Monday Poster Session
Category: Liver
P3678 - Association Between MASLD and Atherosclerotic Cardiovascular Disease Risk Among US Adults
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- CO
Chukwuemeka Ogbu, MD, MPH
Cape Fear valley Medical Center
Fayetteville, NC
Presenting Author(s)
Chukwuemeka Ogbu, MD, MPH1, Ndukwe J. Kalu, MD, MPH2, Shoon Oo, MD3, Elizabeth Onyeaso, MD3, A. Sidney Barrett, MD, MSCR4
1Cape Fear valley Medical Center, Fayetteville, NC; 2Cape Fear Health, Fayetteville, NC; 3Cape Fear Valley Health, Fayetteville, NC; 4Division of Gastroenterology and Hepatology, University of North Carolina, Chapel Hill, NC
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is a growing public health concern due to its implications for cardiovascular (CV) risk. What is less clear are the individual roles of steatosis and fibrosis in conferring CV risk. Using a nationally representative sample, we evaluated the association between MASLD and estimated 10-year atherosclerotic cardiovascular disease (ASCVD) risk among U.S. adults.
Methods: We conducted a cross-sectional analysis of U.S. adults aged 40–79 years from NHANES 2017–2020 with complete vibration-controlled transient elastography (VCTE), cardiometabolic, and laboratory data. Exclusion criteria included pregnancy, viral hepatitis (HBsAg-positive or HCV RNA-positive), excessive alcohol use ( >30g/day for men, >20g/day for women), known liver disease, and prior cardiovascular events. Participants with missing data required to calculate ASCVD risk scores were excluded. MASLD was defined as a Controlled Attenuation Parameter (CAP) ≥288 dB/m plus ≥1 cardiometabolic risk factor. Significant fibrosis was defined as liver stiffness measurement ≥8.0 kPa. A four-category composite exposure variable was created as follows: MASLD - /Fibrosis -, MASLD +/Fibrosis-, MASLD-/Fibrosis+, and MASLD+/Fibrosis+. The primary outcome was elevated 10-year ASCVD risk (≥7.5%) calculated using pooled cohort equations. Survey-weighted logistic regression models adjusted for sociodemographic variable, physical activity, statin use and log-transformed CRP. Sensitivity analyses examined continuous ASCVD risk score and stratified by obesity and sex.
Results: A total of 1,336 participants met inclusion criteria for ASCVD risk estimation. The weighted MASLD prevalence was 39.8%. Among participants with MASLD, 50.6% had elevated ASCVD risk (≥7.5%), compared to 34.5% among those without MASLD (p = 0.0023). After adjustment, MASLD+/Fibrosis+ conferred the greatest odds (aOR: 2.19; 95% CI: 1.13–4.00; p = 0.018), followed by MASLD without fibrosis (aOR: 1.70; 95% CI: 1.03–2.40; p = 0.038). Fibrosis alone showed no significant association.
Discussion: Our findings demonstrate that MASLD especially with concomitant fibrosis, is independently associated with elevated 10-year ASCVD risk. Interestingly, fibrosis alone, does not increase CV risk, suggesting that interventions to reduce steatosis may mitigate CV risk prior to fibrosis improvement. These findings underscore the importance of CVD risk stratification in MASLD management, even among those without obesity or established CVD.
