Monday Poster Session
Category: Infections and Microbiome
Proctitis Secondary to <i>Chlamydia Trachomatis</i> Infection: A Diagnostic Challenge in Anorectal Pathology
P3455 - Proctitis Secondary to Chlamydia Trachomatis Infection: A Diagnostic Challenge in Anorectal Pathology
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Charitha Karanam Ramapathy, MD (she/her/hers)
UAB Montgomery
Montgomery, AL
Presenting Author(s)
Charitha Karanam Ramapathy, MD1, Mahmoud Aryan, MD2, Kirk Russ, MD2
1UAB Montgomery, Montgomery, AL; 2University of Alabama at Birmingham, Birmingham, AL
Introduction: Sexually transmitted infections (STI) causing proctitis which is the inflammation of rectum is an extremely rare entity but has been on the rise in the last two decades. Their association with HIV is noteworthy. Here we present two cases of proctitis caused by chlamydia and syphilis.
Case Description/
Methods: 1. Patient is a 61-year-old male who presented for screening colonoscopy which showed a solitary ulcer in the distal rectum extending from the dentate line with no bleeding and biopsies were taken. He denies rectal prolapse, radiation history, anal intercouse, constipation. The IBD diagnostic panel is negative. Biopsy showed colorectal mucosa with ulceration and detached fibrinopurulent exudate with no evidence of malignancy and CMV immunostain is negative. Figure 1. Infectious workup showed reactive RPR 1: 256 titre and positive chlamydia. He was treated with Doxycycline 100 mg twice daily for 4 weeks.
2. Patient is a 35- year-old male presented with severe rectal pain. He had participated in anal intercouse in the past. CT abdomen and pelvis showed mild thickening of ascending colon. He underwent colonoscopy with findings consistent with ulceration about 15-20 mm in size submucosal swelling on either side anteriorly and just above the anal canal. Biopsies showed chronic active proctitis. Infectious workup showed reactive RPR 1: 128 titre. He was treated with penicillin G Benzathine 2,400,000 units intramuscular injection.
Discussion: Proctitis can result from both infectious and non-infectious origins. STI causes isolated proctitis with common pathogens including Neisseria gonorrhoeae, Treponema pallidum (syphilis), and Chlamydia trachomatis. Symptoms include bloody and mucoid discharge, anal pain and fever. Differentials for non infectious causes include IBD, ischemic colitis and non-steroidal anti-inflammatory drug enteropathy. Assessment of these conditions should involve standard diagnostic measures such as anoscopy or sigmoidoscopy, stool analysis for white blood cells, and microbiological testing—including evaluations for gonorrhea, chlamydia (with LGV PCR when accessible), herpes simplex via NAAT, and syphilis serology. It is imperative to diagnose STI related proctitis early to avoid complications from lymphatic spread leading to abscesses, granulomas, and fistulas. We want to emphasize the importance of STI among the differentials for proctitis, as it can avoid further diagnostic imaging and invasive procedures.
