Monday Poster Session
Category: Interventional Endoscopy
P3573 - The “Light Bulb Moment": Performing Gastrobulbostomy for a Malignant Gastric Outlet Obstruction
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MC
Mark Cromer, MD
Prisma Health Greenville Memorial Hospital
Greenville, SC
Presenting Author(s)
Award: ACG Presidential Poster Award
Mark Cromer, MD, Varun Moktan, MD, Juan E. Corral, MD, Kalpit Devani, MD
Prisma Health Greenville Memorial Hospital, Greenville, SC
Introduction: Therapeutic options for symptom relief of malignant gastric outlet obstruction (MGOO) include surgical gastroenterostomy (S-GE), endoscopic stenting (ES), and endoscopic ultrasound-guided gastroenterostomy (EUS-GE). S-GE can provide excellent symptom relief durability but also involves higher risk of morbidity and mortality. ES provides rapid symptom relief but is often limited by stent dysfunction or migration. This case demonstrates EUS-gastrobulbostomy as a novel EUS-GE approach for MGOO.
Case Description/
Methods: A 51-year-old obese female, nonsmoker, with unknown Helicobacter pylori status initially presented for abdominal pain and oral intake intolerance. Computed tomography (CT) scan revealed irregular gastric antral wall thickening and diffuse mesenteric stranding and nodularity. Endoscopic biopsies at an external facility diagnosed poorly differentiated, HER2-negative gastric adenocarcinoma. Two weeks later she presented to our facility for worsening nausea, vomiting and abdominal distension. Repeat imaging revealed marked interval progression of suspected metastatic peritoneal disease with new large volume ascites. Cytology from paracentesis was suspicious for malignancy (indeterminate) and negative for infection. An upper gastrointestinal series showed a distended, debris-filled stomach with transition in the gastric antrum and minimal contrast flow into the duodenum. It was decided to attempt EUS-GE. On endoscopy, the gastric antral mass was causing proximal gastric dilation, but the examined duodenum was normal. On EUS, no jejunal limb was found in adequate proximity to the stomach for access, but the duodenal bulb was widely patent and only 18mm from the lesser curvature. Using fluoroscopy and EUS guidance, a 15 x 10mm lumen-apposing metal stent was used to successfully create a gastrobulbostomy, bypassing a segment of peri-gastric ascites. The next day, the patient’s nausea and vomiting had resolved, she tolerated oral intake, and her nasogastric tube was eventually removed.
Discussion: EUS-GE is an effective intervention for GOO in terminally ill patients, with 87-100% technical success, and 82-100% clinical success. EUS-GE has also demonstrated higher clinical success, lower need for re-intervention, shorter length of hospitalization, and lower adverse event rates than S-GE or ES. While EUS-GE typically involves accessing the third or fourth portions of the duodenum or proximal jejunum, this case demonstrates gastrobulbostomy to be a viable approach for an antral MGOO.
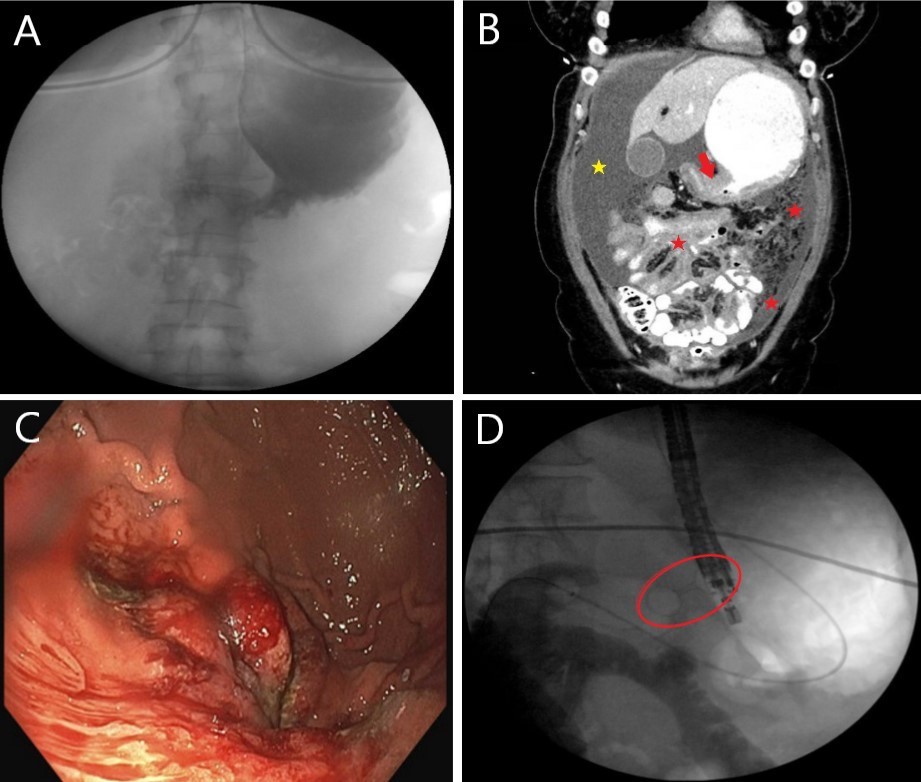
Figure: Figure 1: Case images
A) Upper gastrointestinal series depicting a distended, fluid-filled stomach with only trace contrast entering the duodenum, concerning for partial gastric outlet obstruction.
