Monday Poster Session
Category: Interventional Endoscopy
P3510 - Role of POEM and Heller’s Myotomy Against Esophageal Cancer in Patients With Achalasia: A Multi-Center Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ashujot K. Dang, MD
University of California Riverside School of Medicine
Riverside, CA
Presenting Author(s)
Ashujot K. Dang, MD1, Shivam Kalra, MBBS, MHA2, Saranya Arumugam, MD1, Banreet Dhindsa, MD3, Amaninder Dhaliwal, MD4
1University of California Riverside School of Medicine, Riverside, CA; 2Trident Medical Center, North Charleston, SC; 3Brown University / Rhode Island Hospital, East Providence, RI; 4University of South Carolina School of Medicine, Florence, SC
Introduction: Achalasia, an esophageal motility disorder, is a known risk factor for the development of esophageal cancer (EC). Peroral Endoscopic Myotomy (POEM) and Laparoscopic Heller Myotomy (LHM) are both established treatments for Achalasia. However, the incidence of EC post-myotomy has always been an area of concern, with very limited large-scale studies. This multicentric study aims to compare the incidence of EC in patients treated with POEM or LHM vs patients who are left untreated.
Methods: We queried a retrospective cohort analysis using TrinetX US collaborative network, encompassing medical records from over 69 US healthcare organizations. We identified 7,458 achalasia patients who underwent POEM or LHM (Procedure Group) and 54,825 who did not (Control Group). Propensity score matching (1:1 ratio) was performed based on age, sex, race, and relevant comorbidities (GERD, Barrett's esophagus, tobacco/alcohol use), resulting in 7,372 patients in each cohort. We assessed the primary outcome, which was the incidence of EC (ICD-10 C15 codes). Statistical analysis included descriptive statistics, t-tests, chi-square tests, Kaplan-Meier survival analysis with log-rank test, and Cox proportional hazards regression.
