Monday Poster Session
Category: Interventional Endoscopy
P3524 - Utilizing Machine Learning to Identify Predictors of Post-ERCP Pancreatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jason Erno, MD
University of Virginia Medical Center
Charlottesville, VA
Presenting Author(s)
Jason Erno, MD1, Kathryn Linehan, PhD2, Angela B. Danquah, MS2, Alexander Podboy, MD3
1University of Virginia Medical Center, Charlottesville, VA; 2University of Virginia, Charlottesville, VA; 3University of Virginia Health, Charlottesville, VA
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is an essential diagnostic and therapeutic procedure, but carries a notable risk of complications, including post-ERCP pancreatitis (PEP). Identifying predictors of PEP can aid in patient selection and the implementation of preventative strategies to optimize outcomes. Machine learning (ML) algorithms offer promise for predictive analytics in healthcare. Several recent studies have aimed to develop predictive models to assess pre-procedural PEP risk. However, their performance in predicting PEP has been limited. This study evaluates the utility of ML models alongside sensitivity-specificity analyses to enhance prediction accuracy and determine feature importance.
Methods: This single-center retrospective study analyzed adults who underwent ERCP with native papilla over 5 years. Data collected included comorbidities, sphincterotomy performed, stenting performed, fluoroscopic time required, fellow involvement and types of cannulation performed. PEP was defined as new or worsened abdominal pain with lipase three times the upper limit of normal more than 24 hours but less than 7 days after ERCP. ML analyses were performed on the entire dataset and two additional subsets: patients with and without a history of acute and/or chronic pancreatitis.
Results: A total of 1469 patients were included in the study with 120 experiencing PEP. Most patients did not have a history of acute pancreatitis (27.6%) or chronic pancreatitis (16.5%). A LASSO logistic regression incorporating all cannulation and stent variables identified several significant predictors: higher BMI, CKD, dyslipidemia and enoxaparin use. Otherwise, procedures classified as “not difficult” by the provider and fellow involvement were protective. In separate models optimizing sensitivity and specificity of PEP in all patients, the top features were body mass index (BMI), age, total fluoroscopy time and history of acute pancreatitis. In sensitivity-specificity models in patients without a history of acute or chronic pancreatitis, total fluoroscopy time was consistently the highest predictor with age, BMI and biliary pull type sphincterotomy often following.
Discussion: Feature importance analysis underscores key risk factors for PEP development, providing potential targets for future predictive and preventive strategies. These findings highlight the need for further optimization of ML approaches and their integration with clinical workflows.
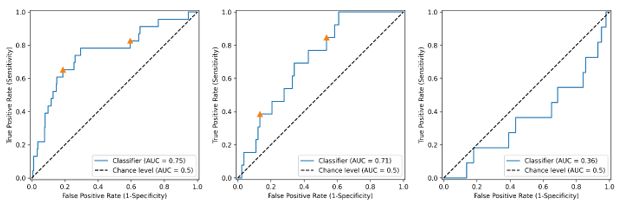
Figure: Demographic data
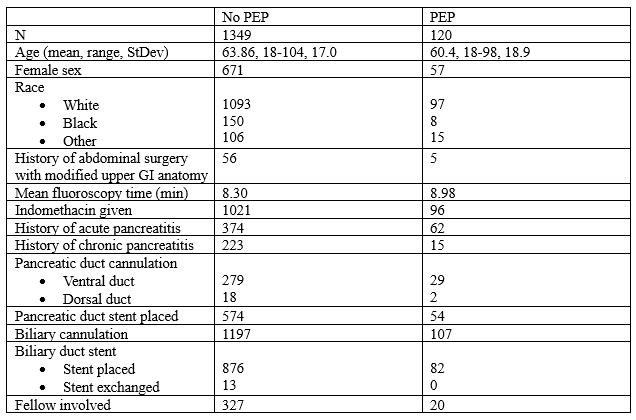
Figure: ROC curves for random forest models of all patients (left), patients with a history of acute or chronic pancreatitis (middle), and patients without a history of acute or chronic pancreatitis (right)
Disclosures:
Jason Erno indicated no relevant financial relationships.
Kathryn Linehan indicated no relevant financial relationships.
Angela Danquah indicated no relevant financial relationships.
Alexander Podboy indicated no relevant financial relationships.
