Monday Poster Session
Category: IBD
P3278 - Abnormal MUC1 Expression: A Biomarker of Post-Operative Crohn’s Disease Recurrence
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Madeleine A. Howard, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Madeleine A. Howard, MD1, Irene K. Yan, 1, Raouf Nakhleh, MD2, Fadi F.. Francis, MD1, Michael Camilleri, MD, DSc3, Francis A.. Farraye, MD, MSc, MACG1, Jana G. Hashash, MD, MSc, FACG1
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic, St. Augustine, FL; 3Mayo Clinic, Rochester, MN
Introduction: Mucin 1 (MUC1) is a transmembrane epithelial glycoprotein that plays a crucial role in maintaining mucosal integrity and protection against luminal insults. Under normal physiological conditions, MUC1 expression follows a tightly regulated pattern contributing to the mucus barrier that separates epithelial cells from the intestinal microbiota and other potentially harmful agents. Emerging evidence suggests that alterations in mucin expression and glycosylation patterns occur during inflammatory processes, potentially serving as molecular signatures of disease. This study investigates the hypothesis that abnormal MUC1 expression patterns could serve as a specific biomarker for postoperative recurrent Crohn’s disease (CD), with overexpression of the hypoglycosylated (abnormal form) MUC1 being associated proportionally to the degree of inflammation. By establishing such a relationship, we aim to provide a foundation for developing novel diagnostic approaches.
Methods: Patients with CD and prior ileocecal resection were identified through the electronic medical records. Within that group of patients, we identified those who had a colonoscopy with biopsies from their neo-terminal ileum. Archived tissue from the neo-terminal ileum of these patients was obtained and stained for a primary antibody against the abnormal hypoglycosylated MUC1 (MUC1_VU4H5). Each slide was graded based on quantity and intensity of the hypoglycosylated MUC1. The average quantity and intensity of abnormal MUC1 was used to represent the score of abnormal MUC1 expression for each patient.
Results: A total of 89 neo-terminal ileum archived tissue samples from patients with CD were stained for hypoglycosylated MUC1. Of these patients, 7 were given a Rutgeerts score of i0 during their colonoscopy, 15 a score of i1, 19 i2, 21 i3, and 27 a score of i4.
Patients with a Rutgeerts ileal score of i0 exhibited no to minimal expression of the abnormal hypoglycosylated MUC1 while patients with more severe postoperative recurrence (Rutgeerts i3 and i4) had higher levels of the hypoglycosylated form (Figures 1, 2).
Discussion: Our findings demonstrate a significant association between abnormal hypoglycosylated MUC1 expression and degree of postoperative CD recurrence, with overexpression levels proportionally reflecting the degree of inflammation. This relationship provides compelling evidence for MUC1 as a potential biomarker with quantitative properties that could transform the assessment and monitoring of postoperative CD.
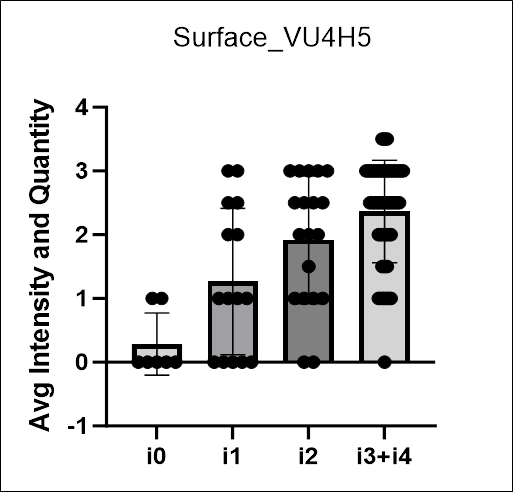
Figure: Quantification of hypoglycosylated abnormal MUC1 expression from the neo-terminal ileum tissue of patients with different degrees of recurrent Crohn’s disease.

Figure: Representative images showing the 4H5 MUC1 stains in neo-terminal ileum tissue of patients with different degrees of postoperative Crohn’s disease recurrence as categorized by Rutgeerts score.
Disclosures:
Madeleine Howard indicated no relevant financial relationships.
Irene Yan indicated no relevant financial relationships.
Raouf Nakhleh indicated no relevant financial relationships.
Fadi Francis indicated no relevant financial relationships.
Michael Camilleri: Alfasigma – Consultant. Amylyx – Consultant. Biocodex – Grant/Research Support. BioKier – Consultant. Brightseed Bio – Consultant, Grant/Research Support. Coloplast – Consultant. Dignify Therapeutics – Stock Options. Intercept – Consultant. Invea – Consultant. Kallyope – Consultant. McDermott Will & Emery – Consultant. Medpace – Consultant. Monteresearch – Consultant. Neurogastrx – Consultant. NGM Biopharmaceuticals – Grant/Research Support. Pfizer – Grant/Research Support. Phenomix – Stock Options. Renexxion – Consultant. SKYE Bioscience – Consultant. Sumitomo – Consultant. Synlogic – Consultant. Vanda – Grant/Research Support.
Francis Farraye: Astellas – Advisory Committee/Board Member. Avalo – Advisory Committee/Board Member. Bausch – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member, Stock Options. Janssen – Advisory Committee/Board Member. Lilly – DSMB. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Jana Hashash: BMS – Ad Board.