Results: After exclusions for prior EC diagnosis, the Procedure Group included 7,351 patients, and the Control Group had 7,313 patients for outcome analysis. The incidence of EC was 0.4% (32 patients) in the Procedure Group and 0.8% (57 patients) in the Control Group. Risk analysis showed the Procedure Group had a significantly lower risk of developing EC (risk difference: -0.003; p = 0.007). Kaplan-Meier analysis showed improved esophageal cancer-free survival in the Procedure Group (survival probability 96.79% vs. 96.21%; log rank p=0.077). Cox proportional hazard analysis indicated a lower hazard ratio for EC in the Procedure Group (HR: 0.676; 95% CI: 0.437, 1.046; p = 0.000).
Discussion: Our study shows that achalasia patients treated with POEM or LHM have a significantly lower incidence of esophageal carcinoma compared to untreated patients. While both groups are at risk, these interventions appear to offer a protective effect. Given the increased prevalence of post-procedure epithelial changes and the established risk factors (smoking, alcohol abuse, older age, advanced achalasia subtypes), long-term surveillance is warranted to prevent EC. Further research on the role of acid suppression therapies and periodic endoscopies with biopsies is encouraged.
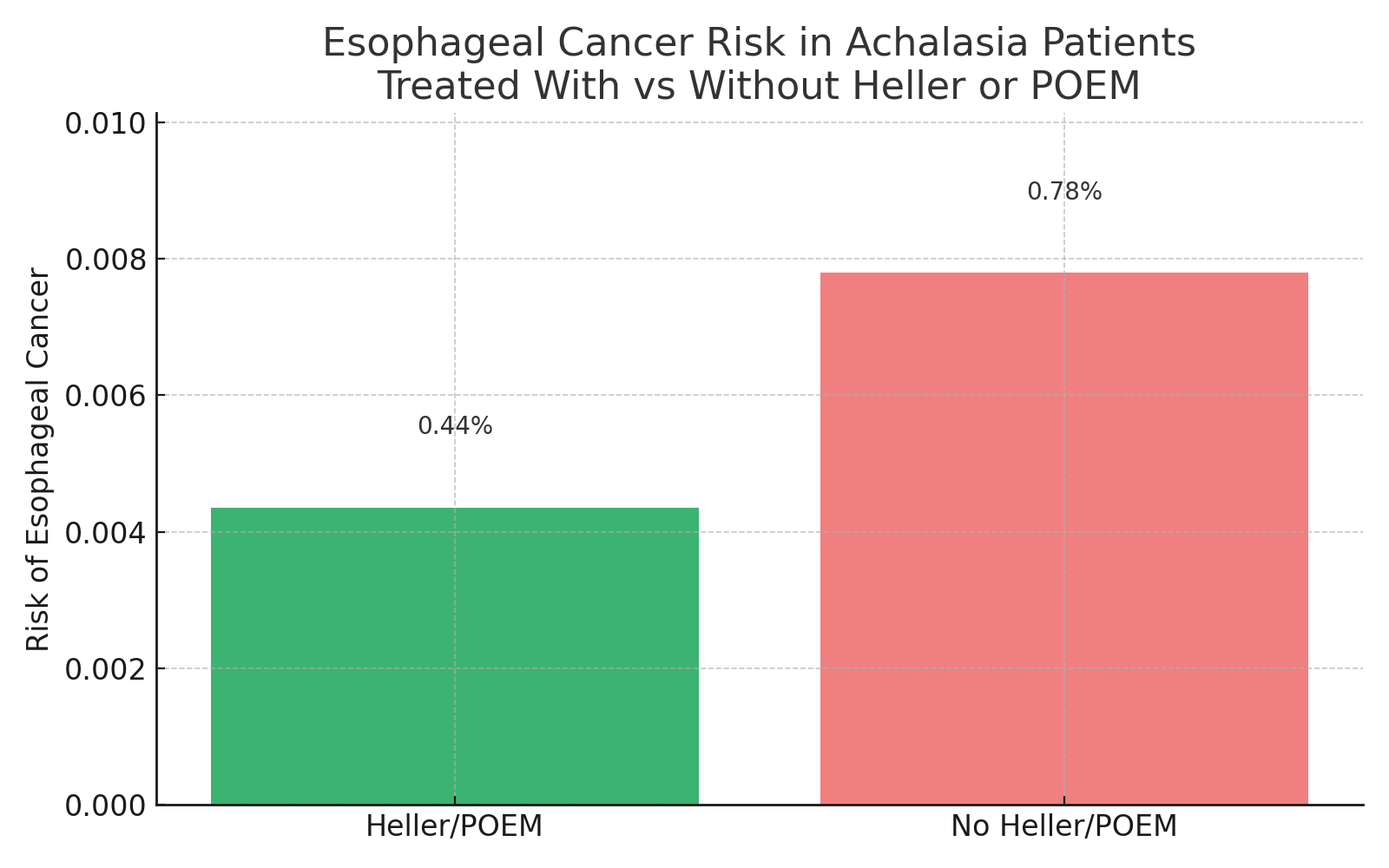
Figure: Figure depicted the risk of esophageal cancer risk in achalsia patients trested with and without Heller or POEM
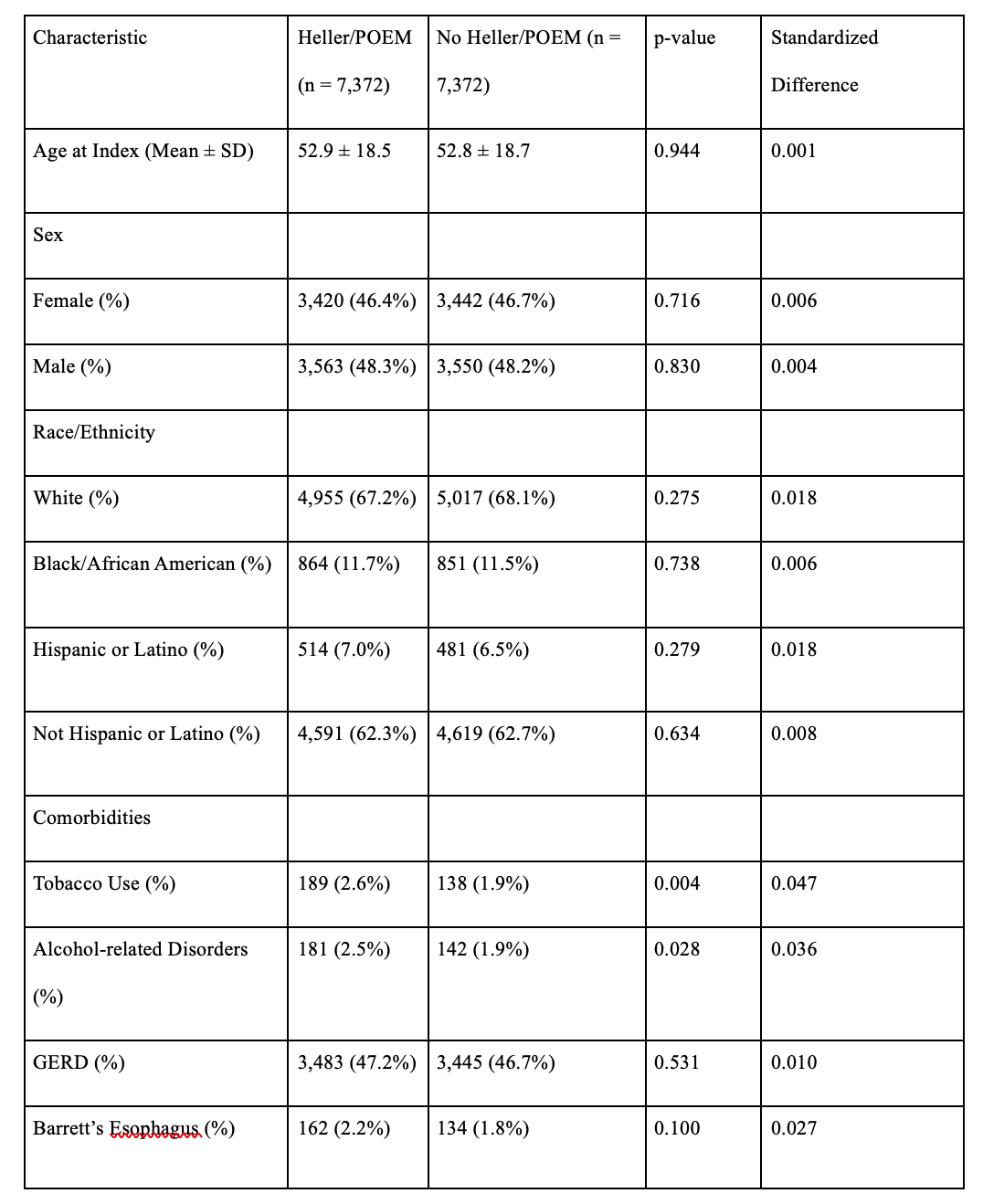
Figure: Table with each outcome risk and comparison between the two groups: Heller/POEM vs no Heller/POEM
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Shivam Kalra indicated no relevant financial relationships.
Saranya Arumugam indicated no relevant financial relationships.
Banreet Dhindsa indicated no relevant financial relationships.
Amaninder Dhaliwal indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Shivam Kalra, MBBS, MHA2, Saranya Arumugam, MD1, Banreet Dhindsa, MD3, Amaninder Dhaliwal, MD4. P3510 - Role of POEM and Heller’s Myotomy Against Esophageal Cancer in Patients With Achalasia: A Multi-Center Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Riverside School of Medicine, Riverside, CA; 2Trident Medical Center, North Charleston, SC; 3Brown University / Rhode Island Hospital, East Providence, RI; 4University of South Carolina School of Medicine, Florence, SC