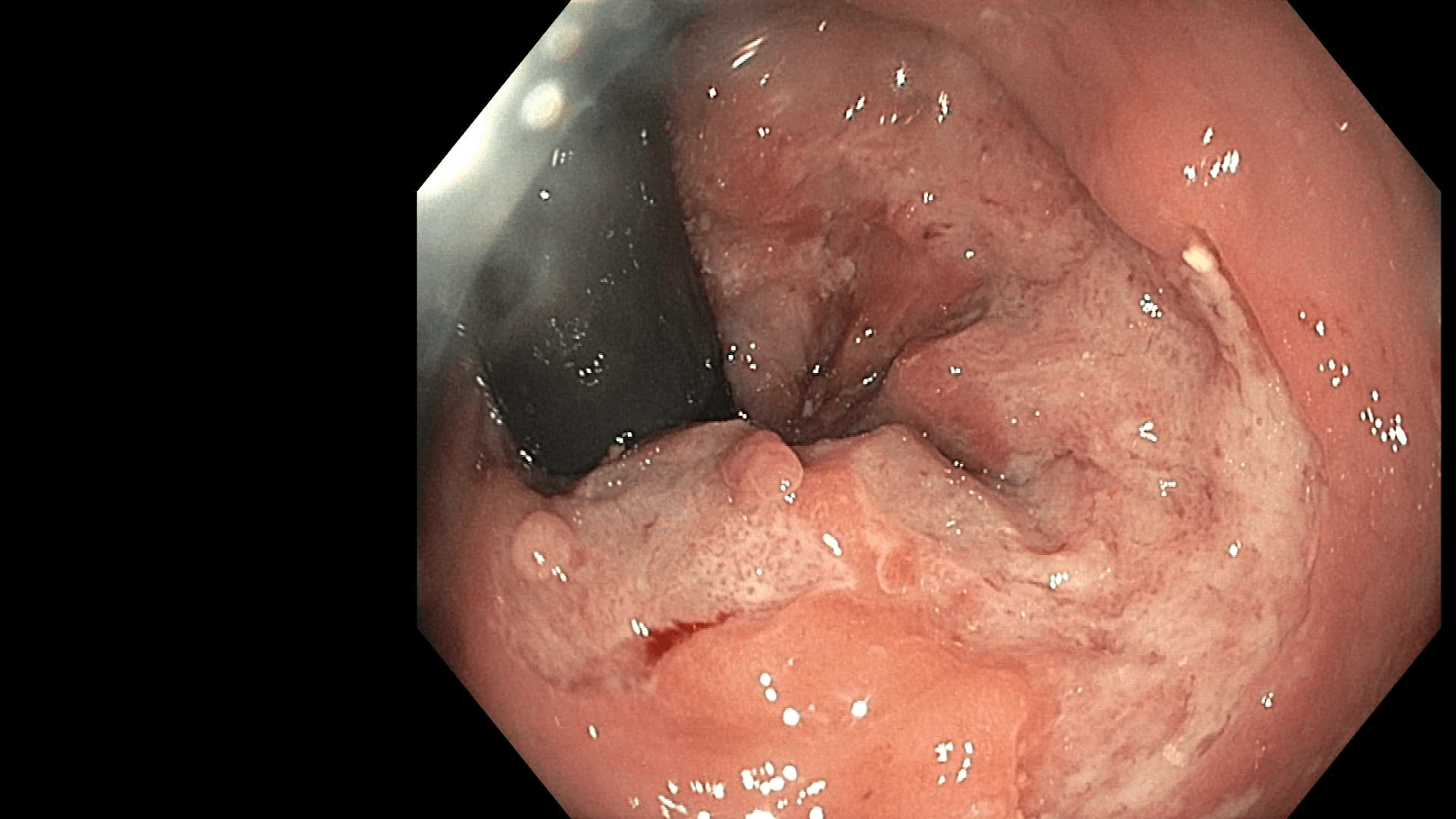
Figure: Figure 1
Disclosures:
Charitha Karanam Ramapathy indicated no relevant financial relationships.
Mahmoud Aryan indicated no relevant financial relationships.
Kirk Russ indicated no relevant financial relationships.
Charitha Karanam Ramapathy, MD1, Mahmoud Aryan, MD2, Kirk Russ, MD2. P3455 - Proctitis Secondary to <i>Chlamydia Trachomatis</i> Infection: A Diagnostic Challenge in Anorectal Pathology, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1UAB Montgomery, Montgomery, AL; 2University of Alabama at Birmingham, Birmingham, AL
Introduction: Sexually transmitted infections (STI) causing proctitis which is the inflammation of rectum is an extremely rare entity but has been on the rise in the last two decades. Their association with HIV is noteworthy. Here we present two cases of proctitis caused by chlamydia and syphilis.
Case Description/
Methods: 1. Patient is a 61-year-old male who presented for screening colonoscopy which showed a solitary ulcer in the distal rectum extending from the dentate line with no bleeding and biopsies were taken. He denies rectal prolapse, radiation history, anal intercouse, constipation. The IBD diagnostic panel is negative. Biopsy showed colorectal mucosa with ulceration and detached fibrinopurulent exudate with no evidence of malignancy and CMV immunostain is negative. Figure 1. Infectious workup showed reactive RPR 1: 256 titre and positive chlamydia. He was treated with Doxycycline 100 mg twice daily for 4 weeks.
2. Patient is a 35- year-old male presented with severe rectal pain. He had participated in anal intercouse in the past. CT abdomen and pelvis showed mild thickening of ascending colon. He underwent colonoscopy with findings consistent with ulceration about 15-20 mm in size submucosal swelling on either side anteriorly and just above the anal canal. Biopsies showed chronic active proctitis. Infectious workup showed reactive RPR 1: 128 titre. He was treated with penicillin G Benzathine 2,400,000 units intramuscular injection.
Discussion: Proctitis can result from both infectious and non-infectious origins. STI causes isolated proctitis with common pathogens including Neisseria gonorrhoeae, Treponema pallidum (syphilis), and Chlamydia trachomatis. Symptoms include bloody and mucoid discharge, anal pain and fever. Differentials for non infectious causes include IBD, ischemic colitis and non-steroidal anti-inflammatory drug enteropathy. Assessment of these conditions should involve standard diagnostic measures such as anoscopy or sigmoidoscopy, stool analysis for white blood cells, and microbiological testing—including evaluations for gonorrhea, chlamydia (with LGV PCR when accessible), herpes simplex via NAAT, and syphilis serology. It is imperative to diagnose STI related proctitis early to avoid complications from lymphatic spread leading to abscesses, granulomas, and fistulas. We want to emphasize the importance of STI among the differentials for proctitis, as it can avoid further diagnostic imaging and invasive procedures.