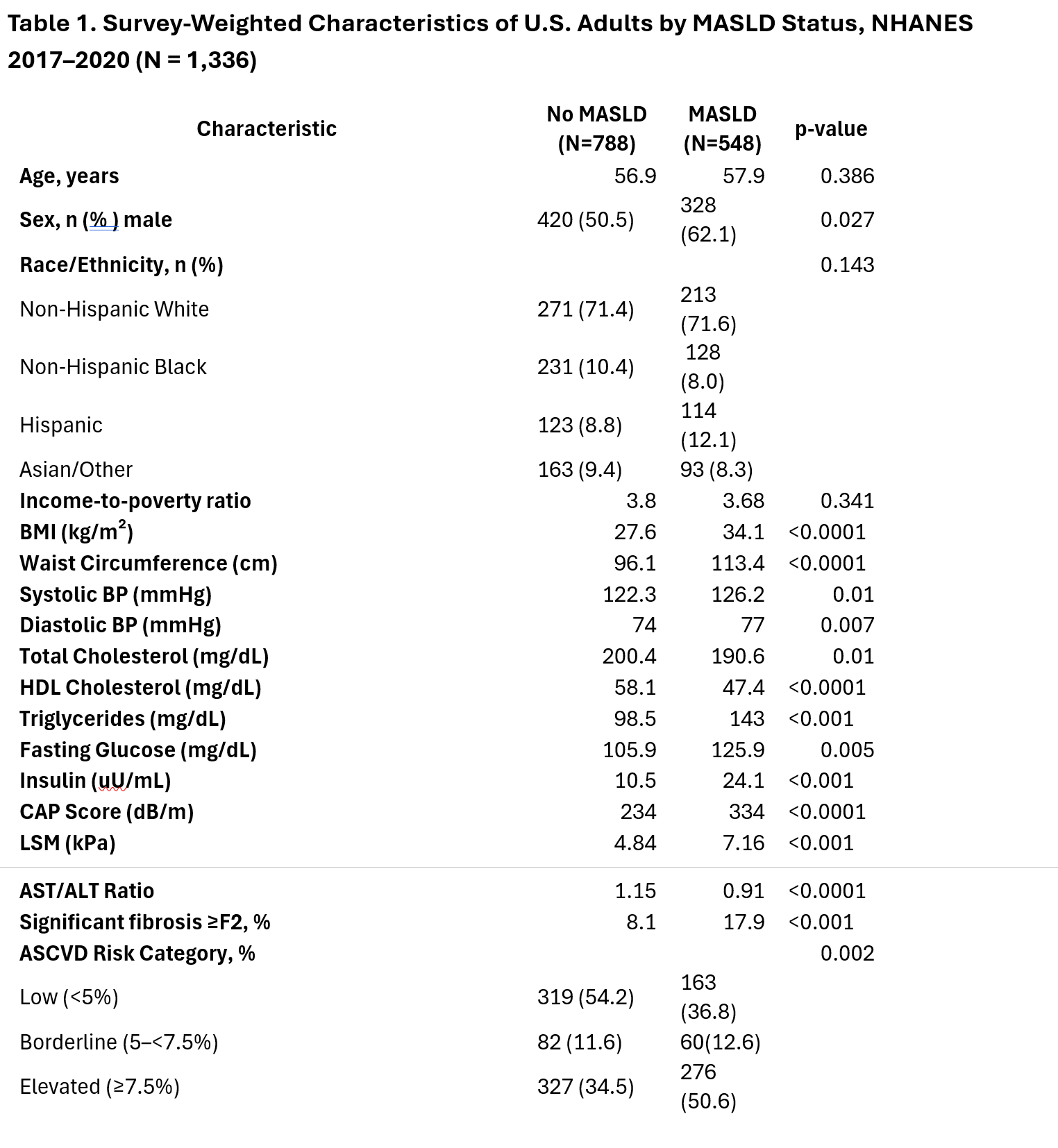
Figure: Values are presented as mean or n (weighted %) unless otherwise indicated. Comparisons between MASLD and non-MASLD groups were based on survey-weighted t-tests for continuous variables and Rao-Scott χ² tests for categorical variables. ASCVD risk was based on 10-year predicted risk using pooled cohort equations. Significant fibrosis was defined as liver stiffness ≥8.0 kPa. Percentages reflect population-weighted estimates; raw counts may not align proportionally due to complex survey weighting. BMI – Body Mass Index; BP – Blood Pressure; HDL – High-Density Lipoprotein; CAP – Controlled Attenuation Parameter; LSM – Liver Stiffness Measurement; AST/ALT – Aspartate Aminotransferase to Alanine Aminotransferase Ratio; uU/mL – Micro-Units per Milliliter; dB/m – Decibels per Meter; kPa – Kilopascals; mg/dL – Milligrams per Deciliter; ASCVD – Atherosclerotic Cardiovascular Disease.