Introduction: Achalasia, an esophageal motility disorder, is a known risk factor for the development of esophageal cancer (EC). Peroral Endoscopic Myotomy (POEM) and Laparoscopic Heller Myotomy (LHM) are both established treatments for Achalasia. However, the incidence of EC post-myotomy has always been an area of concern, with very limited large-scale studies. This multicentric study aims to compare the incidence of EC in patients treated with POEM or LHM vs patients who are left untreated.
Methods: We queried a retrospective cohort analysis using TrinetX US collaborative network, encompassing medical records from over 69 US healthcare organizations. We identified 7,458 achalasia patients who underwent POEM or LHM (Procedure Group) and 54,825 who did not (Control Group). Propensity score matching (1:1 ratio) was performed based on age, sex, race, and relevant comorbidities (GERD, Barrett's esophagus, tobacco/alcohol use), resulting in 7,372 patients in each cohort. We assessed the primary outcome, which was the incidence of EC (ICD-10 C15 codes). Statistical analysis included descriptive statistics, t-tests, chi-square tests, Kaplan-Meier survival analysis with log-rank test, and Cox proportional hazards regression.
Results: After exclusions for prior EC diagnosis, the Procedure Group included 7,351 patients, and the Control Group had 7,313 patients for outcome analysis. The incidence of EC was 0.4% (32 patients) in the Procedure Group and 0.8% (57 patients) in the Control Group. Risk analysis showed the Procedure Group had a significantly lower risk of developing EC (risk difference: -0.003; p = 0.007). Kaplan-Meier analysis showed improved esophageal cancer-free survival in the Procedure Group (survival probability 96.79% vs. 96.21%; log rank p=0.077). Cox proportional hazard analysis indicated a lower hazard ratio for EC in the Procedure Group (HR: 0.676; 95% CI: 0.437, 1.046; p = 0.000).
