Monday Poster Session
Category: Infections and Microbiome
P3440 - Exploring the Association Between Proton Pump Inhibitor Use and Elevated Rates of Ventilator-Associated Pneumonia in ICU Patients: Insights From the MIMIC-IV Database
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anjali Rajagopal, MBBS
University of Connecticut
Hartford, CT
Presenting Author(s)
Saurav Kini, MBBS1, Anjali Rajagopal, MBBS2, Rohit Khullar, MD1, Simardeep Singh, MBBS3, Raffi Karagozian, MD4
1Tufts Medical Center, Boston, MA; 2University of Connecticut, Hartford, CT; 3MedStar Georgetown University Hospital, Baltimore, MD; 4Tufts University School of Medicine, Boston, MA
Introduction: PPIs are commonly used in critically ill patients for stress ulcer prophylaxis. By decreasing gastric acidity, they predispose patients to nosocomial infections such as Ventilator Associated Pneumonia (VAP), linked to significant morbidity and mortality. While prior randomized trials have explored this, real-world ICU data are limited. Using the MIMIC-IV ICU database, we evaluated whether early or prolonged PPI exposure was associated with increased VAP incidence in mechanically ventilated ICU patients.
Methods: A retrospective cohort analysis was conducted in adult (≥18 years) ICU patients intubated for ≥48 hours (n=10,864) using the MIMIC IV database (2008-2019; 85,242 unique admissions). Patients with ICU stay less than 48 hours were excluded. Primary exposure was early PPI use, defined as administration of a PPI within the first 48 hours of ICU admission. Comparison groups studied were early H2 receptor antagonist (H2RA) use, no acid-suppressive therapy, and straitification based on duration of PPI administration. The primary outcome was the incidence of VAP, identified by ICD codes. Incidence of VAP was controlled for by duration of mechanical ventilation. Comparisons between categorical variables were performed using ꭓ2 contingency testing with α = 0.05.
Results: Among 10,865 ICU patients, early PPI use was associated with increased VAP incidence in those ventilated < 7 days (12.7% vs. 9.6%, p < 0.001), but not in those ventilated ≥7 days (36.6% vs. 33.0%, p = 0.06). VAP incidence also increased with prolonged PPI use during and prior to ICU admission. In patients ventilated < 7 days, VAP rates increased from 8.9% (no PPI) to 16.7% ( >2 weeks of PPI). Among those ventilated ≥7 days, VAP incidence ranged from 31.6% (no PPI) to 41.6% with >2 weeks of PPI exposure (p < 0.001).
Discussion: Both early and prolonged PPI use were associated with increased incidence of VAP particularly among patients ventilated for less than 7 days. These findings highlight the need to assess judicious use of acid suppression in all ICU patients. This study captures prescribing patterns, and suggests that variation in exposure, timing, duration, and indication could increase infection incidence in lower-risk patients. Confounding by indication or illness severity cannot be excluded. Future directions include multivariable modeling and propensity-matched analysis to clarify whether PPI use independently contributes to VAP risk.