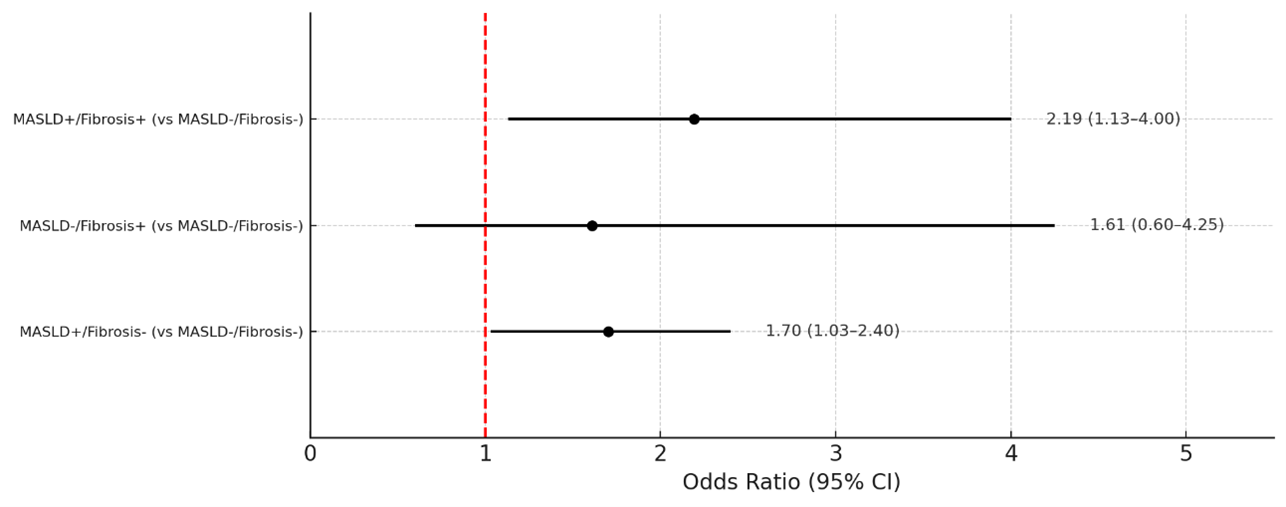
Figure: Association Between MASLD and Elevated 10-Year ASCVD Risk (≥7.5%)
Odds ratios and 95% confidence intervals were estimated using survey-weighted logistic regression models adjusted for education, income-to-poverty ratio, physical activity level, statin use and log-transformed CRP. "No MASLD / No Fibrosis" was used as the reference category for composite exposures. Analyses are based on NHANES 2017–2020 data.
Disclosures:
Chukwuemeka Ogbu indicated no relevant financial relationships.
Ndukwe Kalu indicated no relevant financial relationships.
Shoon Oo indicated no relevant financial relationships.
Elizabeth Onyeaso indicated no relevant financial relationships.
A. Sidney Barrett: Boehringer Ingelheim – Consultant. LifeEdit – Consultant. Madrigal – Consultant. Merck – Consultant. Mirium – Consultant. Target RWE – Consultant.
Chukwuemeka Ogbu, MD, MPH1, Ndukwe J. Kalu, MD, MPH2, Shoon Oo, MD3, Elizabeth Onyeaso, MD3, A. Sidney Barrett, MD, MSCR4. P3678 - Association Between MASLD and Atherosclerotic Cardiovascular Disease Risk Among US Adults, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cape Fear valley Medical Center, Fayetteville, NC; 2Cape Fear Health, Fayetteville, NC; 3Cape Fear Valley Health, Fayetteville, NC; 4Division of Gastroenterology and Hepatology, University of North Carolina, Chapel Hill, NC
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is a growing public health concern due to its implications for cardiovascular (CV) risk. What is less clear are the individual roles of steatosis and fibrosis in conferring CV risk. Using a nationally representative sample, we evaluated the association between MASLD and estimated 10-year atherosclerotic cardiovascular disease (ASCVD) risk among U.S. adults.
Methods: We conducted a cross-sectional analysis of U.S. adults aged 40–79 years from NHANES 2017–2020 with complete vibration-controlled transient elastography (VCTE), cardiometabolic, and laboratory data. Exclusion criteria included pregnancy, viral hepatitis (HBsAg-positive or HCV RNA-positive), excessive alcohol use ( >30g/day for men, >20g/day for women), known liver disease, and prior cardiovascular events. Participants with missing data required to calculate ASCVD risk scores were excluded. MASLD was defined as a Controlled Attenuation Parameter (CAP) ≥288 dB/m plus ≥1 cardiometabolic risk factor. Significant fibrosis was defined as liver stiffness measurement ≥8.0 kPa. A four-category composite exposure variable was created as follows: MASLD - /Fibrosis -, MASLD +/Fibrosis-, MASLD-/Fibrosis+, and MASLD+/Fibrosis+. The primary outcome was elevated 10-year ASCVD risk (≥7.5%) calculated using pooled cohort equations. Survey-weighted logistic regression models adjusted for sociodemographic variable, physical activity, statin use and log-transformed CRP. Sensitivity analyses examined continuous ASCVD risk score and stratified by obesity and sex.