Madeleine A. Howard, MD1, Irene K. Yan, 1, Raouf Nakhleh, MD2, Fadi F.. Francis, MD1, Michael Camilleri, MD, DSc3, Francis A.. Farraye, MD, MSc, MACG1, Jana G. Hashash, MD, MSc, FACG1. P3278 - Abnormal MUC1 Expression: A Biomarker of Post-Operative Crohn’s Disease Recurrence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic, St. Augustine, FL; 3Mayo Clinic, Rochester, MN
Introduction: Mucin 1 (MUC1) is a transmembrane epithelial glycoprotein that plays a crucial role in maintaining mucosal integrity and protection against luminal insults. Under normal physiological conditions, MUC1 expression follows a tightly regulated pattern contributing to the mucus barrier that separates epithelial cells from the intestinal microbiota and other potentially harmful agents. Emerging evidence suggests that alterations in mucin expression and glycosylation patterns occur during inflammatory processes, potentially serving as molecular signatures of disease. This study investigates the hypothesis that abnormal MUC1 expression patterns could serve as a specific biomarker for postoperative recurrent Crohn’s disease (CD), with overexpression of the hypoglycosylated (abnormal form) MUC1 being associated proportionally to the degree of inflammation. By establishing such a relationship, we aim to provide a foundation for developing novel diagnostic approaches.
Methods: Patients with CD and prior ileocecal resection were identified through the electronic medical records. Within that group of patients, we identified those who had a colonoscopy with biopsies from their neo-terminal ileum. Archived tissue from the neo-terminal ileum of these patients was obtained and stained for a primary antibody against the abnormal hypoglycosylated MUC1 (MUC1_VU4H5). Each slide was graded based on quantity and intensity of the hypoglycosylated MUC1. The average quantity and intensity of abnormal MUC1 was used to represent the score of abnormal MUC1 expression for each patient.
Results: A total of 89 neo-terminal ileum archived tissue samples from patients with CD were stained for hypoglycosylated MUC1. Of these patients, 7 were given a Rutgeerts score of i0 during their colonoscopy, 15 a score of i1, 19 i2, 21 i3, and 27 a score of i4.
Patients with a Rutgeerts ileal score of i0 exhibited no to minimal expression of the abnormal hypoglycosylated MUC1 while patients with more severe postoperative recurrence (Rutgeerts i3 and i4) had higher levels of the hypoglycosylated form (Figures 1, 2).
Discussion: Our findings demonstrate a significant association between abnormal hypoglycosylated MUC1 expression and degree of postoperative CD recurrence, with overexpression levels proportionally reflecting the degree of inflammation. This relationship provides compelling evidence for MUC1 as a potential biomarker with quantitative properties that could transform the assessment and monitoring of postoperative CD.
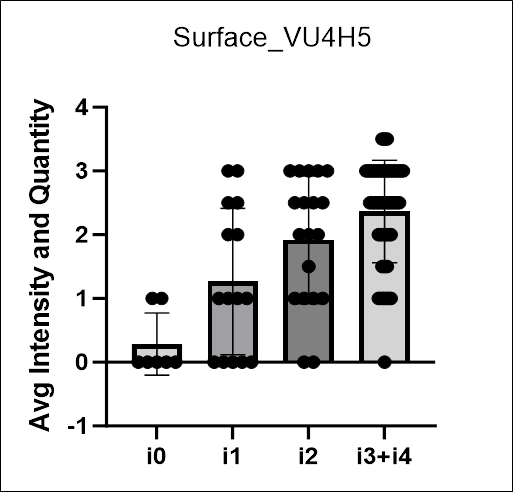
Figure: Quantification of hypoglycosylated abnormal MUC1 expression from the neo-terminal ileum tissue of patients with different degrees of recurrent Crohn’s disease.

Figure: Representative images showing the 4H5 MUC1 stains in neo-terminal ileum tissue of patients with different degrees of postoperative Crohn’s disease recurrence as categorized by Rutgeerts score.
Disclosures:
Madeleine Howard indicated no relevant financial relationships.
Irene Yan indicated no relevant financial relationships.
Raouf Nakhleh indicated no relevant financial relationships.
Fadi Francis indicated no relevant financial relationships.
Michael Camilleri: Alfasigma – Consultant. Amylyx – Consultant. Biocodex – Grant/Research Support. BioKier – Consultant. Brightseed Bio – Consultant, Grant/Research Support. Coloplast – Consultant. Dignify Therapeutics – Stock Options. Intercept – Consultant. Invea – Consultant. Kallyope – Consultant. McDermott Will & Emery – Consultant. Medpace – Consultant. Monteresearch – Consultant. Neurogastrx – Consultant. NGM Biopharmaceuticals – Grant/Research Support. Pfizer – Grant/Research Support. Phenomix – Stock Options. Renexxion – Consultant. SKYE Bioscience – Consultant. Sumitomo – Consultant. Synlogic – Consultant. Vanda – Grant/Research Support.
Francis Farraye: Astellas – Advisory Committee/Board Member. Avalo – Advisory Committee/Board Member. Bausch – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member, Stock Options. Janssen – Advisory Committee/Board Member. Lilly – DSMB. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Jana Hashash: BMS – Ad Board.
Madeleine A. Howard, MD1, Irene K. Yan, 1, Raouf Nakhleh, MD2, Fadi F.. Francis, MD1, Michael Camilleri, MD, DSc3, Francis A.. Farraye, MD, MSc, MACG1, Jana G. Hashash, MD, MSc, FACG1. P3278 - Abnormal MUC1 Expression: A Biomarker of Post-Operative Crohn’s Disease Recurrence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

