Monday Poster Session
Category: GI Bleeding
P3140 - From Withdrawal to Hematemesis: A Rare Case of Cocaine-Associated Necrotizing Esophagitis With Refractory Upper Gastrointestinal Bleeding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Taha Bin Arif, MBBS, MD (he/him/his)
Sinai Hospital of Baltimore, The George Washington University Regional Medical Campus
Baltimore, MD
Presenting Author(s)
Taha Bin Arif, MBBS, MD, Sonia Sugumar, MD, Ruchita Jadhav, MBBS, MD, MPH, Tahir Shaikh, MD
Sinai Hospital of Baltimore, The George Washington University Regional Medical Campus, Baltimore, MD
Introduction: Cocaine use is implicated with a plethora of complications including but not limited to coronary vasoconstriction, dysrhythmias, seizures, etc. A less commonly seen side effect of cocaine use are GI manifestations, which may appear as mesenteric ischemia, gastric ulcers, and rarely, necrotizing esophagitis. This case illustrates the rare occurrence of necrotizing esophagitis in the setting of polysubstance abuse and highlights the complexity of managing recurrent GI bleeding in patients with ongoing drug use.
Case Description/
Methods: A 38-year-old woman with a medical history including intravenous drug use (xylazine, methadone, and cocaine), hypertension, and a remote pulmonary embolism presented with symptoms of opioid withdrawal after missing methadone doses. During hospitalization, she developed hematemesis and melena. Laboratory workup revealed profound anemia (hemoglobin 6.1 g/dL), leukocytosis, acute kidney injury, and elevated liver enzymes. She was transfused and started on proton pump inhibitor therapy. EGD revealed circumferential black necrosis of the esophagus consistent with necrotizing esophagitis, likely cocaine induced. Additionally, multiple gastric ulcers were found, including a Forrest Ib bleeding ulcer at the pylorus which was treated with epinephrine injection and endoscopic clip placement. Despite initial management, the patient had recurrent GI bleeding requiring ICU admission, multiple