Tuesday Poster Session
Category: Liver
P6030 - Cirrhosis and Hepatic Involvement in Hereditary Hemorrhagic Telangiectasia
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- OA
Osama Asad, MD
University of Missouri-Kansas City
Kansas City, MO
Presenting Author(s)
Osama Asad, MD1, Mohamed Ahmed, MD2, Attiq Rehman, MD3, Zaid Al Momani, MD2, Karam Khasawneh, MD4
1University of Missouri-Kansas City, Kansas City, MO; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3University of Missouri Kansas City School of Medicine, Saint Luke's Hospital, Kansas City, MO; 4Jordan University of Science and Technology, Amman, 'Amman, Jordan
Introduction: Hereditary hemorrhagic telangiectasia (HHT) is a rare autosomal dominant vascular disorder characterized by mucocutaneous telangiectasias and visceral arteriovenous malformations (AVMs). Hepatic involvement is common, though only 8–10% develop clinical manifestations. In rare instances, hepatic AVMs may lead to progressive fibrosis and cirrhosis. We present a case of decompensated cirrhosis and portal hypertension secondary to hepatic AVMs in a patient with HHT.
Case Description/
Methods: A 55-year-old woman with a history of type 2 diabetes mellitus, asthma, and cerebral palsy, and a family history of HHT, was diagnosed with liver cirrhosis after routine laboratory testing revealed elevated liver enzymes. Hepatitis viral serologies and autoimmune workup were negative. Initially asymptomatic, she progressed over four years to decompensated cirrhosis with portal hypertension, manifesting as ascites and esophageal varices. Management included periodic paracentesis and serial esophagogastroduodenoscopies (EGDs) with band ligation. Despite intervention, varices progressed and symptoms worsened. Laboratory testing revealed elevated alkaline phosphatase and mildly elevated AST, with low iron studies. Imaging, including MRCP and CT abdomen/pelvis, confirmed a cirrhotic liver with a large hepatic artery-venous shunt and no biliary obstruction. The patient was referred to transplant hepatology and cardiology for further evaluation. Due to the AVM anatomy, she was not a candidate for transjugular intrahepatic portosystemic shunt (TIPS) and is currently being assessed for liver transplantation.
Discussion: Liver involvement in HHT may lead to serious complications such as high-output heart failure, biliary disease, and portal hypertension. While most patients remain asymptomatic, a small subset develops progressive liver disease. Management of hepatic complications is supportive and may include diuretics, band ligation, or TIPS, although anatomical variations can limit their feasibility. Liver transplantation remains the definitive treatment in cases of severe hepatic AVM-related complications. In this case, the patient’s cirrhosis and portal hypertension were attributed to intrahepatic AVMs. Due to her complex vascular anatomy, conventional therapies were inadequate, warranting transplant evaluation.
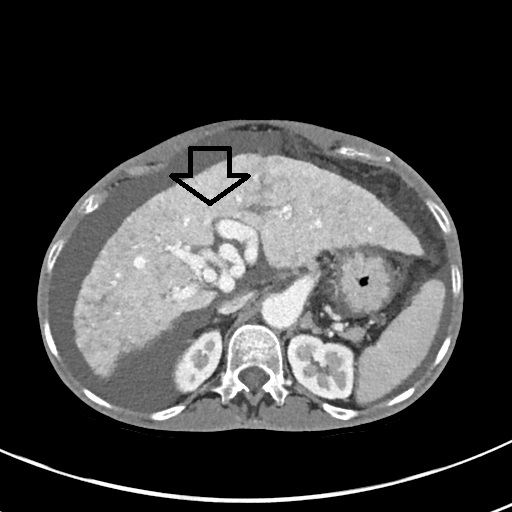
Figure: AVM malformation on CT scan
Disclosures:
Osama Asad indicated no relevant financial relationships.
Mohamed Ahmed indicated no relevant financial relationships.
Attiq Rehman indicated no relevant financial relationships.
Zaid Al Momani indicated no relevant financial relationships.
Karam Khasawneh indicated no relevant financial relationships.
