Tuesday Poster Session
Category: Liver
P6114 - Hyperlocal Brewery: Cases and Comprehensive Review of the Clinical Course, Diagnosis, and Treatment of Autobrewery Syndrome
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Lynette Sequeira, MD
Johns Hopkins University School of Medicine
Baltimore, MD
Presenting Author(s)
Lynette Sequeira, MD, Divya Rayapati, MD, Natarajan Ravendhran, MD
Johns Hopkins University School of Medicine, Baltimore, MD
Introduction: Auto-brewery syndrome (ABS) is a rare condition characterized by endogenous ethanol production through the fermentation of carbohydrates by fungi or bacteria within the gastrointestinal tract, oral cavity, or urinary system. This process can result in a spectrum of symptoms associated with alcohol intoxication—including confusion, slurred speech, and imbalance—often in the absence of alcohol consumption. Triggering factors include fasting, stress, or can be idiopathic, complicating diagnosis and management. We present two cases of ABS in which patients exhibited hallmark symptoms and biochemical evidence of ethanol presence without alcohol intake, both of whom improved with antifungal treatment and lifestyle changes.
Case Description/
Methods: Patient A, a 36-year-old male with no metabolic risk factors, reported episodes of confusion and slurred speech following fasting. Despite negative brain imaging and glucose monitoring, he had persistently elevated liver enzymes, a positive phosphatidylethanol (PETH) test, and hepatic steatosis on imaging. A liver biopsy confirmed steatohepatitis with fibrosis. He was treated with two 14-day courses of fluconazole and initiated a low-carbohydrate diet, resulting in full clinical and biochemical remission, including normalization of liver enzymes, PETH levels, and resolution of steatosis on imaging (Table 1).
Patient B, a 58-year-old male, experienced episodes of brain fog and inebriation-like symptoms triggered by stress and fasting. He exhibited mild hepatic steatosis, transient liver enzyme elevation, and fungal elements on endoscopic culture. He responded favorably to three courses of fluconazole, a low-carbohydrate diet, alcohol abstinence, and probiotic use.
Discussion: These cases underscore the importance of considering ABS in patients with unexplained inebriation symptoms, particularly when traditional risk factors for liver disease are absent. While formal diagnostic criteria are not well-established, suggestive findings—such as positive PETH, abnormal liver studies, and symptom resolution following antifungal therapy—support the diagnosis. Management typically involves antifungal agents, dietary modification, and ongoing symptom surveillance (Table 2).
Increased awareness and early recognition of ABS are essential. Appropriate diagnosis and treatment may prevent progression to irreversible liver damage and significantly improve patient quality of life.
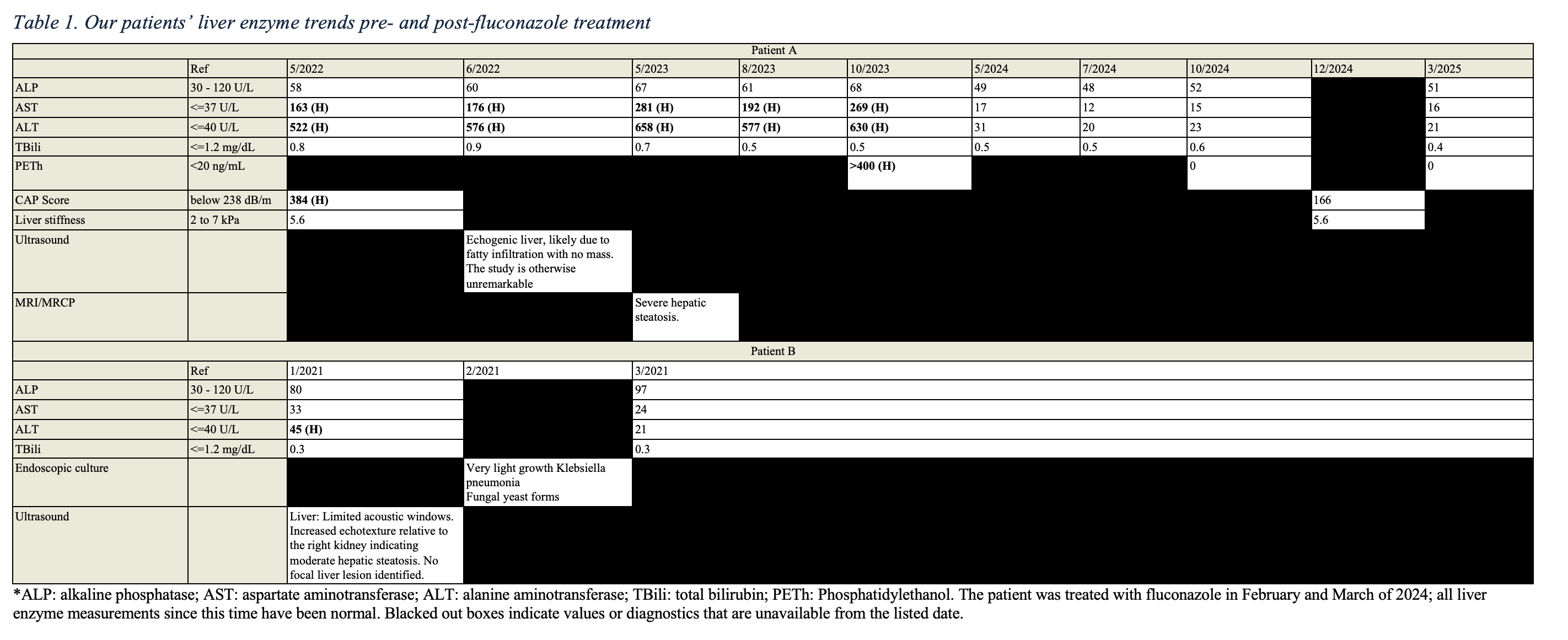
