Monday Poster Session
Category: Interventional Endoscopy
P3585 - Thinking Outside the Band: Coagulation Grasper as Salvage Therapy in Post-Banding Ulcer Hemorrhage
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nourhan Saleh, MD
University of Missouri Health Care
Columbia, MO
Presenting Author(s)
Nourhan Saleh, MD1, Eunice Aregbesola, MD2, Ibukunoluwa Oshobu, MD, MPH1, Mahmoud Mansour, MD1, Darian Fard, MD1, Robert Harris, MD1
1University of Missouri Health Care, Columbia, MO; 2University of Missouri, Columbia, Columbia, MO
Introduction: Post-banding ulcer bleeding (PBUB) occurs in 3–10% of patients following endoscopic variceal ligation (EVL), typically 10–14 days post-procedure. Though often less severe than primary variceal hemorrhage, PBUB can be life-threatening. Management includes repeat banding, injection therapies, balloon tamponade, and rescue interventions such as transjugular intrahepatic portosystemic shunt (TIPS). We present a case of severe PBUB successfully managed with coagulation grasper therapy as a bridge to TIPS.
Case Description/
Methods: A 33-year-old male with decompensated cirrhosis and alcohol use disorder (abstinent for 1.5 years) presented with hematemesis. Labs showed hemoglobin 7.8 g/dL, platelets 129 × 10⁹/L, INR 1.5, MELD 16. He had recurrent variceal bleeds requiring multiple EVLs, most recently with 7 bands placed 2 weeks prior.
Endoscopy revealed an actively bleeding post-banding ulcer in the distal esophagus with rupture of the variceal wall, suggesting incomplete obliteration of the variceal lumen.
Multiple hemostatic attempts failed. Three additional bands placed distally did not control bleeding. Direct banding at the site was unsuccessful due to surrounding scar tissue. Epinephrine injection failed. A 20 mm CRE balloon tamponade provided only transient relief. The patient remained unstable with ongoing hemorrhage, requiring hemostasis before TIPS could be performed. A Blakemore tube was unavailable. Using a distal cap for enhanced visualization, a coagulation grasper was used to directly grasp the bleeding varix, and soft coagulation was applied, achieving hemostasis and stabilizing the patient for TIPS.
Discussion: This case highlights key points about PBUB. The bleeding occurred 14 days post-EVL, during the period when ulcer scabs slough and newly formed vessels are exposed but not yet healed. The rupture in the variceal wall represented a persistent variceal lumen rather than bleeding from granulation tissue, indicating incomplete thrombosis despite prior band placement.
Literature for coaptive therapy in PBUB is limited, with no published reports describing use of coagulation graspers for this indication. In this case, direct soft coagulation to a clearly visualized bleeding site proved effective. This technique represents a novel adjunct in managing refractory PBUB, especially when the bleeding source involves a persistent variceal channel. It also underscores the importance of having multiple therapeutic tools available to address complex and potentially fatal post-EVL complications.
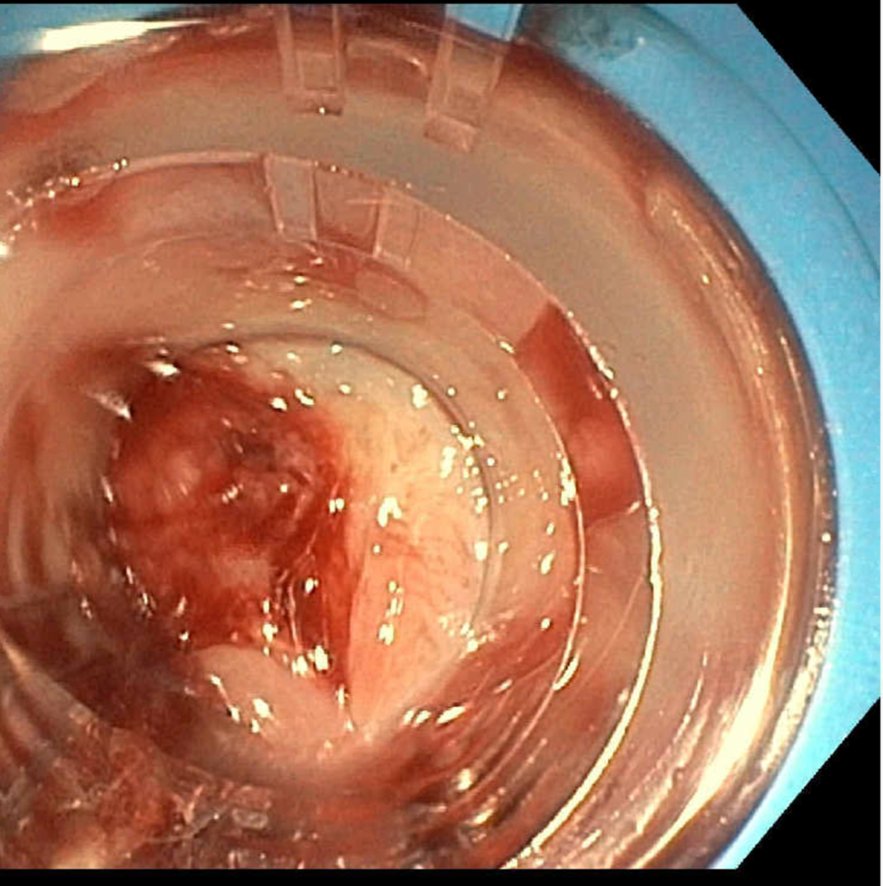
