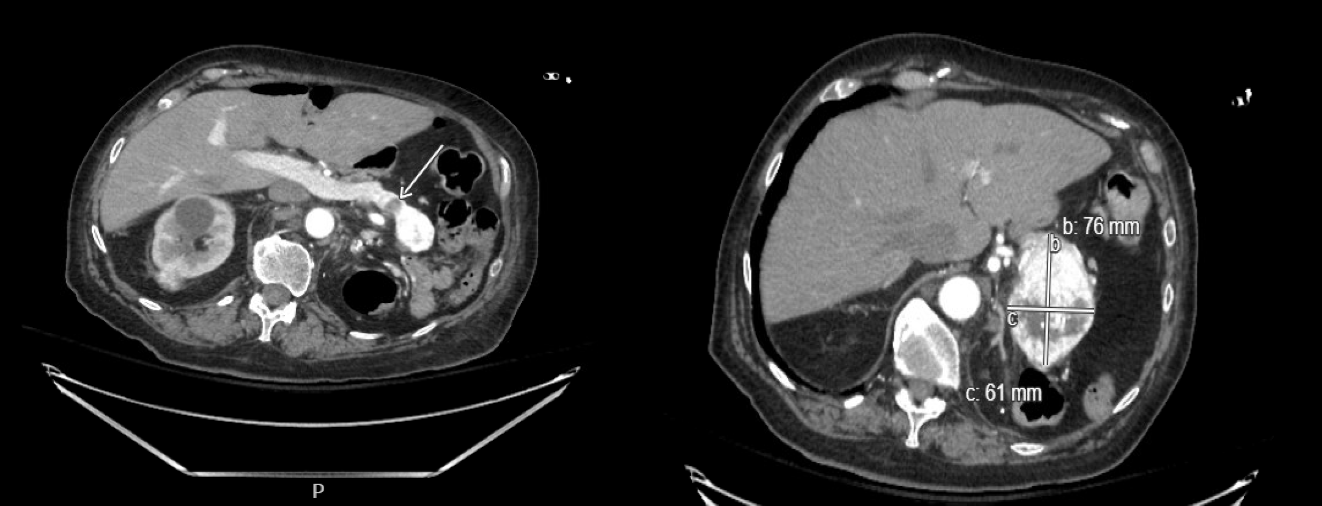
Figure: Figure 1. Varix with suspected fibrin clot on left (yellow arrow). Boston Scientific clip placed at duodenal varix on right.
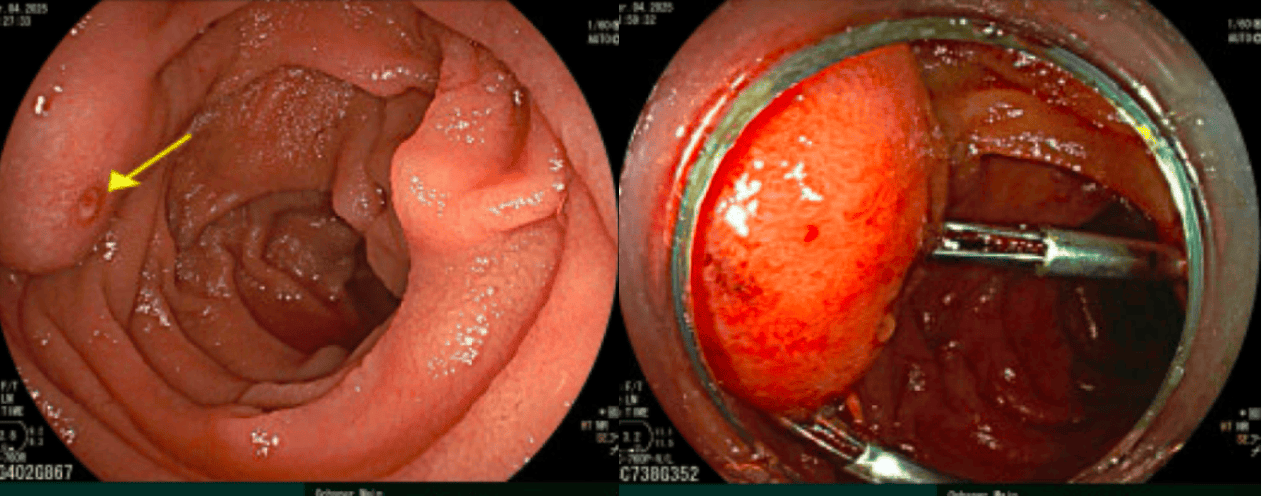
Figure: Figure 2. CTA of the abdomen and pelvis demonstrating venous collateral intraluminal filling defect with mild enhancement, suspicious for tumor thrombus, on the left (white arrow). Pancreatic mass at the body of significant tortuous and dilated collaterals, increased in size from before (6.9 x 6.4 x 5.0 cm, previously 5.3 x 5.6 x 3.9 cm), with direct invasion of adjacent distal duodenum on the right.
Disclosures:
Joanna Yuen indicated no relevant financial relationships.
Andrew Stoddard indicated no relevant financial relationships.
Patt Panuncillon indicated no relevant financial relationships.
Ricardo David Espinosa indicated no relevant financial relationships.
Jaya Bommireddipally indicated no relevant financial relationships.
Reinaldo Quevedo indicated no relevant financial relationships.
Joanna Yuen, DO, MA1, Andrew Stoddard, MD1, Patt Panuncillon, DO2, Ricardo David Espinosa, MD1, Jaya Bommireddipally, MD1, Reinaldo Quevedo, MD3. P3141 - Small Bowel Varix: An Elusive Source of Upper GI Bleed in an Elderly Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