Figure: Table 1. Our patients’ liver enzyme trends pre- and post-fluconazole treatment. *ALP: alkaline phosphatase; AST: aspartate aminotransferase; ALT: alanine aminotransferase; TBili: total bilirubin; PETh: Phosphatidylethanol. Patient A was treated with fluconazole in February and March of 2024; all liver enzyme measurements since this time have been normal. Blacked out boxes indicate values or diagnostics that are unavailable from the listed date.

Figure: Table 2. Summary of prior diagnostic and treatment strategies for ABS
Disclosures:
Lynette Sequeira indicated no relevant financial relationships.
Divya Rayapati indicated no relevant financial relationships.
Natarajan Ravendhran indicated no relevant financial relationships.
Lynette Sequeira, MD, Divya Rayapati, MD, Natarajan Ravendhran, MD. P6114 - Hyperlocal Brewery: Cases and Comprehensive Review of the Clinical Course, Diagnosis, and Treatment of Autobrewery Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Johns Hopkins University School of Medicine, Baltimore, MD
Introduction: Auto-brewery syndrome (ABS) is a rare condition characterized by endogenous ethanol production through the fermentation of carbohydrates by fungi or bacteria within the gastrointestinal tract, oral cavity, or urinary system. This process can result in a spectrum of symptoms associated with alcohol intoxication—including confusion, slurred speech, and imbalance—often in the absence of alcohol consumption. Triggering factors include fasting, stress, or can be idiopathic, complicating diagnosis and management. We present two cases of ABS in which patients exhibited hallmark symptoms and biochemical evidence of ethanol presence without alcohol intake, both of whom improved with antifungal treatment and lifestyle changes.
Case Description/
Methods: Patient A, a 36-year-old male with no metabolic risk factors, reported episodes of confusion and slurred speech following fasting. Despite negative brain imaging and glucose monitoring, he had persistently elevated liver enzymes, a positive phosphatidylethanol (PETH) test, and hepatic steatosis on imaging. A liver biopsy confirmed steatohepatitis with fibrosis. He was treated with two 14-day courses of fluconazole and initiated a low-carbohydrate diet, resulting in full clinical and biochemical remission, including normalization of liver enzymes, PETH levels, and resolution of steatosis on imaging (Table 1).
Patient B, a 58-year-old male, experienced episodes of brain fog and inebriation-like symptoms triggered by stress and fasting. He exhibited mild hepatic steatosis, transient liver enzyme elevation, and fungal elements on endoscopic culture. He responded favorably to three courses of fluconazole, a low-carbohydrate diet, alcohol abstinence, and probiotic use.
Discussion: These cases underscore the importance of considering ABS in patients with unexplained inebriation symptoms, particularly when traditional risk factors for liver disease are absent. While formal diagnostic criteria are not well-established, suggestive findings—such as positive PETH, abnormal liver studies, and symptom resolution following antifungal therapy—support the diagnosis. Management typically involves antifungal agents, dietary modification, and ongoing symptom surveillance (Table 2).