Figure: Figure 1: Post-banding ulcer hemorrhage with cap tamponade. Endoscopic view of a bleeding variceal wall within a post-EVL ulcer. The transparent cap provides temporary pressure control and visualization of the bleeding source prior to successful coagulation grasper therapy.

Figure: Figure 2: Post-coaptive therapy hemostasis. Endoscopic view following successful coagulation grasper application. Note the variceal engorgement after treatment, suggesting blood containment within the vessel rather than extravasation through the previously visible defect.
Disclosures:
Nourhan Saleh indicated no relevant financial relationships.
Eunice Aregbesola indicated no relevant financial relationships.
Ibukunoluwa Oshobu indicated no relevant financial relationships.
Mahmoud Mansour indicated no relevant financial relationships.
Darian Fard indicated no relevant financial relationships.
Robert Harris indicated no relevant financial relationships.
Nourhan Saleh, MD1, Eunice Aregbesola, MD2, Ibukunoluwa Oshobu, MD, MPH1, Mahmoud Mansour, MD1, Darian Fard, MD1, Robert Harris, MD1. P3585 - Thinking Outside the Band: Coagulation Grasper as Salvage Therapy in Post-Banding Ulcer Hemorrhage, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Missouri Health Care, Columbia, MO; 2University of Missouri, Columbia, Columbia, MO
Introduction: Post-banding ulcer bleeding (PBUB) occurs in 3–10% of patients following endoscopic variceal ligation (EVL), typically 10–14 days post-procedure. Though often less severe than primary variceal hemorrhage, PBUB can be life-threatening. Management includes repeat banding, injection therapies, balloon tamponade, and rescue interventions such as transjugular intrahepatic portosystemic shunt (TIPS). We present a case of severe PBUB successfully managed with coagulation grasper therapy as a bridge to TIPS.
Case Description/
Methods: A 33-year-old male with decompensated cirrhosis and alcohol use disorder (abstinent for 1.5 years) presented with hematemesis. Labs showed hemoglobin 7.8 g/dL, platelets 129 × 10⁹/L, INR 1.5, MELD 16. He had recurrent variceal bleeds requiring multiple EVLs, most recently with 7 bands placed 2 weeks prior.
Endoscopy revealed an actively bleeding post-banding ulcer in the distal esophagus with rupture of the variceal wall, suggesting incomplete obliteration of the variceal lumen.
Multiple hemostatic attempts failed. Three additional bands placed distally did not control bleeding. Direct banding at the site was unsuccessful due to surrounding scar tissue. Epinephrine injection failed. A 20 mm CRE balloon tamponade provided only transient relief. The patient remained unstable with ongoing hemorrhage, requiring hemostasis before TIPS could be performed. A Blakemore tube was unavailable. Using a distal cap for enhanced visualization, a coagulation grasper was used to directly grasp the bleeding varix, and soft coagulation was applied, achieving hemostasis and stabilizing the patient for TIPS.
Discussion: This case highlights key points about PBUB. The bleeding occurred 14 days post-EVL, during the period when ulcer scabs slough and newly formed vessels are exposed but not yet healed. The rupture in the variceal wall represented a persistent variceal lumen rather than bleeding from granulation tissue, indicating incomplete thrombosis despite prior band placement.