Results: A total of 1,336 participants met inclusion criteria for ASCVD risk estimation. The weighted MASLD prevalence was 39.8%. Among participants with MASLD, 50.6% had elevated ASCVD risk (≥7.5%), compared to 34.5% among those without MASLD (p = 0.0023). After adjustment, MASLD+/Fibrosis+ conferred the greatest odds (aOR: 2.19; 95% CI: 1.13–4.00; p = 0.018), followed by MASLD without fibrosis (aOR: 1.70; 95% CI: 1.03–2.40; p = 0.038). Fibrosis alone showed no significant association.
Discussion: Our findings demonstrate that MASLD especially with concomitant fibrosis, is independently associated with elevated 10-year ASCVD risk. Interestingly, fibrosis alone, does not increase CV risk, suggesting that interventions to reduce steatosis may mitigate CV risk prior to fibrosis improvement. These findings underscore the importance of CVD risk stratification in MASLD management, even among those without obesity or established CVD.
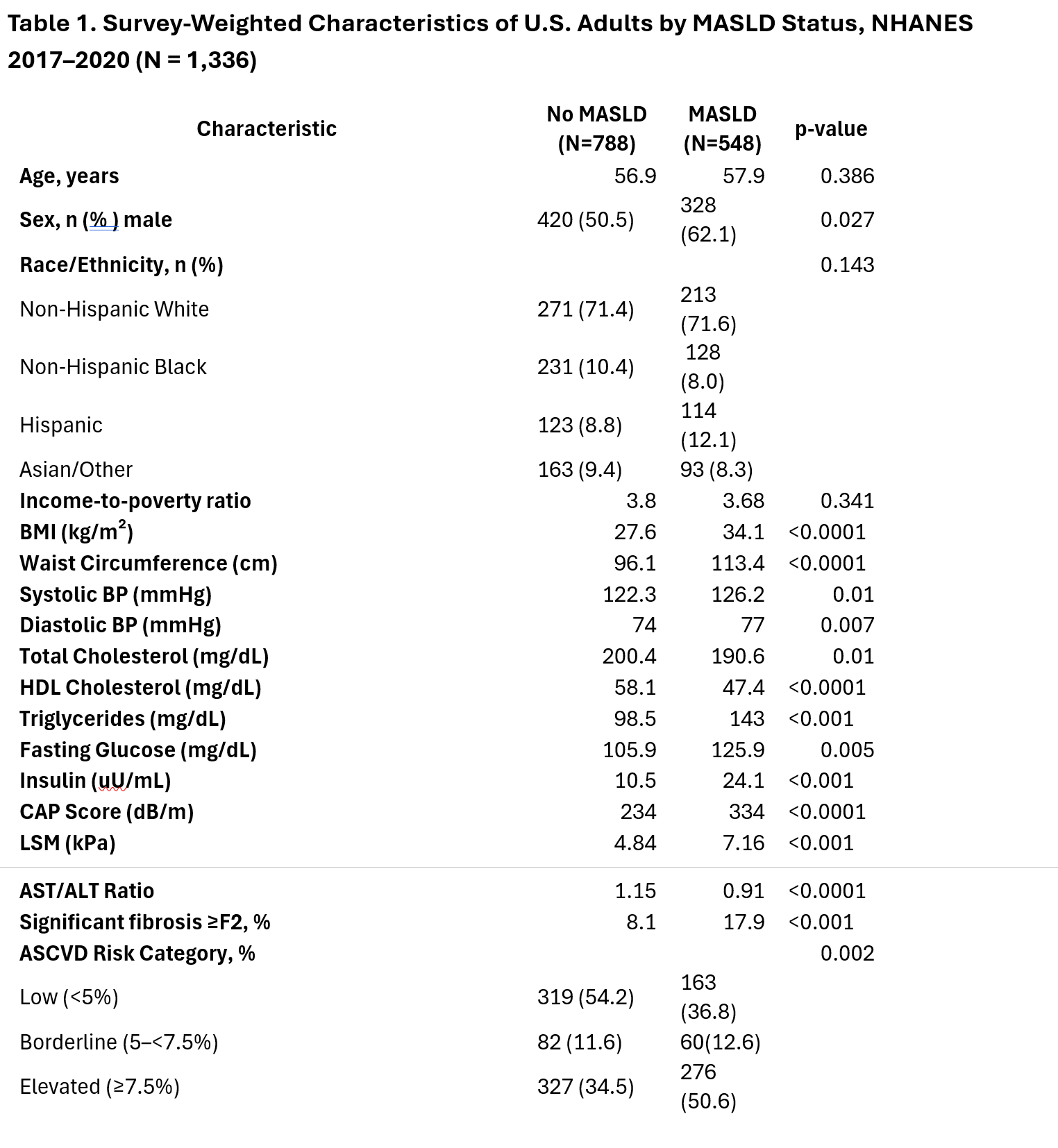
Figure: Values are presented as mean or n (weighted %) unless otherwise indicated. Comparisons between MASLD and non-MASLD groups were based on survey-weighted t-tests for continuous variables and Rao-Scott χ² tests for categorical variables. ASCVD risk was based on 10-year predicted risk using pooled cohort equations. Significant fibrosis was defined as liver stiffness ≥8.0 kPa. Percentages reflect population-weighted estimates; raw counts may not align proportionally due to complex survey weighting. BMI – Body Mass Index; BP – Blood Pressure; HDL – High-Density Lipoprotein; CAP – Controlled Attenuation Parameter; LSM – Liver Stiffness Measurement; AST/ALT – Aspartate Aminotransferase to Alanine Aminotransferase Ratio; uU/mL – Micro-Units per Milliliter; dB/m – Decibels per Meter; kPa – Kilopascals; mg/dL – Milligrams per Deciliter; ASCVD – Atherosclerotic Cardiovascular Disease.