transfusions, and repeat EGDs. A subsequent CT angiography did not show active bleeding. Endoscopic suturing was performed due to concerns about potential rebleeding and incomplete visualization of a large posterior antral ulcer. Last EGD showed healing esophagitis, resolved ulcers, and a newly identified 2–3 cm submucosal mass in the duodenal bulb, prompting plans for outpatient endoscopic ultrasound with fine needle aspiration.
Discussion: Necrotizing esophagitis or black esophagus is characterized by circumferential black discoloration of the distal esophagus with a sharp demarcation at the gastroesophageal junction, and histologically by mucosal necrosis with disruption of muscle fibers, typically without identifiable infectious agents. It is a recognized but uncommon condition in gastroenterology, associated with a reported mortality rate of up to 38%. The vasoconstrictive properties of cocaine, which can lead to ischemic gastrointestinal injury—including juxta-pyloric and duodenal ulceration or perforation—likely contributed to the mucosal ischemia and necrosis seen in this patient.
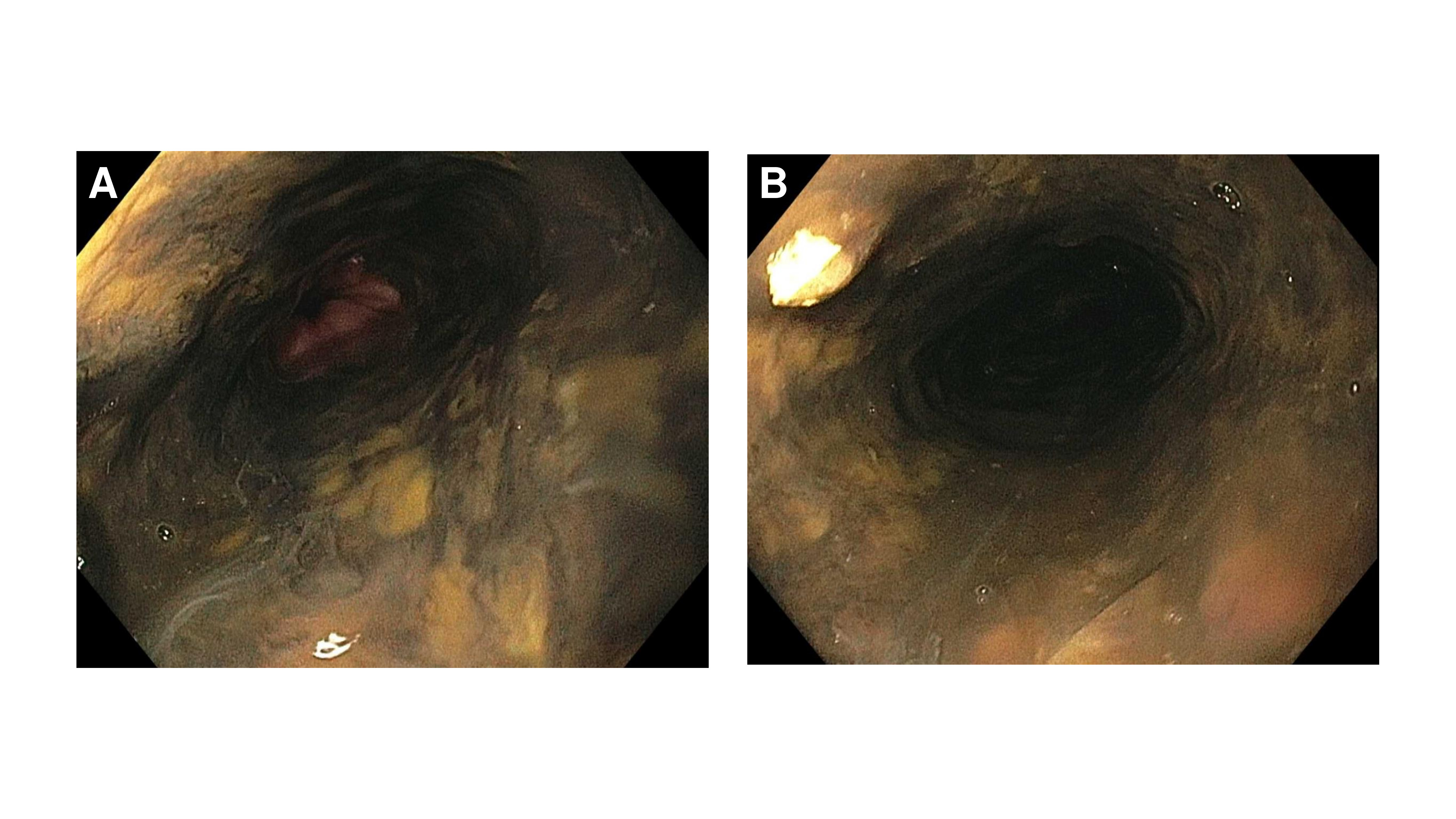
Figure: Figure 1A: Severe mucosal changes characterized by circumferential black discoloration and ulceration in the esophagus consistent with necrotizing esophagitis; 1B: Possible cocaine induced necrotizing esophagitis seen on EGD.
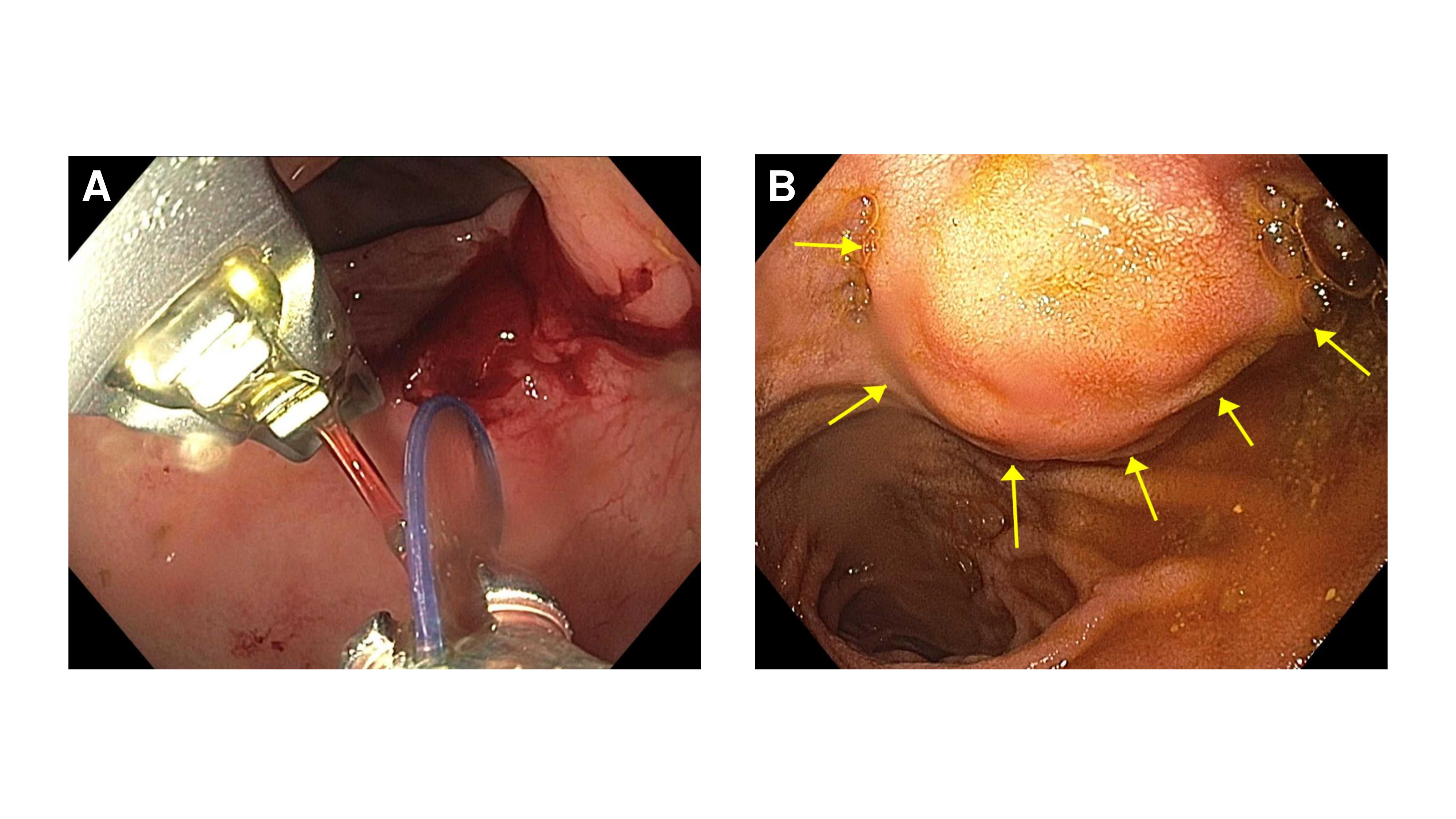
Figure: Figure 2A: Approximation of large posterior antal ulcer using endoscopic sutures ; 2B: Submucosal duodenal bulb mass seen on subsequent EGDs.
Disclosures:
Taha Bin Arif indicated no relevant financial relationships.
Sonia Sugumar indicated no relevant financial relationships.
Ruchita Jadhav indicated no relevant financial relationships.
Tahir Shaikh indicated no relevant financial relationships.
Taha Bin Arif, MBBS, MD, Sonia Sugumar, MD, Ruchita Jadhav, MBBS, MD, MPH, Tahir Shaikh, MD. P3140 - From Withdrawal to Hematemesis: A Rare Case of Cocaine-Associated Necrotizing Esophagitis With Refractory Upper Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Sinai Hospital of Baltimore, The George Washington University Regional Medical Campus, Baltimore, MD