B) Coronal view of computed tomography scan showing antral wall thickening (arrow), distended, contrast-filled stomach with transition in the gastric antrum suspicious for partial gastric outlet obstruction; omental caking / peritoneal carcinomatosis and mesenteric stranding (red stars); and abdominopelvic ascites (yellow star)
C) Endoscopy image showing a circumferential, nodular, erythematous mass in the gastric antrum causing luminal narrowing
D) Fluoroscopy image demonstrating successful deployment of a lumen-apposing metal stent creating a gastrobulbostomy (circled)
Disclosures:
Mark Cromer indicated no relevant financial relationships.
Varun Moktan indicated no relevant financial relationships.
Juan Corral indicated no relevant financial relationships.
Kalpit Devani indicated no relevant financial relationships.
Mark Cromer, MD, Varun Moktan, MD, Juan E. Corral, MD, Kalpit Devani, MD. P3573 - The “Light Bulb Moment": Performing Gastrobulbostomy for a Malignant Gastric Outlet Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mark Cromer, MD, Varun Moktan, MD, Juan E. Corral, MD, Kalpit Devani, MD
Prisma Health Greenville Memorial Hospital, Greenville, SC
Introduction: Therapeutic options for symptom relief of malignant gastric outlet obstruction (MGOO) include surgical gastroenterostomy (S-GE), endoscopic stenting (ES), and endoscopic ultrasound-guided gastroenterostomy (EUS-GE). S-GE can provide excellent symptom relief durability but also involves higher risk of morbidity and mortality. ES provides rapid symptom relief but is often limited by stent dysfunction or migration. This case demonstrates EUS-gastrobulbostomy as a novel EUS-GE approach for MGOO.
Case Description/
Methods: A 51-year-old obese female, nonsmoker, with unknown Helicobacter pylori status initially presented for abdominal pain and oral intake intolerance. Computed tomography (CT) scan revealed irregular gastric antral wall thickening and diffuse mesenteric stranding and nodularity. Endoscopic biopsies at an external facility diagnosed poorly differentiated, HER2-negative gastric adenocarcinoma. Two weeks later she presented to our facility for worsening nausea, vomiting and abdominal distension. Repeat imaging revealed marked interval progression of suspected metastatic peritoneal disease with new large volume ascites. Cytology from paracentesis was suspicious for malignancy (indeterminate) and negative for infection. An upper gastrointestinal series showed a distended, debris-filled stomach with transition in the gastric antrum and minimal contrast flow into the duodenum. It was decided to attempt EUS-GE. On endoscopy, the gastric antral mass was causing proximal gastric dilation, but the examined duodenum was normal. On EUS, no jejunal limb was found in adequate proximity to the stomach for access, but the duodenal bulb was widely patent and only 18mm from the lesser curvature. Using fluoroscopy and EUS guidance, a 15 x 10mm lumen-apposing metal stent was used to successfully create a gastrobulbostomy, bypassing a segment of peri-gastric ascites. The next day, the patient’s nausea and vomiting had resolved, she tolerated oral intake, and her nasogastric tube was eventually removed.