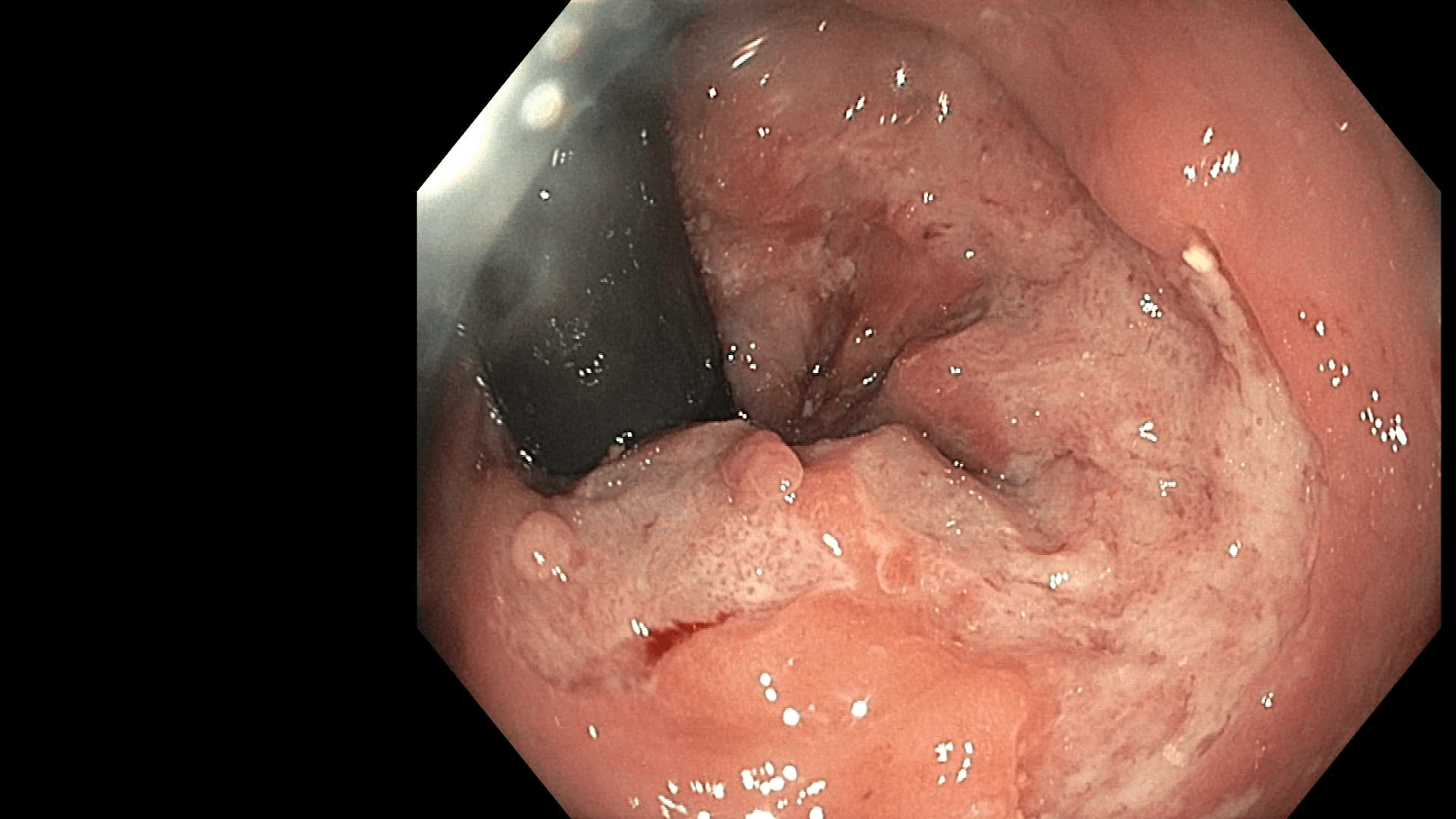
Figure: Figure 1
Disclosures:
Charitha Karanam Ramapathy indicated no relevant financial relationships.
Mahmoud Aryan indicated no relevant financial relationships.
Kirk Russ indicated no relevant financial relationships.
Charitha Karanam Ramapathy, MD1, Mahmoud Aryan, MD2, Kirk Russ, MD2. P3455 - Proctitis Secondary to <i>Chlamydia Trachomatis</i> Infection: A Diagnostic Challenge in Anorectal Pathology, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