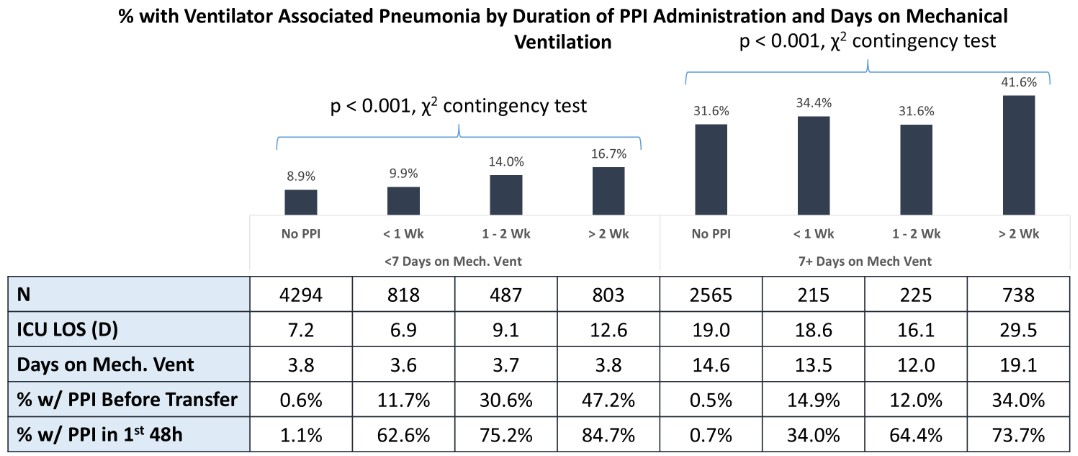
Figure: Adjusting for duration of mechanical ventilation, the rate of VAP prolonged use of PPIs during or prior to initiation of mechanical ventilation, up to 16.7% for patients with < 7 days and 41.6% for patients with 7 + days receiving ventilation and >2 weeks of PPI
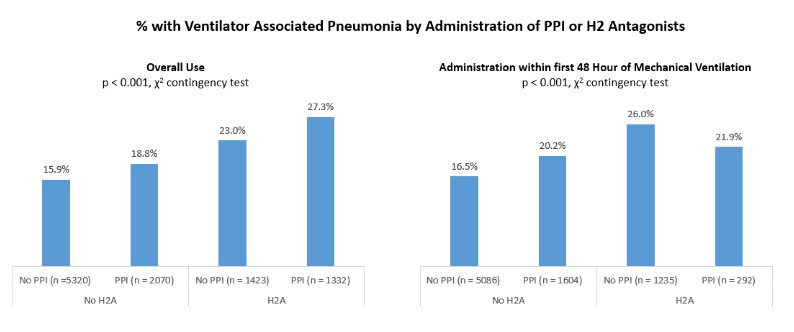
Figure: The rate of VAP increases with both use of PPIs and H2B among patients intubated for at least 48 hours.
Disclosures:
Saurav Kini indicated no relevant financial relationships.
Anjali Rajagopal indicated no relevant financial relationships.
Rohit Khullar indicated no relevant financial relationships.
Simardeep Singh indicated no relevant financial relationships.
Raffi Karagozian indicated no relevant financial relationships.
Saurav Kini, MBBS1, Anjali Rajagopal, MBBS2, Rohit Khullar, MD1, Simardeep Singh, MBBS3, Raffi Karagozian, MD4. P3440 - Exploring the Association Between Proton Pump Inhibitor Use and Elevated Rates of Ventilator-Associated Pneumonia in ICU Patients: Insights From the MIMIC-IV Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Tufts Medical Center, Boston, MA; 2University of Connecticut, Hartford, CT; 3MedStar Georgetown University Hospital, Baltimore, MD; 4Tufts University School of Medicine, Boston, MA
Introduction: PPIs are commonly used in critically ill patients for stress ulcer prophylaxis. By decreasing gastric acidity, they predispose patients to nosocomial infections such as Ventilator Associated Pneumonia (VAP), linked to significant morbidity and mortality. While prior randomized trials have explored this, real-world ICU data are limited. Using the MIMIC-IV ICU database, we evaluated whether early or prolonged PPI exposure was associated with increased VAP incidence in mechanically ventilated ICU patients.
Methods: A retrospective cohort analysis was conducted in adult (≥18 years) ICU patients intubated for ≥48 hours (n=10,864) using the MIMIC IV database (2008-2019; 85,242 unique admissions). Patients with ICU stay less than 48 hours were excluded. Primary exposure was early PPI use, defined as administration of a PPI within the first 48 hours of ICU admission. Comparison groups studied were early H2 receptor antagonist (H2RA) use, no acid-suppressive therapy, and straitification based on duration of PPI administration. The primary outcome was the incidence of VAP, identified by ICD codes. Incidence of VAP was controlled for by duration of mechanical ventilation. Comparisons between categorical variables were performed using ꭓ2 contingency testing with α = 0.05.
Results: Among 10,865 ICU patients, early PPI use was associated with increased VAP incidence in those ventilated < 7 days (12.7% vs. 9.6%, p < 0.001), but not in those ventilated ≥7 days (36.6% vs. 33.0%, p = 0.06). VAP incidence also increased with prolonged PPI use during and prior to ICU admission. In patients ventilated < 7 days, VAP rates increased from 8.9% (no PPI) to 16.7% ( >2 weeks of PPI). Among those ventilated ≥7 days, VAP incidence ranged from 31.6% (no PPI) to 41.6% with >2 weeks of PPI exposure (p < 0.001).