Introduction: Cocaine use is implicated with a plethora of complications including but not limited to coronary vasoconstriction, dysrhythmias, seizures, etc. A less commonly seen side effect of cocaine use are GI manifestations, which may appear as mesenteric ischemia, gastric ulcers, and rarely, necrotizing esophagitis. This case illustrates the rare occurrence of necrotizing esophagitis in the setting of polysubstance abuse and highlights the complexity of managing recurrent GI bleeding in patients with ongoing drug use.
Case Description/
Methods: A 38-year-old woman with a medical history including intravenous drug use (xylazine, methadone, and cocaine), hypertension, and a remote pulmonary embolism presented with symptoms of opioid withdrawal after missing methadone doses. During hospitalization, she developed hematemesis and melena. Laboratory workup revealed profound anemia (hemoglobin 6.1 g/dL), leukocytosis, acute kidney injury, and elevated liver enzymes. She was transfused and started on proton pump inhibitor therapy. EGD revealed circumferential black necrosis of the esophagus consistent with necrotizing esophagitis, likely cocaine induced. Additionally, multiple gastric ulcers were found, including a Forrest Ib bleeding ulcer at the pylorus which was treated with epinephrine injection and endoscopic clip placement. Despite initial management, the patient had recurrent GI bleeding requiring ICU admission, multiple transfusions, and repeat EGDs. A subsequent CT angiography did not show active bleeding. Endoscopic suturing was performed due to concerns about potential rebleeding and incomplete visualization of a large posterior antral ulcer. Last EGD showed healing esophagitis, resolved ulcers, and a newly identified 2–3 cm submucosal mass in the duodenal bulb, prompting plans for outpatient endoscopic ultrasound with fine needle aspiration.
