Monday Poster Session
Category: Liver
P3670 - De Novo Gastrointestinal Malignancies Among Liver Transplant Recipients
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Chawin Lopimpisuth, MD
University of Miami Miller School of Medicine at Jackson Memorial Hospital
Miami, FL
Presenting Author(s)
Award: ACG Presidential Poster Award
Chawin Lopimpisuth, MD1, Alisa Likhitsup, MD2
1University of Miami Miller School of Medicine at Jackson Memorial Hospital, Miami, FL; 2University of Michigan, Ann Arbor, MI
Introduction: De novo malignancies (DNM) are one of the most common long-term complications following liver transplantation (LT), particularly in the gastrointestinal (GI) tract. The incidence has been reported to be 2 – 3 times higher than in the general population. Our study sought to identify the cumulative incidence and risk factors related to GI DNM among LT recipients.
Methods: We conducted a cohort study using the United Network Organ Sharing (UNOS) database, evaluating all adult LT recipients (aged 18 years or older) from 1997 – 2023. GI DNM included esophageal, stomach, small bowel, pancreatic, and colorectal cancers (CRC) occurring at least 1 year after LT. A competing risk regression model was used to assess cumulative incidence of GI DNM in relation to primary indication of LT and history of hepatocellular carcinoma (HCC) and/or cholangiocarcinoma (CCA) with death as a competing event. Multivariable Cox proportional hazards regression models were used to identify factors associated with GI DNM.
Results: A total of 137,742 patients were analyzed; median age was 55 (IQR 48 – 62) years, 72.1% were White, and 20.7% had history of HCC/CCA (Table 1). GI DNM occurred in 1,426 (1.0%) LT recipients (572 [40.1%] CRC, 462 [32.3%] pancreatic, 226 [15.8%] esophageal, 124 [8.6%] gastric, and 55 [3.8%] small bowel cancers). Median follow-up time was 6.4 (IQR 3.1 – 11.1) years. The 5-, 10-, 15-year cumulative incidence of GI DNM were highest among PSC patients (2.0, 2.8, 5.4% for PSC with HCC/CCA and 1.0, 2.3, 4.4% for PSC without HCC/CCA), followed by alcohol-associated liver disease (ALD) (1.0, 2.9, 4.5% for ALD with HCC and 0.5, 1.4, 2.3% for ALD without HCC), MASLD (1.1, 2.6, 3.6% for MASLD with HCC and 0.5, 1.2, 2.0% for MASLD without HCC), and HCV (0.6, 1.5, 2.3% for HCV with HCC and 0.3, 1.0, 1.7% for HCV without HCC) (Figure 1). In multivariate Cox regression analysis, GI DNM developed more among older patients (aHR 1.04; CI 1.03 – 1.04), those with ALD (aHR 1.27; CI 1.06 – 1.52), PSC (aHR 2.39; CI 1.91 – 2.99), prior HCC (aHR 1.35; CI 1.15 – 1.57), and less among Hispanic patients (aHR 0.76; CI 0.63 – 0.93).
Discussion: In this large retrospective study, the incidence of GI DNM varied by the liver disease etiology, and the highest rates noted in patients with PSC. Age, ALD, and a history of HCC/CCA were associated with increased risk. These findings support the need of more tailored and vigilant cancer screening strategies in LT recipients.
