Monday Poster Session
Category: IBD
P3372 - A Stitch in Time Saves Nine: Diagnosis of Small Bowel Adenocarcinoma in Crohn’s Prior to Surgery
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- WY
Wen Ting Yang, MD (she/her/hers)
Brown Medicine/Lifespan
Providence, RI
Presenting Author(s)
Wen Ting Yang, MD1, Michelle Kwon, MD1, Samir A. Shah, MD, FACG2
1Brown Medicine/Lifespan, Providence, RI; 2Gastroenterology Associates, Inc. powered by the GI alliance, Providence, RI
Introduction: Small bowel cancer is rare. Crohn’s ileitis is associated with up to a sixty-fold increased risk of developing small bowel adenocarcinoma (SBA). Despite this knowledge and advances in imaging, the diagnosis of SBA is challenging to make before surgical resection. We present a case of SBA in the ileum in a patient with longstanding Crohn’s to alert clinicians to consider SBA.
Case Description/
Methods: A 44-year-old male was diagnosed on colonoscopy with Crohn’s ileitis. He declined medical therapy as his symptoms were mild. At age 54, he developed new postprandial bloating and distention. Follow up colonoscopy showed mild narrowing of the ileum and small bowel series revealed 18 cm involvement of the ileum. Infliximab was initiated with clinical response for 8 years until he formed antibodies to infliximab and was switched to adalimumab during which he developed arthritic symptoms and self-discontinued therapy. He re-presented 2 years later with worsening symptoms. Both colonoscopy and magnetic resonance enterography (MRE) showed significant narrowing (~15-20 cm of the distal ileum) without proximal dilation at the ileocecal valve/distal ileum and active disease in the distal ileum, confirmed on biopsy. He was then switched to ustekinumab. Despite improving symptoms, repeat colonoscopy continued to show active disease, and medical therapy was subsequently changed to risankizumab. However, after finishing induction, he was hospitalized 3 times within 6 months for recurrent partial small bowel obstruction for which surgical resection was recommended but declined as he felt well in between episodes. CT and MRE showed narrowing and thickening of terminal ileum and no masses. Colonoscopy demonstrated an impassable stricture in the distal terminal ileum. Biopsy of the stricture, however, revealed moderately differentiated invasive adenocarcinoma. He underwent surgical resection, followed by adjuvant chemotherapy and remained in remission from both SBA and Crohn’s on risankizumab. Surgical pathology confirmed a 2.5 cm tumor without metastases.
Discussion: Our case highlights the diagnostic challenge of SBA before surgery. Routine imaging often does not show SBA until it is at a more advanced stage and most SBAs are diagnosed incidentally at surgery. Clinicians should consider the possibility of SBA in evaluating symptoms in patients with longstanding Crohn’s ileitis.
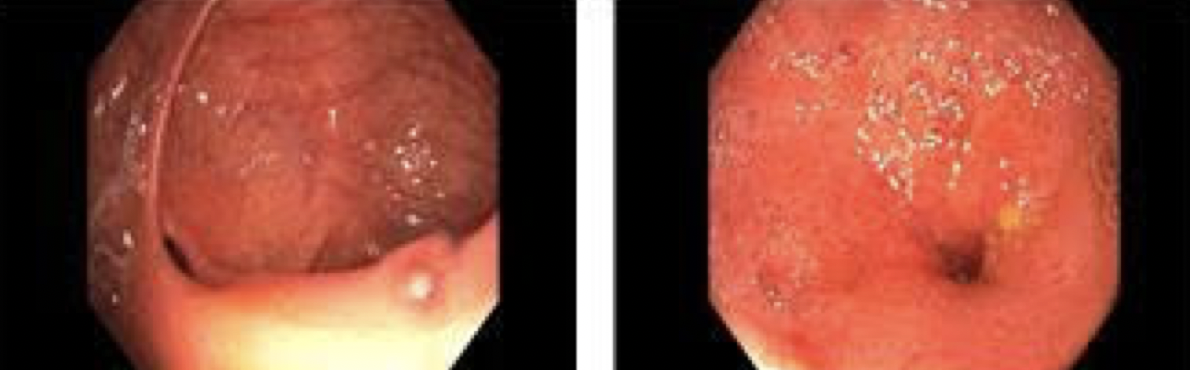
Figure: Figure 1. Colonoscopy showing ileocecal valve (left) and impassable stricture in terminal ileum ~1 cm from the ileocecal valve (right).

Figure: Figure 2. Surgical pathology revealing well differentiated invasive adenocarcinoma.
Disclosures:
Wen Ting Yang indicated no relevant financial relationships.
Michelle Kwon indicated no relevant financial relationships.
Samir Shah: pfizer – Advisory Committee/Board Member. Roche Information Systems – Consultant.