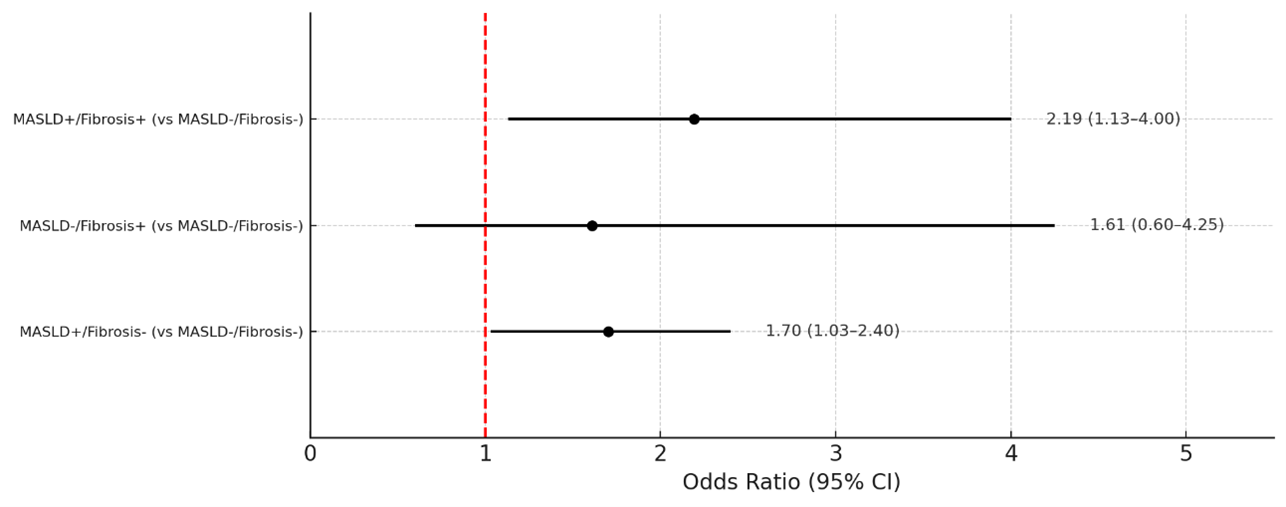
Figure: Association Between MASLD and Elevated 10-Year ASCVD Risk (≥7.5%)
Odds ratios and 95% confidence intervals were estimated using survey-weighted logistic regression models adjusted for education, income-to-poverty ratio, physical activity level, statin use and log-transformed CRP. "No MASLD / No Fibrosis" was used as the reference category for composite exposures. Analyses are based on NHANES 2017–2020 data.
Disclosures:
Chukwuemeka Ogbu indicated no relevant financial relationships.
Ndukwe Kalu indicated no relevant financial relationships.
Shoon Oo indicated no relevant financial relationships.
Elizabeth Onyeaso indicated no relevant financial relationships.
A. Sidney Barrett: Boehringer Ingelheim – Consultant. LifeEdit – Consultant. Madrigal – Consultant. Merck – Consultant. Mirium – Consultant. Target RWE – Consultant.
Chukwuemeka Ogbu, MD, MPH1, Ndukwe J. Kalu, MD, MPH2, Shoon Oo, MD3, Elizabeth Onyeaso, MD3, A. Sidney Barrett, MD, MSCR4. P3678 - Association Between MASLD and Atherosclerotic Cardiovascular Disease Risk Among US Adults, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
