Tuesday Poster Session
Category: Liver
P6029 - Double Trouble: EBV and Coronavirus HKU1 Coinfection Leading to Acute Liver Injury
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- YD
Yara Dababneh, MD (she/her/hers)
Henry Ford Hospital
Detroit, MI
Presenting Author(s)
Yara Dababneh, MD1, Stephanie Betcher, MD2, William JN. Davis, DO3, Diana Jomaa-Rteil, MD3, Humberto C.. Gonzalez, MD1
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Chicago, IL; 3Henry Ford Health, Detroit, MI
Introduction: Although it has been almost 5 years since we faced the COVID 19 pandemic, it is still surprising to see the effects of Coronavirus on patients and the phenomena associated with it.
Case Description/
Methods: 19-year-old female presented for fevers and abnormal liver enzymes. Patient had presented to an urgent care a week before her admission with acute upper respiratory symptoms and at that time all viral etiologies including COVID and Flu were negative, a few days after she went to see her primary care provider (PCP) for persistent fevers. Labs at that time were done and showed White Blood Cells (WBC) 1.8 k/uL, platelets at 94 K/uL, abnormal liver enzymes with AST 200 IU/L, ALT 174 IU/L, Total Bilirubin 3 mg/dL, Direct Bilirubin 1.7 mg/dL, ALP 271 IU/L. Right Upper Quadrant (RUQ) Ultrasound showed normal findings. She presented two days later to her PCP with persistent fevers. Repeat Liver enzymes showed worsening values with AST 397 IU/L, ALT 384 IU/L, Total Bilirubin 3.7 mg/dL, Direct Bilirubin 2.2 mg/dL, ALP 390 IU/L, WBC 2.4 k/uL, platelets 86 K/uL, Neutrophils 0.48 K/uL workup including acute viral hepatitis and EBV monospot test were negative. She was admitted thereafter and evaluated by our hepatology team. Her Liver enzymes continued to worsen peaking at AST 656 IU/L, ALT 886 IU/L, Total Bilirubin 3.9 mg/dL, Direct Bilirubin 2.5 mg/dL, ALP 550 IU/L, repeat RUQ Ultrasound showed splenomegaly up to 16cm. Broad infectious, autoimmune and toxicology labs were ordered and results were positive for Coronavirus HKU1 and EBV PCR with quantitative value of 47,000 copies/mL. The patient was managed supportively. Eventually she improved with a decrease in her liver enzymes and return of normal daily activities while avoiding contact sports. She followed up in clinic with repeat labs every week and normalization of her liver enzymes and undetected EBV PCR three weeks after.
Discussion: This case outlines two underlying etiologies that contributed to the above presentation. Although EBV is a known cause of Acute Liver Injury (ALI) with elevated Liver enzymes and splenomegaly. Coronavirus HKU1 has been reported once as a cause of acute liver injury mainly in the pediatric population as patients present with mild respiratory symptoms and acute liver injury. We wanted to stress the importance of maintaining a high index of clinical suspicion as other uncommon viral etiologies can be the underlying cause of ALI especially in cases where all common viral causes are ruled out.
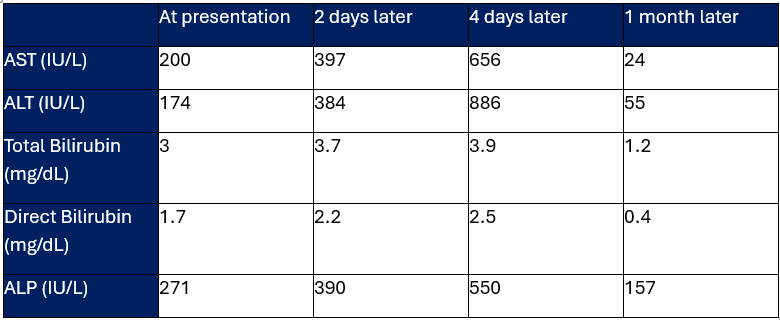
Figure: Liver enzymes trend over time.
Disclosures:
Yara Dababneh indicated no relevant financial relationships.
Stephanie Betcher indicated no relevant financial relationships.
William Davis indicated no relevant financial relationships.
Diana Jomaa-Rteil indicated no relevant financial relationships.
Humberto Gonzalez: Madrigal Pharmaceuticals – Advisor or Review Panel Member, Speakers Bureau.