Discussion: Our study shows that achalasia patients treated with POEM or LHM have a significantly lower incidence of esophageal carcinoma compared to untreated patients. While both groups are at risk, these interventions appear to offer a protective effect. Given the increased prevalence of post-procedure epithelial changes and the established risk factors (smoking, alcohol abuse, older age, advanced achalasia subtypes), long-term surveillance is warranted to prevent EC. Further research on the role of acid suppression therapies and periodic endoscopies with biopsies is encouraged.
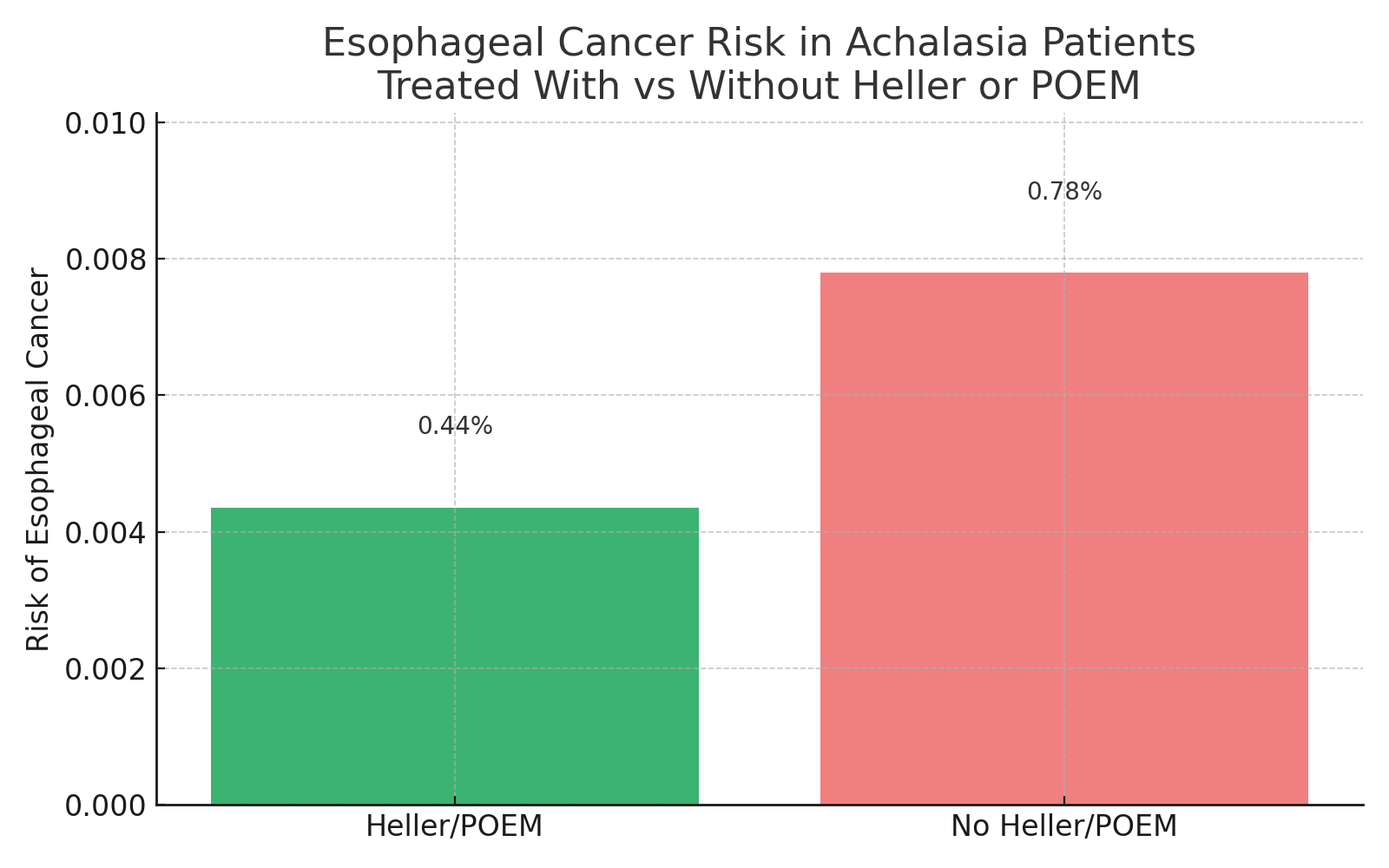
Figure: Figure depicted the risk of esophageal cancer risk in achalsia patients trested with and without Heller or POEM
