Monday Poster Session
Category: Interventional Endoscopy
P3578 - Hemostasis With Fully Covered Self-Expanding Bare Metal Stent as a Bridge to Liver Transplantation in a Patient With Acute Liver Injury and Hemodynamically Unstable Hemobilia
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anneleise Frie, MD
University of Wisconsin Hospitals and Clinics
Madison, WI
Presenting Author(s)
Anneleise Frie, MD1, Joshua Morny, MBChB2, Nimrod Deiss-Yehiely, MD3, Samuel Koebe, MD4, Michael Woods, MD4, Patrick Pfau, MD5
1University of Wisconsin Hospitals and Clinics, Madison, WI; 2William S. Middleton Memorial Veteran's Hospital, Madison, WI; 3University of Wisconsin Hospitals and Clinics, Department of Medicine, Division of Gastroenterology and Hepatology, Madison, WI; 4University of Wisconsin Hospitals and Clinics, Department of Radiology, Madison, WI; 5University of Wisconsin School of Medicine and Public Health, Madison, WI
Introduction: Hemobilia is an uncommon but important etiology of upper gastrointestinal bleeding presenting with jaundice, right upper quadrant abdominal pain and gastrointestinal hemorrhage. The source may be arterial or venous caused by iatrogenic, traumatic, neoplastic, inflammatory, infectious, and vascular etiologies. Rarely, hemobilia may occur due to portal hypertensive biliopathy secondary to varices in the bile duct.
Case Description/
Methods: A 49-year-old male presented with jaundice, abdominal pain and melena. He was admitted for acute liver injury secondary to alcoholic hepatitis complicated by portal hypertension, ascites with hepatorenal syndrome and portal venous thrombosis with a MELD score of 41. He was evaluated and listed for liver transplant. This was precluded by acute hematochezia and shock requiring multiple blood transfusions and vasopressor support. Upper endoscopy demonstrated hemobilia (Figure 1a). Labs were notable for hemoglobin 7.6, platelet count 49,000, and INR 2.3. Interventional Radiology was consulted for transcatheter arterial embolization (TAE), but non-invasive imaging supported variceal bleeding in the distal bile duct due to portal hypertensive biliopathy rather than arterial bleeding (Figure 2). A TIPS procedure was considered but determined to be too risky in the setting of his clinical instability. Endoscopic retrograde cholangiopancreatography (ERCP) was performed with placement of one fully covered self-expandable metal stent (FCSEMS) into the common bile duct, achieving hemostasis (Figure 1b) and clinical stability. He underwent liver transplantation with successful duct-to-duct biliary anastomosis. The stent was removed two days later without further hemobilia.
Discussion: Treatment goals in hemobilia are hemostasis and maintenance of bile flow. TAE is becoming the gold standard for treatment of persistent arterial hemobilia in hemodynamically unstable patients. Endoscopic biliary stent placement is the initial therapy for venous hemobilia in hemodynamically stable patients. TAE would have been therapeutically ineffective in our patient due to the venous source of bleeding. Moreover, given the presence of a thrombosed portal vein, TAE could have led to significant hepatic ischemia. Though palliative biliary stenting for portal biliopathy has been reported previously, the success of ERCP with FCSEMS in our patient highlights the use of FCSEMS as a bridge to liver transplantation in patients with hemodynamically unstable hemobilia secondary to portal biliopathy.
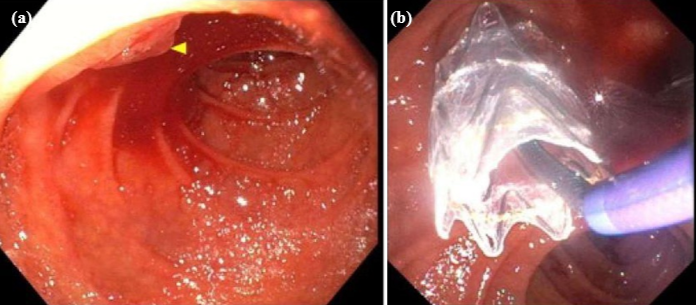
Figure: Figure 1. (a) Red blood in the second portion of the duodenum with bright red blood actively hemorrhaging from the papilla with washing, visualized during initial esophagogastroduodenoscopy. (b) Placement of one 10mm x 6cm fully covered self-expandable metal stent 4cm into the common bile duct, crossing the ampulla and papilla without sphincterotomy, during endoscopic retrograde cholangiopancreatography.
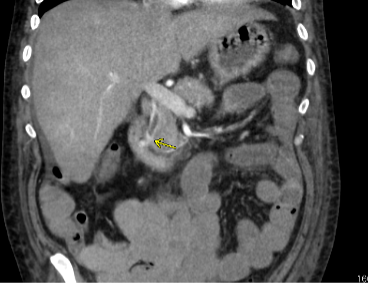
Figure: Figure 2. Computed tomography angiogram of the abdomen demonstrated hyper enhancement of the ampulla/papilla without active extravasation, consistent with biliary varices.
Disclosures:
Anneleise Frie indicated no relevant financial relationships.
Joshua Morny indicated no relevant financial relationships.
Nimrod Deiss-Yehiely indicated no relevant financial relationships.
Samuel Koebe indicated no relevant financial relationships.
Michael Woods indicated no relevant financial relationships.
Patrick Pfau indicated no relevant financial relationships.