Literature for coaptive therapy in PBUB is limited, with no published reports describing use of coagulation graspers for this indication. In this case, direct soft coagulation to a clearly visualized bleeding site proved effective. This technique represents a novel adjunct in managing refractory PBUB, especially when the bleeding source involves a persistent variceal channel. It also underscores the importance of having multiple therapeutic tools available to address complex and potentially fatal post-EVL complications.
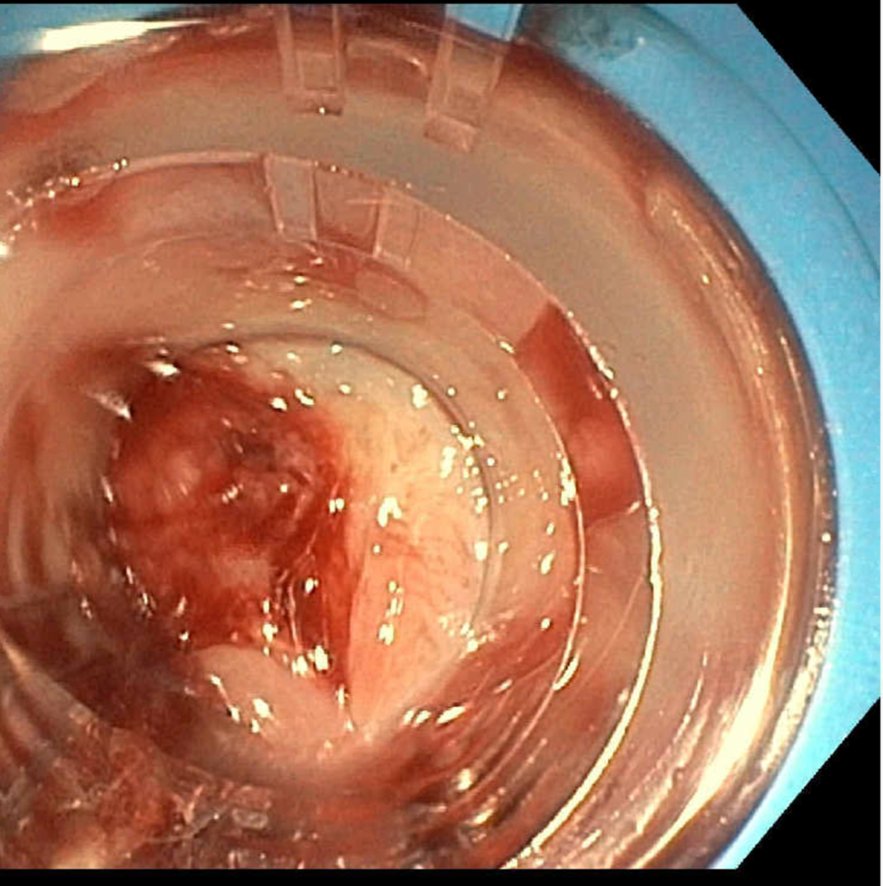
Figure: Figure 1: Post-banding ulcer hemorrhage with cap tamponade. Endoscopic view of a bleeding variceal wall within a post-EVL ulcer. The transparent cap provides temporary pressure control and visualization of the bleeding source prior to successful coagulation grasper therapy.

Figure: Figure 2: Post-coaptive therapy hemostasis. Endoscopic view following successful coagulation grasper application. Note the variceal engorgement after treatment, suggesting blood containment within the vessel rather than extravasation through the previously visible defect.
Disclosures:
Nourhan Saleh indicated no relevant financial relationships.
Eunice Aregbesola indicated no relevant financial relationships.
Ibukunoluwa Oshobu indicated no relevant financial relationships.
Mahmoud Mansour indicated no relevant financial relationships.
Darian Fard indicated no relevant financial relationships.
Robert Harris indicated no relevant financial relationships.
Nourhan Saleh, MD1, Eunice Aregbesola, MD2, Ibukunoluwa Oshobu, MD, MPH1, Mahmoud Mansour, MD1, Darian Fard, MD1, Robert Harris, MD1. P3585 - Thinking Outside the Band: Coagulation Grasper as Salvage Therapy in Post-Banding Ulcer Hemorrhage, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