Discussion: Both early and prolonged PPI use were associated with increased incidence of VAP particularly among patients ventilated for less than 7 days. These findings highlight the need to assess judicious use of acid suppression in all ICU patients. This study captures prescribing patterns, and suggests that variation in exposure, timing, duration, and indication could increase infection incidence in lower-risk patients. Confounding by indication or illness severity cannot be excluded. Future directions include multivariable modeling and propensity-matched analysis to clarify whether PPI use independently contributes to VAP risk.
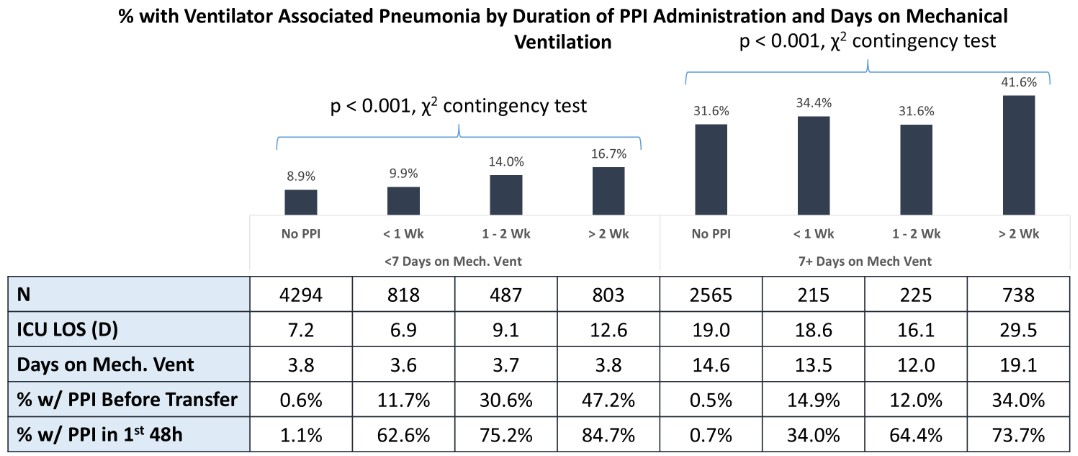
Figure: Adjusting for duration of mechanical ventilation, the rate of VAP prolonged use of PPIs during or prior to initiation of mechanical ventilation, up to 16.7% for patients with < 7 days and 41.6% for patients with 7 + days receiving ventilation and >2 weeks of PPI
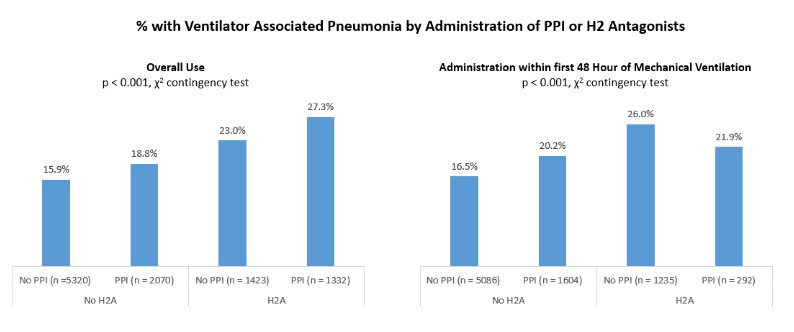
Figure: The rate of VAP increases with both use of PPIs and H2B among patients intubated for at least 48 hours.
Disclosures:
Saurav Kini indicated no relevant financial relationships.
Anjali Rajagopal indicated no relevant financial relationships.
Rohit Khullar indicated no relevant financial relationships.
Simardeep Singh indicated no relevant financial relationships.
Raffi Karagozian indicated no relevant financial relationships.
Saurav Kini, MBBS1, Anjali Rajagopal, MBBS2, Rohit Khullar, MD1, Simardeep Singh, MBBS3, Raffi Karagozian, MD4. P3440 - Exploring the Association Between Proton Pump Inhibitor Use and Elevated Rates of Ventilator-Associated Pneumonia in ICU Patients: Insights From the MIMIC-IV Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