Anneleise Frie, MD1, Joshua Morny, MBChB2, Nimrod Deiss-Yehiely, MD3, Samuel Koebe, MD4, Michael Woods, MD4, Patrick Pfau, MD5. P3578 - Hemostasis With Fully Covered Self-Expanding Bare Metal Stent as a Bridge to Liver Transplantation in a Patient With Acute Liver Injury and Hemodynamically Unstable Hemobilia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Wisconsin Hospitals and Clinics, Madison, WI; 2William S. Middleton Memorial Veteran's Hospital, Madison, WI; 3University of Wisconsin Hospitals and Clinics, Department of Medicine, Division of Gastroenterology and Hepatology, Madison, WI; 4University of Wisconsin Hospitals and Clinics, Department of Radiology, Madison, WI; 5University of Wisconsin School of Medicine and Public Health, Madison, WI
Introduction: Hemobilia is an uncommon but important etiology of upper gastrointestinal bleeding presenting with jaundice, right upper quadrant abdominal pain and gastrointestinal hemorrhage. The source may be arterial or venous caused by iatrogenic, traumatic, neoplastic, inflammatory, infectious, and vascular etiologies. Rarely, hemobilia may occur due to portal hypertensive biliopathy secondary to varices in the bile duct.
Case Description/
Methods: A 49-year-old male presented with jaundice, abdominal pain and melena. He was admitted for acute liver injury secondary to alcoholic hepatitis complicated by portal hypertension, ascites with hepatorenal syndrome and portal venous thrombosis with a MELD score of 41. He was evaluated and listed for liver transplant. This was precluded by acute hematochezia and shock requiring multiple blood transfusions and vasopressor support. Upper endoscopy demonstrated hemobilia (Figure 1a). Labs were notable for hemoglobin 7.6, platelet count 49,000, and INR 2.3. Interventional Radiology was consulted for transcatheter arterial embolization (TAE), but non-invasive imaging supported variceal bleeding in the distal bile duct due to portal hypertensive biliopathy rather than arterial bleeding (Figure 2). A TIPS procedure was considered but determined to be too risky in the setting of his clinical instability. Endoscopic retrograde cholangiopancreatography (ERCP) was performed with placement of one fully covered self-expandable metal stent (FCSEMS) into the common bile duct, achieving hemostasis (Figure 1b) and clinical stability. He underwent liver transplantation with successful duct-to-duct biliary anastomosis. The stent was removed two days later without further hemobilia.
Discussion: Treatment goals in hemobilia are hemostasis and maintenance of bile flow. TAE is becoming the gold standard for treatment of persistent arterial hemobilia in hemodynamically unstable patients. Endoscopic biliary stent placement is the initial therapy for venous hemobilia in hemodynamically stable patients. TAE would have been therapeutically ineffective in our patient due to the venous source of bleeding. Moreover, given the presence of a thrombosed portal vein, TAE could have led to significant hepatic ischemia. Though palliative biliary stenting for portal biliopathy has been reported previously, the success of ERCP with FCSEMS in our patient highlights the use of FCSEMS as a bridge to liver transplantation in patients with hemodynamically unstable hemobilia secondary to portal biliopathy.
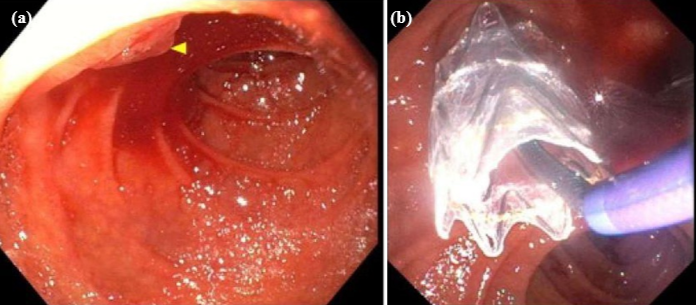
Figure: Figure 1. (a) Red blood in the second portion of the duodenum with bright red blood actively hemorrhaging from the papilla with washing, visualized during initial esophagogastroduodenoscopy. (b) Placement of one 10mm x 6cm fully covered self-expandable metal stent 4cm into the common bile duct, crossing the ampulla and papilla without sphincterotomy, during endoscopic retrograde cholangiopancreatography.
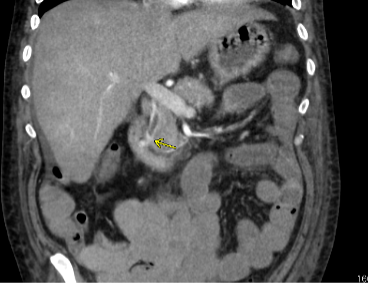
Figure: Figure 2. Computed tomography angiogram of the abdomen demonstrated hyper enhancement of the ampulla/papilla without active extravasation, consistent with biliary varices.
Disclosures:
Anneleise Frie indicated no relevant financial relationships.
Joshua Morny indicated no relevant financial relationships.
Nimrod Deiss-Yehiely indicated no relevant financial relationships.
Samuel Koebe indicated no relevant financial relationships.
Michael Woods indicated no relevant financial relationships.
Patrick Pfau indicated no relevant financial relationships.
Anneleise Frie, MD1, Joshua Morny, MBChB2, Nimrod Deiss-Yehiely, MD3, Samuel Koebe, MD4, Michael Woods, MD4, Patrick Pfau, MD5. P3578 - Hemostasis With Fully Covered Self-Expanding Bare Metal Stent as a Bridge to Liver Transplantation in a Patient With Acute Liver Injury and Hemodynamically Unstable Hemobilia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