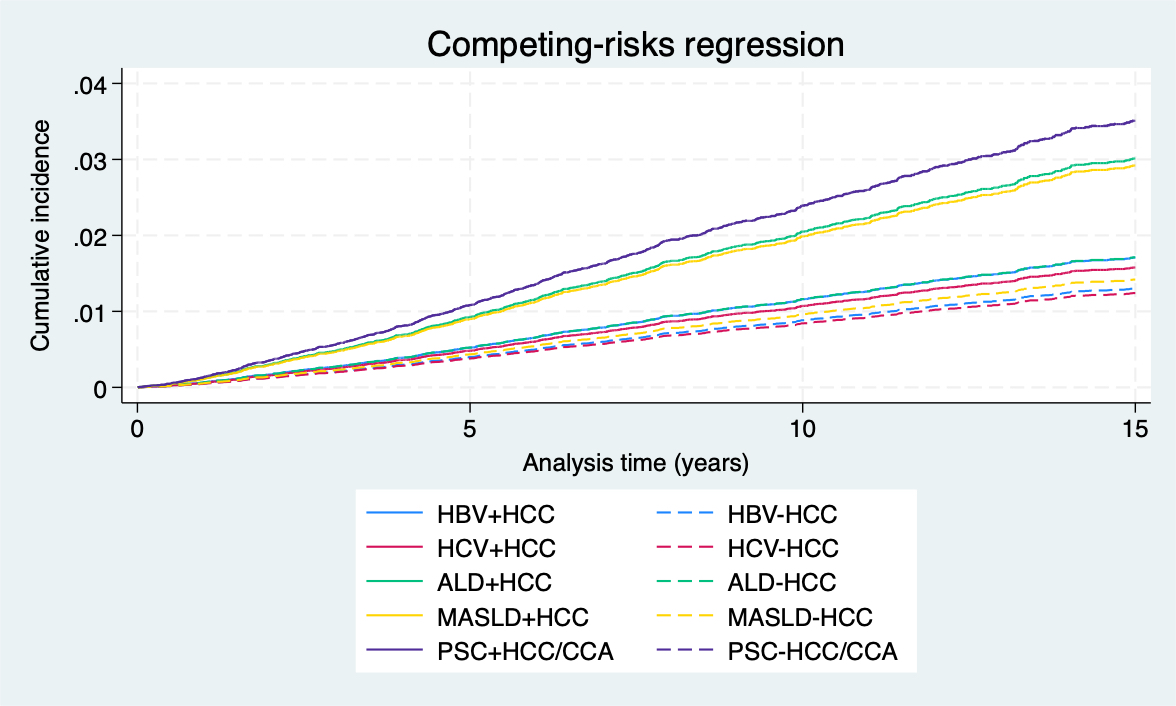
Figure: Figure 1: Cumulative incidence of GI DNM in relation to primary indication of LT and history of HCC/CCA.

Figure: Table 1: Baseline recipient characteristics
† Continuous variables presented as median and IQR; categorical variables presented as N (%)
Disclosures:
Chawin Lopimpisuth indicated no relevant financial relationships.
Alisa Likhitsup indicated no relevant financial relationships.
Chawin Lopimpisuth, MD1, Alisa Likhitsup, MD2. P3670 - <i>De Novo</i> Gastrointestinal Malignancies Among Liver Transplant Recipients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Chawin Lopimpisuth, MD1, Alisa Likhitsup, MD2
1University of Miami Miller School of Medicine at Jackson Memorial Hospital, Miami, FL; 2University of Michigan, Ann Arbor, MI
Introduction: De novo malignancies (DNM) are one of the most common long-term complications following liver transplantation (LT), particularly in the gastrointestinal (GI) tract. The incidence has been reported to be 2 – 3 times higher than in the general population. Our study sought to identify the cumulative incidence and risk factors related to GI DNM among LT recipients.
Methods: We conducted a cohort study using the United Network Organ Sharing (UNOS) database, evaluating all adult LT recipients (aged 18 years or older) from 1997 – 2023. GI DNM included esophageal, stomach, small bowel, pancreatic, and colorectal cancers (CRC) occurring at least 1 year after LT. A competing risk regression model was used to assess cumulative incidence of GI DNM in relation to primary indication of LT and history of hepatocellular carcinoma (HCC) and/or cholangiocarcinoma (CCA) with death as a competing event. Multivariable Cox proportional hazards regression models were used to identify factors associated with GI DNM.
Results: A total of 137,742 patients were analyzed; median age was 55 (IQR 48 – 62) years, 72.1% were White, and 20.7% had history of HCC/CCA (Table 1). GI DNM occurred in 1,426 (1.0%) LT recipients (572 [40.1%] CRC, 462 [32.3%] pancreatic, 226 [15.8%] esophageal, 124 [8.6%] gastric, and 55 [3.8%] small bowel cancers). Median follow-up time was 6.4 (IQR 3.1 – 11.1) years. The 5-, 10-, 15-year cumulative incidence of GI DNM were highest among PSC patients (2.0, 2.8, 5.4% for PSC with HCC/CCA and 1.0, 2.3, 4.4% for PSC without HCC/CCA), followed by alcohol-associated liver disease (ALD) (1.0, 2.9, 4.5% for ALD with HCC and 0.5, 1.4, 2.3% for ALD without HCC), MASLD (1.1, 2.6, 3.6% for MASLD with HCC and 0.5, 1.2, 2.0% for MASLD without HCC), and HCV (0.6, 1.5, 2.3% for HCV with HCC and 0.3, 1.0, 1.7% for HCV without HCC) (Figure 1). In multivariate Cox regression analysis, GI DNM developed more among older patients (aHR 1.04; CI 1.03 – 1.04), those with ALD (aHR 1.27; CI 1.06 – 1.52), PSC (aHR 2.39; CI 1.91 – 2.99), prior HCC (aHR 1.35; CI 1.15 – 1.57), and less among Hispanic patients (aHR 0.76; CI 0.63 – 0.93).