Wen Ting Yang, MD1, Michelle Kwon, MD1, Samir A. Shah, MD, FACG2. P3372 - A Stitch in Time Saves Nine: Diagnosis of Small Bowel Adenocarcinoma in Crohn’s Prior to Surgery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brown Medicine/Lifespan, Providence, RI; 2Gastroenterology Associates, Inc. powered by the GI alliance, Providence, RI
Introduction: Small bowel cancer is rare. Crohn’s ileitis is associated with up to a sixty-fold increased risk of developing small bowel adenocarcinoma (SBA). Despite this knowledge and advances in imaging, the diagnosis of SBA is challenging to make before surgical resection. We present a case of SBA in the ileum in a patient with longstanding Crohn’s to alert clinicians to consider SBA.
Case Description/
Methods: A 44-year-old male was diagnosed on colonoscopy with Crohn’s ileitis. He declined medical therapy as his symptoms were mild. At age 54, he developed new postprandial bloating and distention. Follow up colonoscopy showed mild narrowing of the ileum and small bowel series revealed 18 cm involvement of the ileum. Infliximab was initiated with clinical response for 8 years until he formed antibodies to infliximab and was switched to adalimumab during which he developed arthritic symptoms and self-discontinued therapy. He re-presented 2 years later with worsening symptoms. Both colonoscopy and magnetic resonance enterography (MRE) showed significant narrowing (~15-20 cm of the distal ileum) without proximal dilation at the ileocecal valve/distal ileum and active disease in the distal ileum, confirmed on biopsy. He was then switched to ustekinumab. Despite improving symptoms, repeat colonoscopy continued to show active disease, and medical therapy was subsequently changed to risankizumab. However, after finishing induction, he was hospitalized 3 times within 6 months for recurrent partial small bowel obstruction for which surgical resection was recommended but declined as he felt well in between episodes. CT and MRE showed narrowing and thickening of terminal ileum and no masses. Colonoscopy demonstrated an impassable stricture in the distal terminal ileum. Biopsy of the stricture, however, revealed moderately differentiated invasive adenocarcinoma. He underwent surgical resection, followed by adjuvant chemotherapy and remained in remission from both SBA and Crohn’s on risankizumab. Surgical pathology confirmed a 2.5 cm tumor without metastases.
Discussion: Our case highlights the diagnostic challenge of SBA before surgery. Routine imaging often does not show SBA until it is at a more advanced stage and most SBAs are diagnosed incidentally at surgery. Clinicians should consider the possibility of SBA in evaluating symptoms in patients with longstanding Crohn’s ileitis.
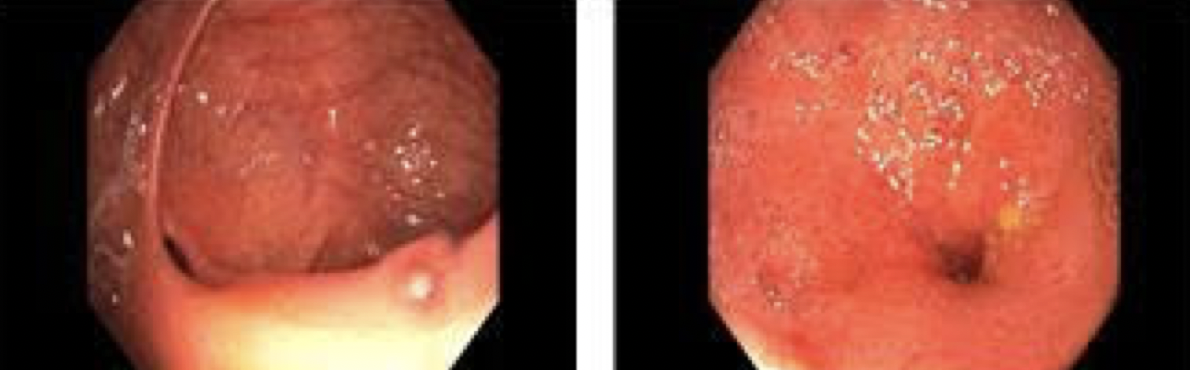
Figure: Figure 1. Colonoscopy showing ileocecal valve (left) and impassable stricture in terminal ileum ~1 cm from the ileocecal valve (right).

Figure: Figure 2. Surgical pathology revealing well differentiated invasive adenocarcinoma.
Disclosures:
Wen Ting Yang indicated no relevant financial relationships.
Michelle Kwon indicated no relevant financial relationships.
Samir Shah: pfizer – Advisory Committee/Board Member. Roche Information Systems – Consultant.
Wen Ting Yang, MD1, Michelle Kwon, MD1, Samir A. Shah, MD, FACG2. P3372 - A Stitch in Time Saves Nine: Diagnosis of Small Bowel Adenocarcinoma in Crohn’s Prior to Surgery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
