Monday Poster Session
Category: Liver
P3682 - Frailty in Autoimmune Hepatitis Hospitalizations: A Predictor of Worse Outcomes and Elevated Transplant Needs
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ali Jaan, MD
Unity Hospital
Rochester, NY
Presenting Author(s)
Ali Jaan, MD1, Adeena Maryyum, 2, Kamran Qureshi, MD3, Wing-Kin Syn, MD, PhD3
1Unity Hospital, Rochester, NY; 2Ayub Medical College, Abbottabad, North-West Frontier, Pakistan; 3Saint Louis University School of Medicine, Saint Louis, MO
Introduction: Frailty, a surrogate for diminished physiological reserve, remains an underexplored determinant of the clinical course of autoimmune hepatitis (AIH). We evaluated the independent prognostic significance of frailty in predicting outcomes and healthcare utilization to understand its impact on altering the disease trajectory.
Methods: Utilizing the data from the National Readmission Database (NRD) 2016 - 2019, patients hospitalized with a principal diagnosis of AIH were identified using the International Classification of Diseases, 10th revision, Clinical Modifications (ICD-10-CM) codes and categorized into young (age 18-64 years) and elderly (age ≥65 years) groups. The two groups were further stratified by frailty status, determined via the validated Hospital Frailty Risk Score. Multivariable regression models were employed to evaluate the independent association between frailty, clinical outcomes, and healthcare utilization using STATA version 14.2 for statistical analysis.
Results: Among the 12,960 hospitalized patients with AIH, a total of 26.27% (n=2,436) young and 45.4% (n=1,674) elderly were categorized as frail (Table 1). The frail cohorts were older, with a higher prevalence of cirrhosis and disproportionate comorbidity burden (p< 0.001) in both young and elderly age groups. Adjusted analysis revealed a significantly higher mortality among frail individuals (adjusted odds ratio [aOR], 20.42 & 7.62 for young and elderly; p< 0.001) (Table 2). Moreover, frail patients exhibited elevated odds for spontaneous bacterial peritonitis, coagulopathy, hepatorenal syndrome, and hepatic encephalopathy in both age groups. The clinical course of frail patients was further complicated by a greater need for intensive care unit admission (p< 0.001), and elevated odds of liver failure, associated with higher odds for requiring liver transplant. Finally, resource utilization, estimated by length of stay, total hospitalization charges, and discharge to rehabilitation facilities, were also significantly higher among patients with frailty (p< 0.001).
Discussion: Our findings underscore frailty as a pivotal determinant of prognosis in patients with AIH, independently amplifying the risk of mortality, hepatic complications, intensive and care and liver transplant needs, highlighting the critical need for early frailty recognition and incorporation into stratification models to guide the prognosis, management, and allocation of care.
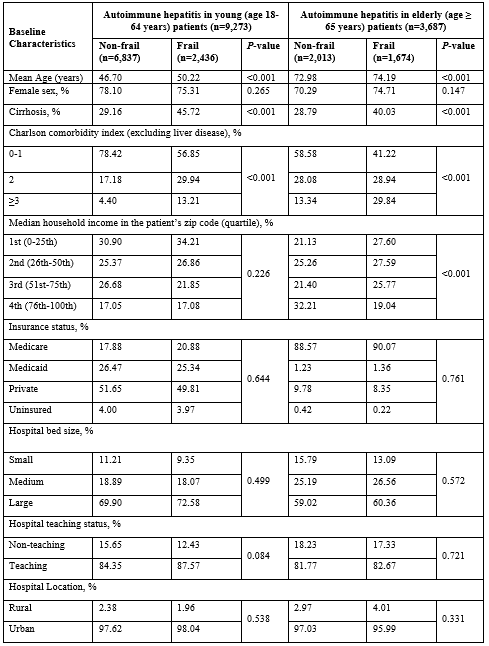
Figure: Table 1: Baseline characteristics of autoimmune hepatitis hospitalizations, stratified by frailty.
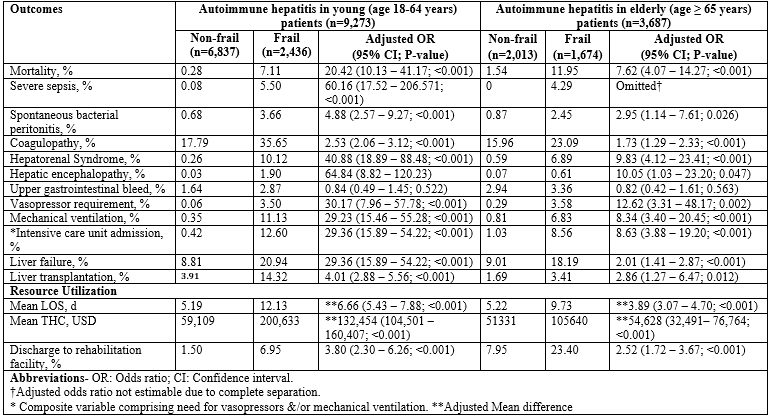
Figure: Table 2: Unadjusted and adjusted outcomes of autoimmune hepatitis hospitalizations, stratified by frailty status.
Disclosures:
Ali Jaan indicated no relevant financial relationships.
Adeena Maryyum indicated no relevant financial relationships.
Kamran Qureshi indicated no relevant financial relationships.
Wing-Kin Syn indicated no relevant financial relationships.