Discussion: In this large retrospective study, the incidence of GI DNM varied by the liver disease etiology, and the highest rates noted in patients with PSC. Age, ALD, and a history of HCC/CCA were associated with increased risk. These findings support the need of more tailored and vigilant cancer screening strategies in LT recipients.
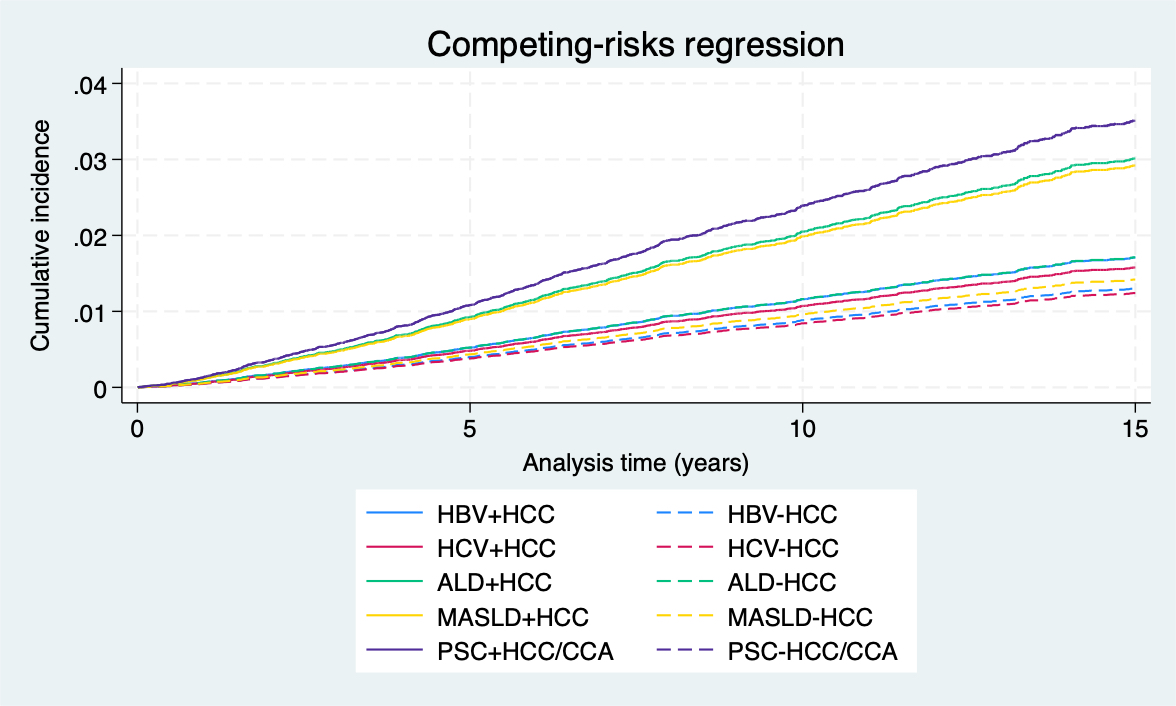
Figure: Figure 1: Cumulative incidence of GI DNM in relation to primary indication of LT and history of HCC/CCA.

Figure: Table 1: Baseline recipient characteristics
† Continuous variables presented as median and IQR; categorical variables presented as N (%)
Disclosures:
Chawin Lopimpisuth indicated no relevant financial relationships.
Alisa Likhitsup indicated no relevant financial relationships.
Chawin Lopimpisuth, MD1, Alisa Likhitsup, MD2. P3670 - <i>De Novo</i> Gastrointestinal Malignancies Among Liver Transplant Recipients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