Jason Erno, MD1, Kathryn Linehan, PhD2, Angela B. Danquah, MS2, Alexander Podboy, MD3. P3524 - Utilizing Machine Learning to Identify Predictors of Post-ERCP Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Virginia Medical Center, Charlottesville, VA; 2University of Virginia, Charlottesville, VA; 3University of Virginia Health, Charlottesville, VA
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is an essential diagnostic and therapeutic procedure, but carries a notable risk of complications, including post-ERCP pancreatitis (PEP). Identifying predictors of PEP can aid in patient selection and the implementation of preventative strategies to optimize outcomes. Machine learning (ML) algorithms offer promise for predictive analytics in healthcare. Several recent studies have aimed to develop predictive models to assess pre-procedural PEP risk. However, their performance in predicting PEP has been limited. This study evaluates the utility of ML models alongside sensitivity-specificity analyses to enhance prediction accuracy and determine feature importance.
Methods: This single-center retrospective study analyzed adults who underwent ERCP with native papilla over 5 years. Data collected included comorbidities, sphincterotomy performed, stenting performed, fluoroscopic time required, fellow involvement and types of cannulation performed. PEP was defined as new or worsened abdominal pain with lipase three times the upper limit of normal more than 24 hours but less than 7 days after ERCP. ML analyses were performed on the entire dataset and two additional subsets: patients with and without a history of acute and/or chronic pancreatitis.
Results: A total of 1469 patients were included in the study with 120 experiencing PEP. Most patients did not have a history of acute pancreatitis (27.6%) or chronic pancreatitis (16.5%). A LASSO logistic regression incorporating all cannulation and stent variables identified several significant predictors: higher BMI, CKD, dyslipidemia and enoxaparin use. Otherwise, procedures classified as “not difficult” by the provider and fellow involvement were protective. In separate models optimizing sensitivity and specificity of PEP in all patients, the top features were body mass index (BMI), age, total fluoroscopy time and history of acute pancreatitis. In sensitivity-specificity models in patients without a history of acute or chronic pancreatitis, total fluoroscopy time was consistently the highest predictor with age, BMI and biliary pull type sphincterotomy often following.
Discussion: Feature importance analysis underscores key risk factors for PEP development, providing potential targets for future predictive and preventive strategies. These findings highlight the need for further optimization of ML approaches and their integration with clinical workflows.
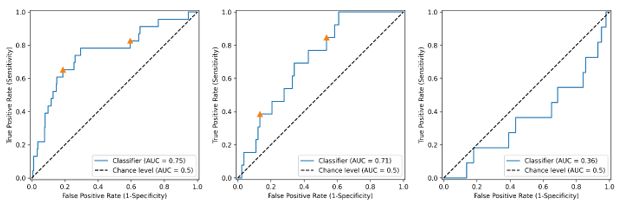
Figure: Demographic data
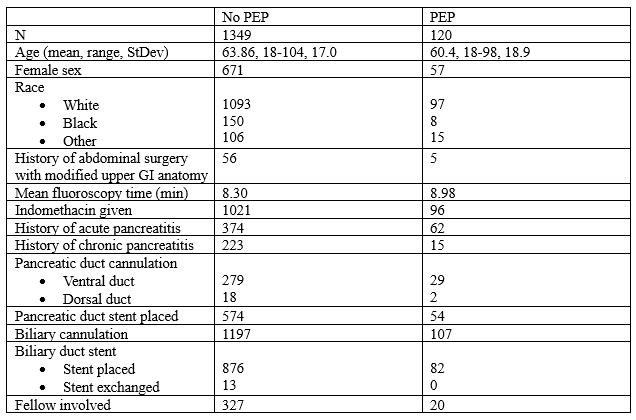
Figure: ROC curves for random forest models of all patients (left), patients with a history of acute or chronic pancreatitis (middle), and patients without a history of acute or chronic pancreatitis (right)
Disclosures:
Jason Erno indicated no relevant financial relationships.
Kathryn Linehan indicated no relevant financial relationships.
Angela Danquah indicated no relevant financial relationships.
Alexander Podboy indicated no relevant financial relationships.
Jason Erno, MD1, Kathryn Linehan, PhD2, Angela B. Danquah, MS2, Alexander Podboy, MD3. P3524 - Utilizing Machine Learning to Identify Predictors of Post-ERCP Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