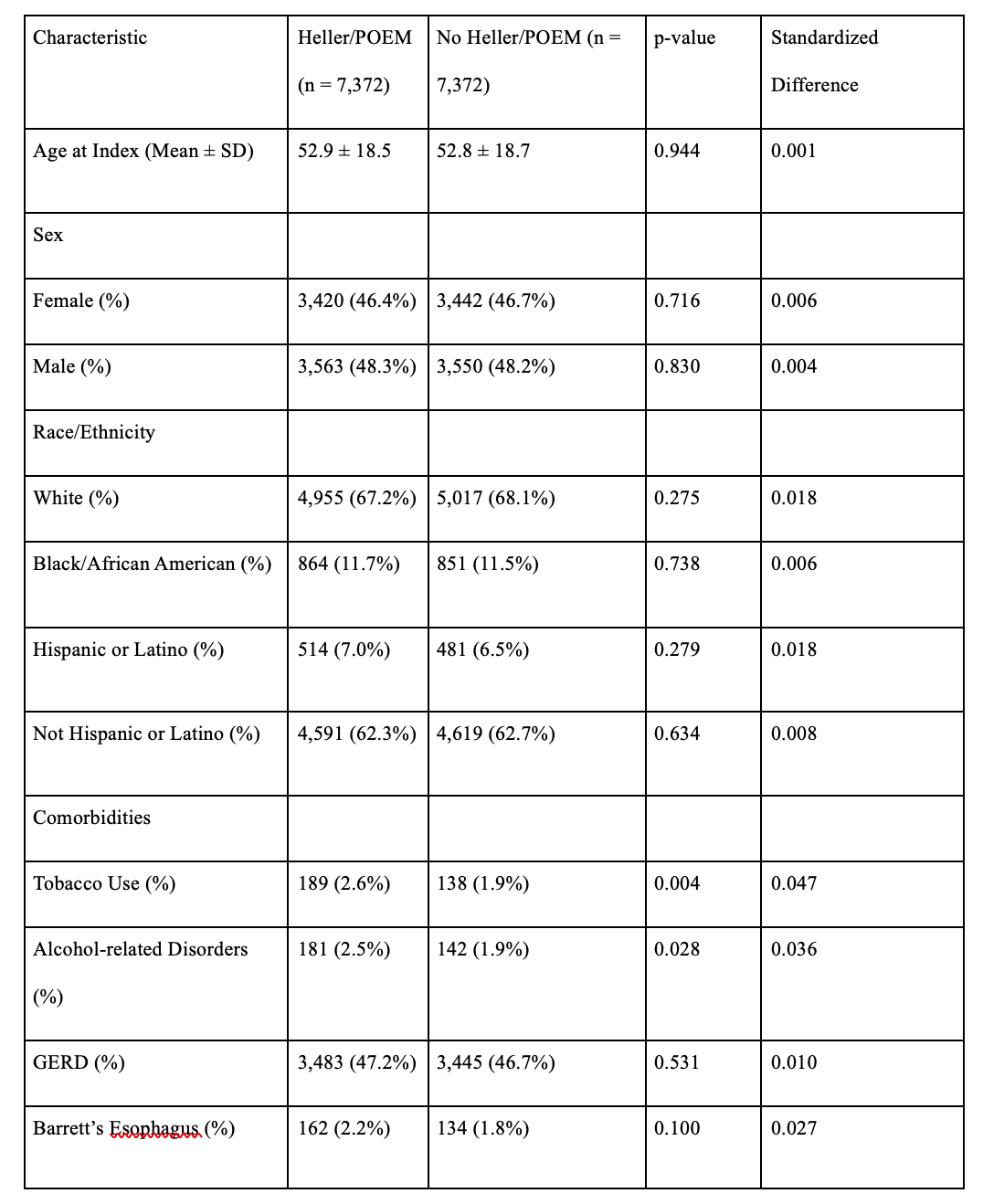
Figure: Table with each outcome risk and comparison between the two groups: Heller/POEM vs no Heller/POEM
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Shivam Kalra indicated no relevant financial relationships.
Saranya Arumugam indicated no relevant financial relationships.
Banreet Dhindsa indicated no relevant financial relationships.
Amaninder Dhaliwal indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Shivam Kalra, MBBS, MHA2, Saranya Arumugam, MD1, Banreet Dhindsa, MD3, Amaninder Dhaliwal, MD4. P3510 - Role of POEM and Heller’s Myotomy Against Esophageal Cancer in Patients With Achalasia: A Multi-Center Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