Yara Dababneh, MD1, Stephanie Betcher, MD2, William JN. Davis, DO3, Diana Jomaa-Rteil, MD3, Humberto C.. Gonzalez, MD1. P6029 - Double Trouble: EBV and Coronavirus HKU1 Coinfection Leading to Acute Liver Injury, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Chicago, IL; 3Henry Ford Health, Detroit, MI
Introduction: Although it has been almost 5 years since we faced the COVID 19 pandemic, it is still surprising to see the effects of Coronavirus on patients and the phenomena associated with it.
Case Description/
Methods: 19-year-old female presented for fevers and abnormal liver enzymes. Patient had presented to an urgent care a week before her admission with acute upper respiratory symptoms and at that time all viral etiologies including COVID and Flu were negative, a few days after she went to see her primary care provider (PCP) for persistent fevers. Labs at that time were done and showed White Blood Cells (WBC) 1.8 k/uL, platelets at 94 K/uL, abnormal liver enzymes with AST 200 IU/L, ALT 174 IU/L, Total Bilirubin 3 mg/dL, Direct Bilirubin 1.7 mg/dL, ALP 271 IU/L. Right Upper Quadrant (RUQ) Ultrasound showed normal findings. She presented two days later to her PCP with persistent fevers. Repeat Liver enzymes showed worsening values with AST 397 IU/L, ALT 384 IU/L, Total Bilirubin 3.7 mg/dL, Direct Bilirubin 2.2 mg/dL, ALP 390 IU/L, WBC 2.4 k/uL, platelets 86 K/uL, Neutrophils 0.48 K/uL workup including acute viral hepatitis and EBV monospot test were negative. She was admitted thereafter and evaluated by our hepatology team. Her Liver enzymes continued to worsen peaking at AST 656 IU/L, ALT 886 IU/L, Total Bilirubin 3.9 mg/dL, Direct Bilirubin 2.5 mg/dL, ALP 550 IU/L, repeat RUQ Ultrasound showed splenomegaly up to 16cm. Broad infectious, autoimmune and toxicology labs were ordered and results were positive for Coronavirus HKU1 and EBV PCR with quantitative value of 47,000 copies/mL. The patient was managed supportively. Eventually she improved with a decrease in her liver enzymes and return of normal daily activities while avoiding contact sports. She followed up in clinic with repeat labs every week and normalization of her liver enzymes and undetected EBV PCR three weeks after.
Discussion: This case outlines two underlying etiologies that contributed to the above presentation. Although EBV is a known cause of Acute Liver Injury (ALI) with elevated Liver enzymes and splenomegaly. Coronavirus HKU1 has been reported once as a cause of acute liver injury mainly in the pediatric population as patients present with mild respiratory symptoms and acute liver injury. We wanted to stress the importance of maintaining a high index of clinical suspicion as other uncommon viral etiologies can be the underlying cause of ALI especially in cases where all common viral causes are ruled out.
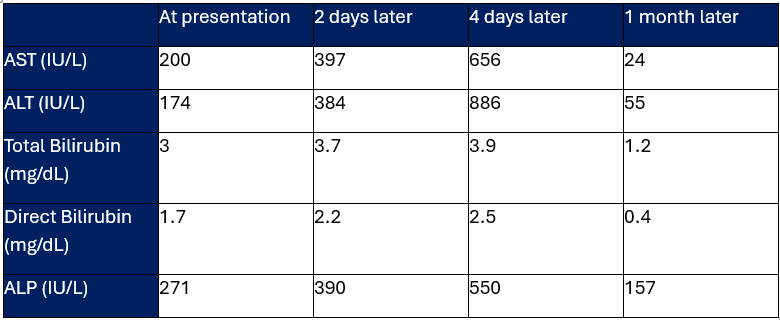
Figure: Liver enzymes trend over time.
Disclosures:
Yara Dababneh indicated no relevant financial relationships.
Stephanie Betcher indicated no relevant financial relationships.
William Davis indicated no relevant financial relationships.
Diana Jomaa-Rteil indicated no relevant financial relationships.
Humberto Gonzalez: Madrigal Pharmaceuticals – Advisor or Review Panel Member, Speakers Bureau.
Yara Dababneh, MD1, Stephanie Betcher, MD2, William JN. Davis, DO3, Diana Jomaa-Rteil, MD3, Humberto C.. Gonzalez, MD1. P6029 - Double Trouble: EBV and Coronavirus HKU1 Coinfection Leading to Acute Liver Injury, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