Increased awareness and early recognition of ABS are essential. Appropriate diagnosis and treatment may prevent progression to irreversible liver damage and significantly improve patient quality of life.
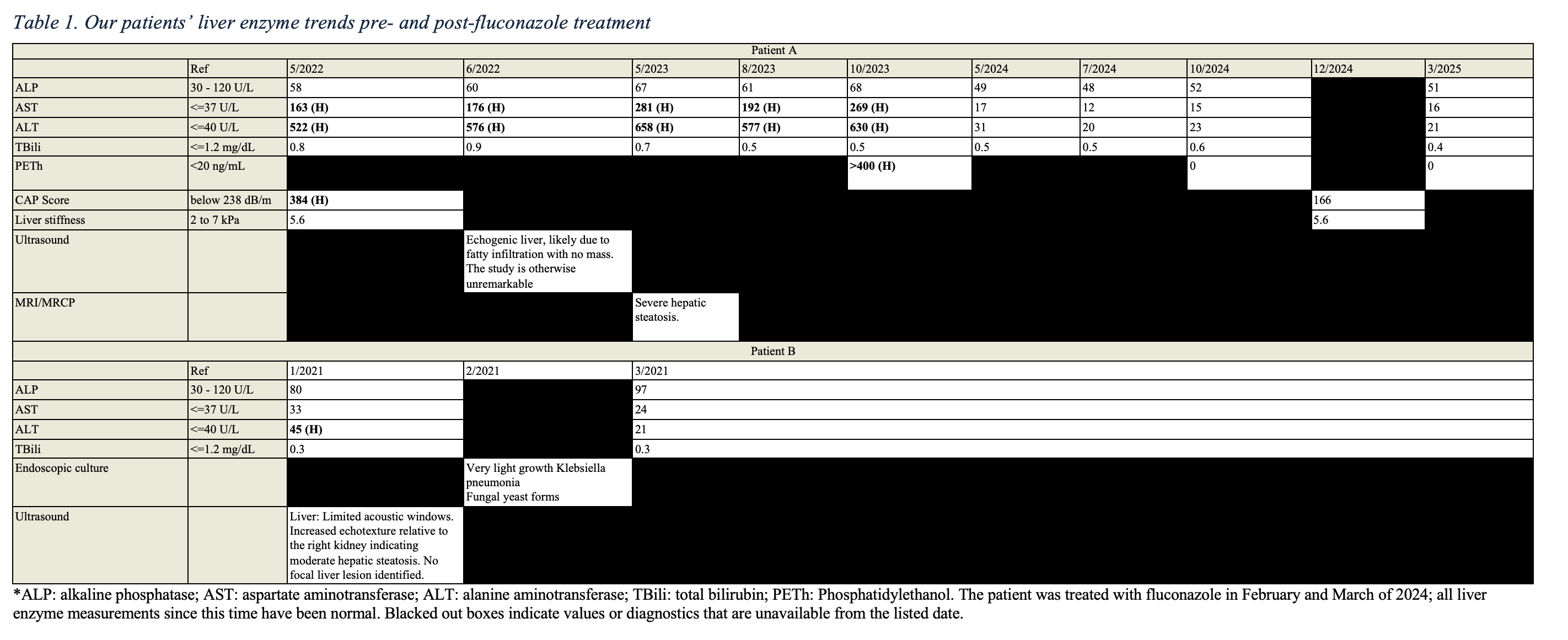
Figure: Table 1. Our patients’ liver enzyme trends pre- and post-fluconazole treatment. *ALP: alkaline phosphatase; AST: aspartate aminotransferase; ALT: alanine aminotransferase; TBili: total bilirubin; PETh: Phosphatidylethanol. Patient A was treated with fluconazole in February and March of 2024; all liver enzyme measurements since this time have been normal. Blacked out boxes indicate values or diagnostics that are unavailable from the listed date.

Figure: Table 2. Summary of prior diagnostic and treatment strategies for ABS
Disclosures:
Lynette Sequeira indicated no relevant financial relationships.
Divya Rayapati indicated no relevant financial relationships.
Natarajan Ravendhran indicated no relevant financial relationships.
Lynette Sequeira, MD, Divya Rayapati, MD, Natarajan Ravendhran, MD. P6114 - Hyperlocal Brewery: Cases and Comprehensive Review of the Clinical Course, Diagnosis, and Treatment of Autobrewery Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