Osama Asad, MD1, Mohamed Ahmed, MD2, Attiq Rehman, MD3, Zaid Al Momani, MD2, Karam Khasawneh, MD4. P6030 - Cirrhosis and Hepatic Involvement in Hereditary Hemorrhagic Telangiectasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Missouri-Kansas City, Kansas City, MO; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3University of Missouri Kansas City School of Medicine, Saint Luke's Hospital, Kansas City, MO; 4Jordan University of Science and Technology, Amman, 'Amman, Jordan
Introduction: Hereditary hemorrhagic telangiectasia (HHT) is a rare autosomal dominant vascular disorder characterized by mucocutaneous telangiectasias and visceral arteriovenous malformations (AVMs). Hepatic involvement is common, though only 8–10% develop clinical manifestations. In rare instances, hepatic AVMs may lead to progressive fibrosis and cirrhosis. We present a case of decompensated cirrhosis and portal hypertension secondary to hepatic AVMs in a patient with HHT.
Case Description/
Methods: A 55-year-old woman with a history of type 2 diabetes mellitus, asthma, and cerebral palsy, and a family history of HHT, was diagnosed with liver cirrhosis after routine laboratory testing revealed elevated liver enzymes. Hepatitis viral serologies and autoimmune workup were negative. Initially asymptomatic, she progressed over four years to decompensated cirrhosis with portal hypertension, manifesting as ascites and esophageal varices. Management included periodic paracentesis and serial esophagogastroduodenoscopies (EGDs) with band ligation. Despite intervention, varices progressed and symptoms worsened. Laboratory testing revealed elevated alkaline phosphatase and mildly elevated AST, with low iron studies. Imaging, including MRCP and CT abdomen/pelvis, confirmed a cirrhotic liver with a large hepatic artery-venous shunt and no biliary obstruction. The patient was referred to transplant hepatology and cardiology for further evaluation. Due to the AVM anatomy, she was not a candidate for transjugular intrahepatic portosystemic shunt (TIPS) and is currently being assessed for liver transplantation.
Discussion: Liver involvement in HHT may lead to serious complications such as high-output heart failure, biliary disease, and portal hypertension. While most patients remain asymptomatic, a small subset develops progressive liver disease. Management of hepatic complications is supportive and may include diuretics, band ligation, or TIPS, although anatomical variations can limit their feasibility. Liver transplantation remains the definitive treatment in cases of severe hepatic AVM-related complications. In this case, the patient’s cirrhosis and portal hypertension were attributed to intrahepatic AVMs. Due to her complex vascular anatomy, conventional therapies were inadequate, warranting transplant evaluation.
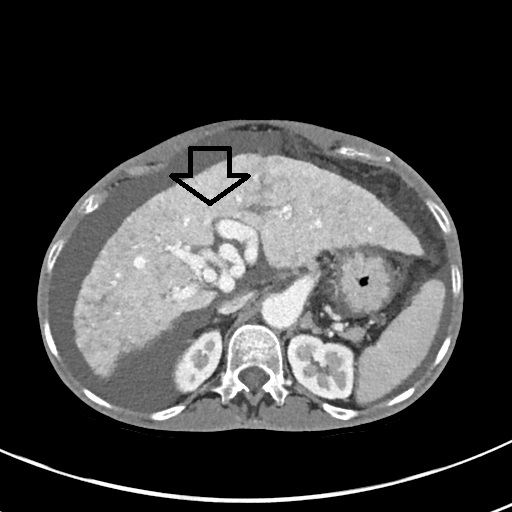
Figure: AVM malformation on CT scan
Disclosures:
Osama Asad indicated no relevant financial relationships.
Mohamed Ahmed indicated no relevant financial relationships.
Attiq Rehman indicated no relevant financial relationships.
Zaid Al Momani indicated no relevant financial relationships.
Karam Khasawneh indicated no relevant financial relationships.
Osama Asad, MD1, Mohamed Ahmed, MD2, Attiq Rehman, MD3, Zaid Al Momani, MD2, Karam Khasawneh, MD4. P6030 - Cirrhosis and Hepatic Involvement in Hereditary Hemorrhagic Telangiectasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