Discussion: EUS-GE is an effective intervention for GOO in terminally ill patients, with 87-100% technical success, and 82-100% clinical success. EUS-GE has also demonstrated higher clinical success, lower need for re-intervention, shorter length of hospitalization, and lower adverse event rates than S-GE or ES. While EUS-GE typically involves accessing the third or fourth portions of the duodenum or proximal jejunum, this case demonstrates gastrobulbostomy to be a viable approach for an antral MGOO.
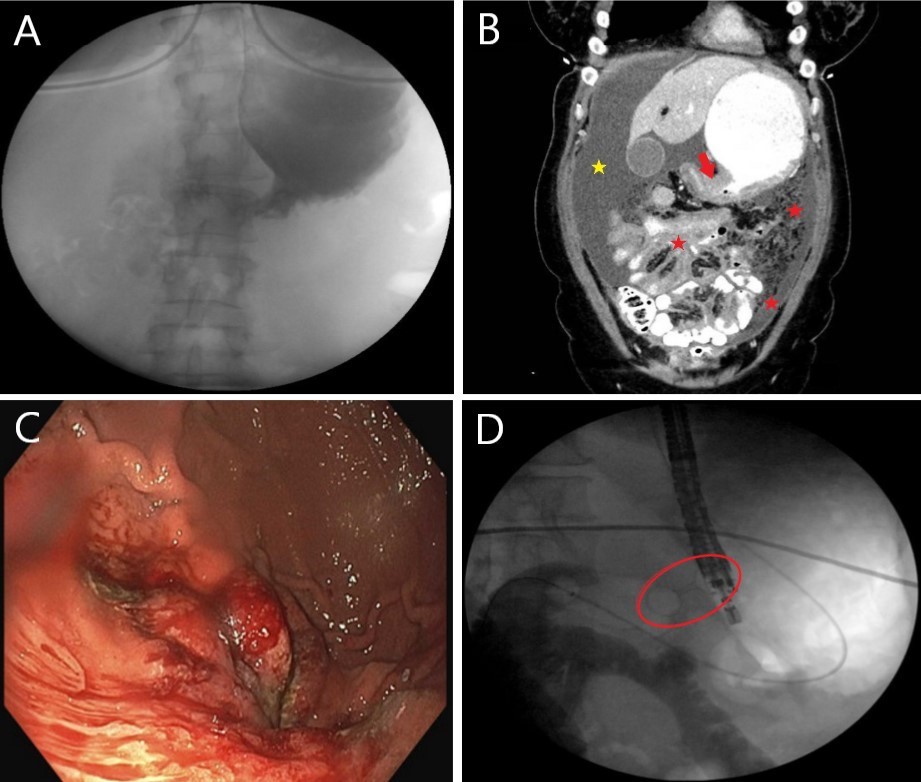
Figure: Figure 1: Case images
A) Upper gastrointestinal series depicting a distended, fluid-filled stomach with only trace contrast entering the duodenum, concerning for partial gastric outlet obstruction.
B) Coronal view of computed tomography scan showing antral wall thickening (arrow), distended, contrast-filled stomach with transition in the gastric antrum suspicious for partial gastric outlet obstruction; omental caking / peritoneal carcinomatosis and mesenteric stranding (red stars); and abdominopelvic ascites (yellow star)
C) Endoscopy image showing a circumferential, nodular, erythematous mass in the gastric antrum causing luminal narrowing
D) Fluoroscopy image demonstrating successful deployment of a lumen-apposing metal stent creating a gastrobulbostomy (circled)
Disclosures:
Mark Cromer indicated no relevant financial relationships.
Varun Moktan indicated no relevant financial relationships.
Juan Corral indicated no relevant financial relationships.
Kalpit Devani indicated no relevant financial relationships.
Mark Cromer, MD, Varun Moktan, MD, Juan E. Corral, MD, Kalpit Devani, MD. P3573 - The “Light Bulb Moment": Performing Gastrobulbostomy for a Malignant Gastric Outlet Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