Ali Jaan, MD1, Adeena Maryyum, 2, Kamran Qureshi, MD3, Wing-Kin Syn, MD, PhD3. P3682 - Frailty in Autoimmune Hepatitis Hospitalizations: A Predictor of Worse Outcomes and Elevated Transplant Needs, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Unity Hospital, Rochester, NY; 2Ayub Medical College, Abbottabad, North-West Frontier, Pakistan; 3Saint Louis University School of Medicine, Saint Louis, MO
Introduction: Frailty, a surrogate for diminished physiological reserve, remains an underexplored determinant of the clinical course of autoimmune hepatitis (AIH). We evaluated the independent prognostic significance of frailty in predicting outcomes and healthcare utilization to understand its impact on altering the disease trajectory.
Methods: Utilizing the data from the National Readmission Database (NRD) 2016 - 2019, patients hospitalized with a principal diagnosis of AIH were identified using the International Classification of Diseases, 10th revision, Clinical Modifications (ICD-10-CM) codes and categorized into young (age 18-64 years) and elderly (age ≥65 years) groups. The two groups were further stratified by frailty status, determined via the validated Hospital Frailty Risk Score. Multivariable regression models were employed to evaluate the independent association between frailty, clinical outcomes, and healthcare utilization using STATA version 14.2 for statistical analysis.
Results: Among the 12,960 hospitalized patients with AIH, a total of 26.27% (n=2,436) young and 45.4% (n=1,674) elderly were categorized as frail (Table 1). The frail cohorts were older, with a higher prevalence of cirrhosis and disproportionate comorbidity burden (p< 0.001) in both young and elderly age groups. Adjusted analysis revealed a significantly higher mortality among frail individuals (adjusted odds ratio [aOR], 20.42 & 7.62 for young and elderly; p< 0.001) (Table 2). Moreover, frail patients exhibited elevated odds for spontaneous bacterial peritonitis, coagulopathy, hepatorenal syndrome, and hepatic encephalopathy in both age groups. The clinical course of frail patients was further complicated by a greater need for intensive care unit admission (p< 0.001), and elevated odds of liver failure, associated with higher odds for requiring liver transplant. Finally, resource utilization, estimated by length of stay, total hospitalization charges, and discharge to rehabilitation facilities, were also significantly higher among patients with frailty (p< 0.001).
Discussion: Our findings underscore frailty as a pivotal determinant of prognosis in patients with AIH, independently amplifying the risk of mortality, hepatic complications, intensive and care and liver transplant needs, highlighting the critical need for early frailty recognition and incorporation into stratification models to guide the prognosis, management, and allocation of care.
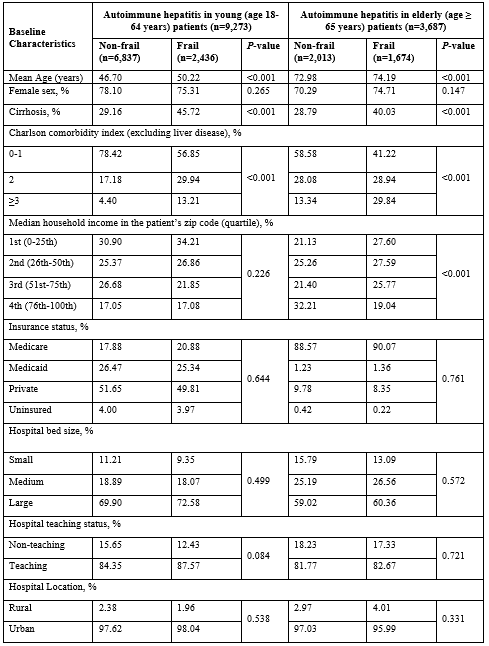
Figure: Table 1: Baseline characteristics of autoimmune hepatitis hospitalizations, stratified by frailty.
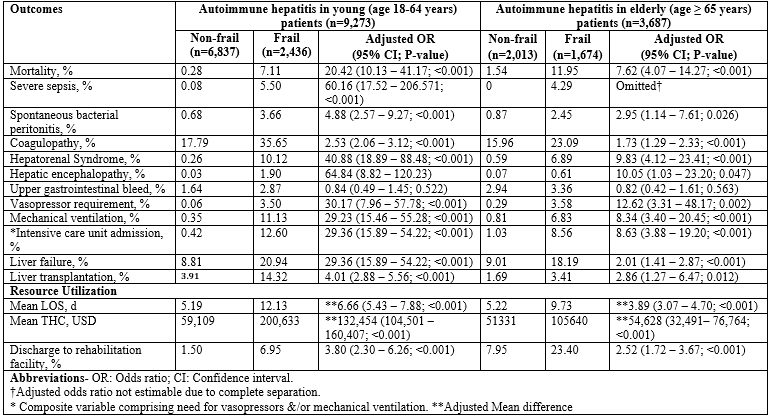
Figure: Table 2: Unadjusted and adjusted outcomes of autoimmune hepatitis hospitalizations, stratified by frailty status.
Disclosures:
Ali Jaan indicated no relevant financial relationships.
Adeena Maryyum indicated no relevant financial relationships.
Kamran Qureshi indicated no relevant financial relationships.
Wing-Kin Syn indicated no relevant financial relationships.
Ali Jaan, MD1, Adeena Maryyum, 2, Kamran Qureshi, MD3, Wing-Kin Syn, MD, PhD3. P3682 - Frailty in Autoimmune Hepatitis Hospitalizations: A Predictor of Worse Outcomes and Elevated Transplant Needs, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