Discussion: Necrotizing esophagitis or black esophagus is characterized by circumferential black discoloration of the distal esophagus with a sharp demarcation at the gastroesophageal junction, and histologically by mucosal necrosis with disruption of muscle fibers, typically without identifiable infectious agents. It is a recognized but uncommon condition in gastroenterology, associated with a reported mortality rate of up to 38%. The vasoconstrictive properties of cocaine, which can lead to ischemic gastrointestinal injury—including juxta-pyloric and duodenal ulceration or perforation—likely contributed to the mucosal ischemia and necrosis seen in this patient.
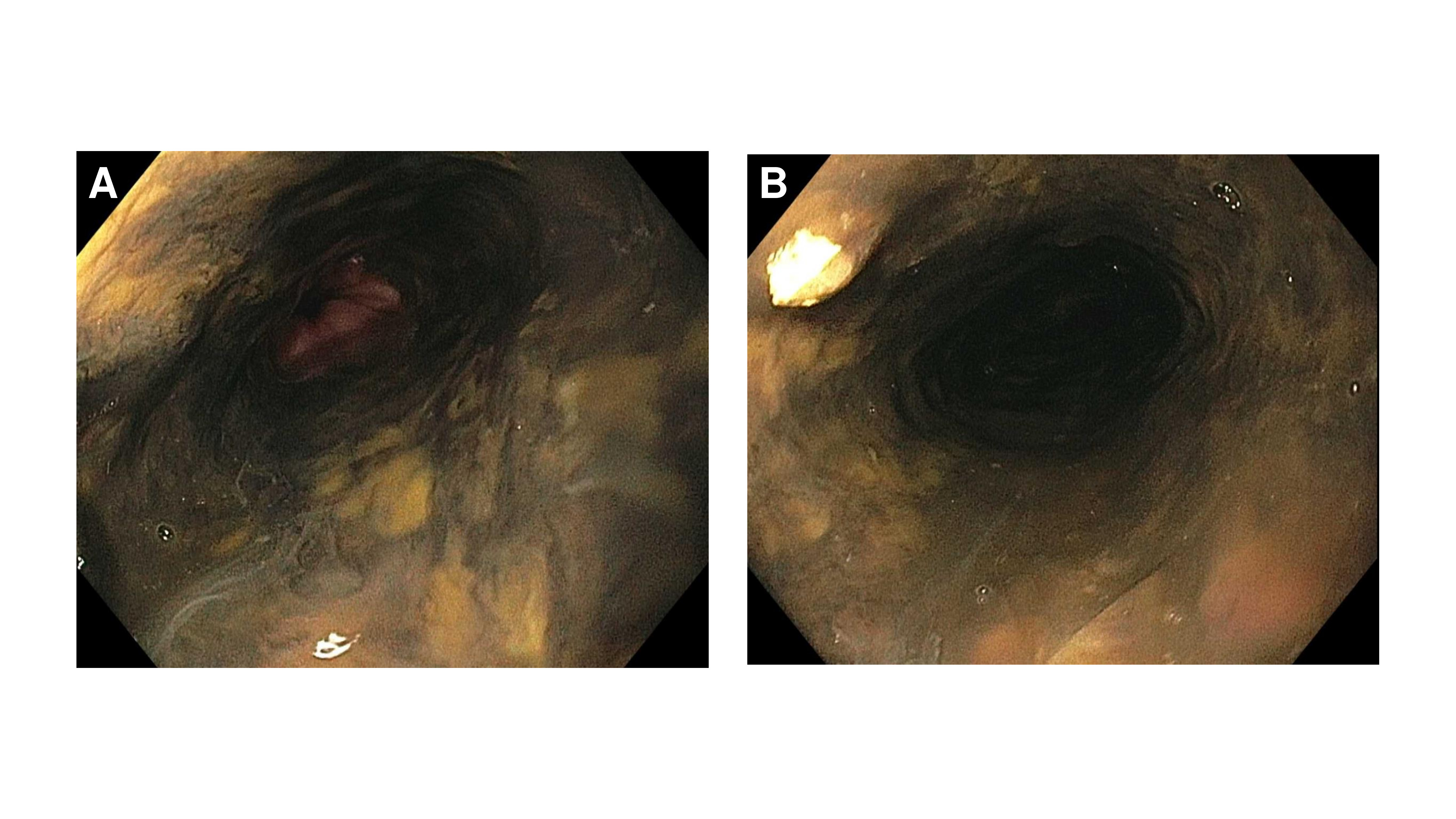
Figure: Figure 1A: Severe mucosal changes characterized by circumferential black discoloration and ulceration in the esophagus consistent with necrotizing esophagitis; 1B: Possible cocaine induced necrotizing esophagitis seen on EGD.
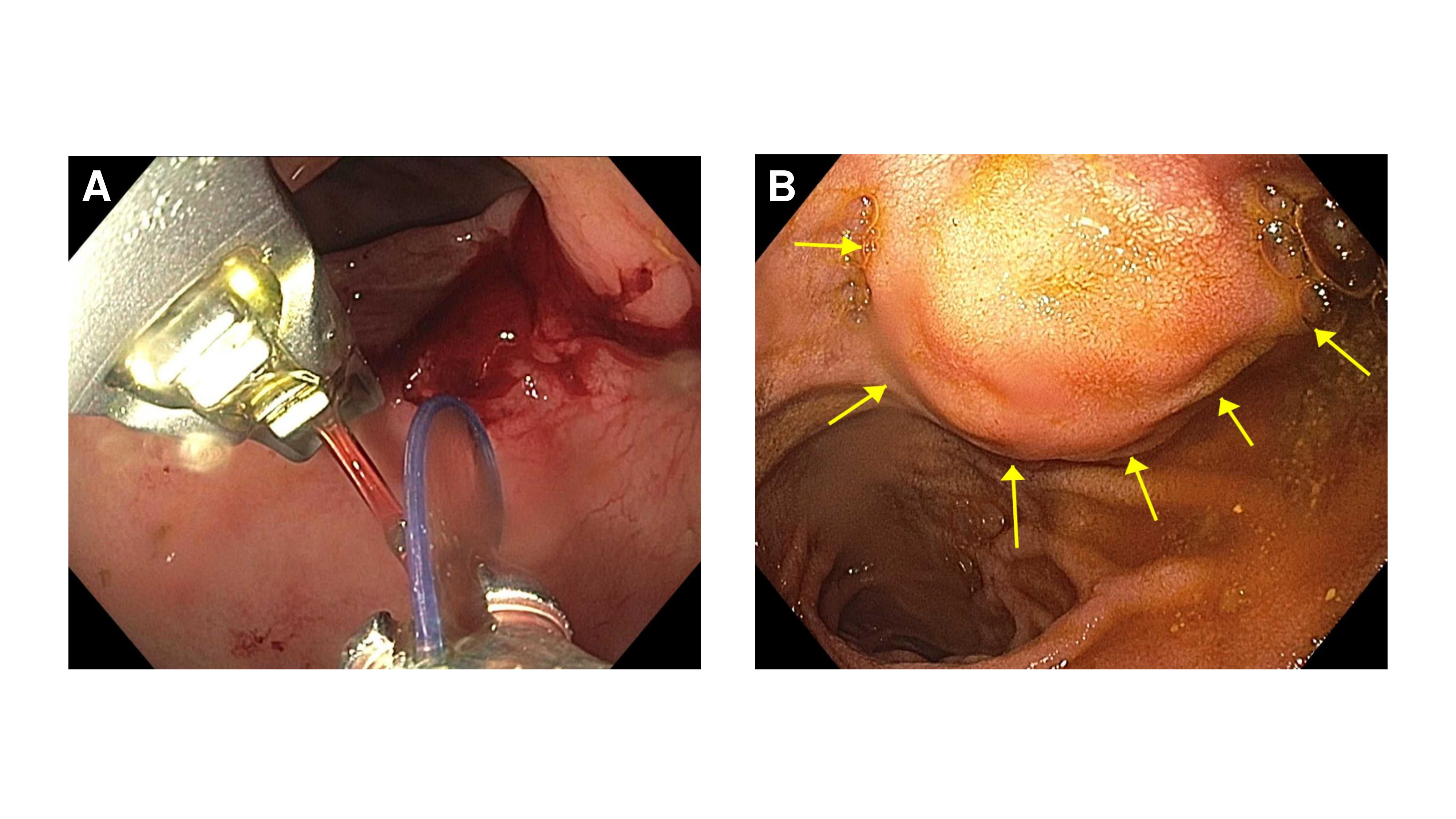
Figure: Figure 2A: Approximation of large posterior antal ulcer using endoscopic sutures ; 2B: Submucosal duodenal bulb mass seen on subsequent EGDs.
Disclosures:
Taha Bin Arif indicated no relevant financial relationships.
Sonia Sugumar indicated no relevant financial relationships.
Ruchita Jadhav indicated no relevant financial relationships.
Tahir Shaikh indicated no relevant financial relationships.
Taha Bin Arif, MBBS, MD, Sonia Sugumar, MD, Ruchita Jadhav, MBBS, MD, MPH, Tahir Shaikh, MD. P3140 - From Withdrawal to Hematemesis: A Rare Case of Cocaine-Associated Necrotizing Esophagitis With Refractory Upper Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
